Home » Department of Pediatrics » Tay-Sachs disease
Change font: A
A
GM2 gangliosidosis (Tay-Sachs disease) is a disease with an autosomal recessive pattern of inheritance that affects the central nervous system (spinal cord, brain, and meningeal membranes). During the first six months of life, children develop normally with this disease, but then brain functions begin to suffer, and they often die before the age of 3-4 years.
The incidence rate is about 1 case per 250,000 population.
What is Tay-Sachs disease?
Tay-Sachs disease is a rare neurodegenerative disorder in which a deficiency of an enzyme (hexosaminidase A) causes the excessive accumulation of certain fats (lipids) known as gangliosides in the brain and nerve cells. This excessive accumulation of gangliosides leads to progressive dysfunction of the central nervous system. The disease belongs to the group of lysosomal storage diseases. Lysosomes are the main digestive units in cells. Enzymes in lysosomes break down or “digest” nutrients, including certain complex carbohydrates and fats. When an enzyme such as hexosaminidase A, which is needed to break down certain substances such as fats, is missing or ineffective, they accumulate in lysosomes. This is called abnormal "hoarding". When too much fat deposits accumulate in the lysosome, it becomes toxic, destroying cells and damaging surrounding tissue.
Symptoms associated with Tay-Sachs disease may include an exaggerated startle response to sudden sounds, lethargy, loss of previously acquired skills (eg, psychomotor regression), and severely decreased muscle tone (hypotonia). Infants with hypotonia may be described as “floppy.” As the disease progresses, affected infants and children may develop cherry-red spots in the middle layer of the eyes, gradual loss of vision and hearing loss, increased muscle stiffness and limited movement (spasticity), paralysis, uncontrollable electrical disturbances in the brain (epilepsy), and deterioration cognitive processes (dementia). The classic form of Tay-Sachs disease occurs in infancy. This is the most common form and is usually fatal in early childhood. There are also juvenile and adult forms of Tay-Sachs disease, but they are rare. Children with the juvenile form, also called the subacute form, develop symptoms later than children with the infantile form and usually survive into later childhood or adolescence. The adult form, also called late-onset Tay-Sachs disease, can occur any time from adolescence to the mid-30s. Symptoms and severity may vary from one person to another. Some people may be between the juvenile and adult forms.
Tay-Sachs disease is transmitted in an autosomal recessive manner. The disease results from changes (mutations) in a gene known as the HEXA gene, which regulates the production of the enzyme hexosaminidase A. The HEXA gene is found on the long arm (q) of chromosome 15 (15q23-q24). There is no cure for Tay-Sachs disease, and treatment is aimed at relieving specific symptoms that occur.
Another name for Tay-Sachs disease is GM2 gangliosidosis type 1. There are two other related diseases called Sandhoff disease and hexosaminidase activator deficiency, which are indistinguishable from Tay-Sachs disease based on symptoms and can only be differentiated by testing for underlying causes. These two disorders also cause decreased hexosaminidase activity, but are caused by changes in different genes. Collectively, these three disorders are known as GM2 gangliosidoses.
Classification
Tay-Sachs disease (amaurotic idiocy) comes in three forms:
- childhood – manifests itself at six months of age and is accompanied by a progressive decline in mental and physical capabilities;
- teenage – motor-cognitive disorders, dysarthria, dysphagia, ataxia, spasticity appear;
- adult – is a rare form, manifests itself at 25–30 years of age and is accompanied by a progressive decline in neurological functions.
In the first form of the disease, death occurs at 3–4 years. In the adolescent form of the disease, death is guaranteed at 15–16 years of age.
Signs and symptoms
Tay-Sachs disease is divided into the classic or infantile form, the juvenile form, and the adult or late-onset form. In people with infantile Tay-Sachs disease, symptoms usually first appear between three and five months of age. For people with late onset, symptoms may appear any time from their teens to their mid-30s.
— Infantile form of the disease.
The childhood form of Tay-Sachs disease is characterized by almost complete absence of activity of the enzyme hexosaminidase A. The disorder often progresses rapidly, leading to significant deterioration in mental and physical condition.
Babies may appear completely unaffected at birth. Initial symptoms, which usually develop between 3 and 6 months, may include mild muscle weakness, muscle twitching (myoclonic jerks), and an exaggerated startle response, such as to a sudden or unexpected sound. The startle response may be due in part to increased sensitivity to sound (acoustic hypersensitivity).
Symptoms
Regardless of the form of the disease, several main symptoms appear: dysphagia, ataxia, loss of cognitive function, muscle atrophy. If a child under one year of age reacts sharply to sharp sounds, gains weight poorly and cannot relax his muscles, parents should show him to specialists - this is how Tay-Sachs disease begins in infants. Symptoms become increasingly severe. After 6 months, motor activity decreases, the baby loses the ability to sit independently and change position. Blindness gradually develops, hearing decreases, muscles atrophy and complete paralysis of the body develops.
In the juvenile form, in addition to the main symptoms, dysarthria (decreased speech clarity), spasticity, and impaired coordination of movements are observed. There is a gradual loss of cognitive functions - a decrease in memory, attention, and performance. Dementia develops. In the later stages of the disease, seizures appear.
The first symptoms of the adult form of the disease are difficulty swallowing, loss of coordination and dysarthria. Mental disorders similar to the symptoms of schizophrenia (visual and auditory hallucinations, apathy, decreased emotionality) often appear. Without treatment, cognitive function deteriorates. Only for this form of the disease there is an effective treatment that can stop Tay-Sachs disease. The National Guide to Neonatology says that effective methods for diagnosing the adult form of the disease appeared only in the 70s; before that, the disease was considered a childhood disease.
Causes
Tay-Sachs disease is caused by a change (mutation) in the gene encoding the alpha subunit of hexoamindase A (HEXA). Genes provide instructions for making proteins, which play a critical role in many body functions. When a gene mutation occurs, the protein product may be faulty, ineffective, or missing. Depending on the protein's functions, it can affect many organ systems in the body, including the brain.
The HEXA gene regulates the production of the enzyme hexosaminidase A. More than 80 different mutations of the HEXA gene have been identified in people with this disease. Inheriting two mutated copies of the HEXA gene (homozygous) causes a deficiency of the enzyme hexosaminidase A, which is needed to break down a fatty substance (lipid) known as GM2 ganglioside in the body's cells. Failure to break down GM2 ganglioside leads to its abnormal accumulation in the brain and nerve cells, ultimately leading to progressive deterioration of the central nervous system.
In childhood Tay-Sachs disease, there is an almost complete absence of hexosaminidase A. In late-onset Tay-Sachs disease, there is a deficiency in the activity of the enzyme hexosaminidase A. Because of some enzyme activity, the disease is less severe and progresses much more slowly than childhood Tay-Sachs disease. The exact amount of enzyme activity in late-onset Tay-Sachs disease varies greatly from person to person. Consequently, the age of onset, severity, specific symptoms and rate of progression of late-onset disease also vary greatly from one person to another.
Changes in the HEXA gene, which causes Tay-Sachs disease, are inherited in an autosomal recessive manner. Most genetic diseases are determined by the status of two copies of a gene, one from the father and one from the mother. Recessive genetic disorders occur when a person inherits two copies of an abnormal gene for the same trait, one from each parent. If a person inherits one normal gene and one disease gene, he will be a carrier of the disease, but usually asymptomatic. The risk for two carrier parents of passing on the altered gene and having an affected child is 25% in each pregnancy. The risk of having a child who is a carrier like the parents is 50% with each pregnancy. The chance that a child will receive normal genes from both parents is 25%. The risk is the same for men and women.
Researchers have determined that the Tay-Sachs disease gene is located on the long arm (q) of chromosome 15 (15q23-q24). Chromosomes are located in the nucleus of human cells and carry the genetic information of each person. Cells in the human body usually have 46 chromosomes. Pairs of human chromosomes, numbered 1 to 22, are called autosomes, and the sex chromosomes are designated X and Y. Males have one X and one Y chromosome, and females have two X chromosomes. Each chromosome has a short arm, designated "p", and a long arm, designated "q". Chromosomes are further divided into many numbered bands. For example, "chromosome 11p13" refers to band 13 on the short arm of chromosome 11. The numbered bands indicate the location of the thousands of genes present on each chromosome.
Causes of the disease
For a long time, doctors could not answer the question of what causes Tay-Sachs disease. The causes of the pathology became known only in the middle of the twentieth century, when ideas about genetics were formed. Studies have shown that the disease develops as a result of a mutation in the HEXA gene, which is located on the 15th chromosome. The disease is a type of GM2 gangliosidosis, a genetic pathology associated with a deficiency or decreased activity of hexosaminidase. Amaurotic idiocy occurs as a result of a decrease in the activity of hexazaminidase A or a deficiency of this enzyme.
The disease is transmitted in an autosomal recessive manner, therefore if a person has a healthy HEXA gene in his genotype, then he does not develop Tay-Sachs disease. The genetics of the disease is similar to the inheritance of such pathologies as Gaucher disease, Urbach-Wiethe disease, Dabin-Johnson syndrome: if both parents were carriers of the mutated gene, the probability of having a sick child is 0.25%, if both mother and father were sick, then both In children, the disease manifests itself in almost 100% of cases.
Affected Populations
Tay-Sachs disease affects men and women equally. The disease is more common among Jews of Ashkenazi origin, that is, people from Eastern or Central Europe. About one in 30 Ashkenazi Jews carries the altered Tay-Sachs disease gene. Additionally, one in every 300 people of non-Ashkenazi Jewish background is a carrier.
In this specific Jewish population, about 1 in 3,600 live births are affected. The disease is also seen in some people of Italian, Irish Catholic, and non-Jewish French-Canadian ancestry, especially those living in the Cajun community of Louisiana and southeastern Quebec. In the general population, the rate of transmission of the altered gene is approximately 1 in 250-300 people.
Prenatal diagnosis
Modern research makes it possible to determine early in pregnancy whether the child has inherited the mutant HEXA gene from its parents. If both parents are carriers of the disease, it is recommended to perform a chorionic villus biopsy. This is one of the most common prenatal diagnostic procedures, the purpose of which is to identify genetic abnormalities in the fetus. It is carried out at 10-14 weeks of pregnancy. Amniocentesis also gives a clear idea of whether the child is a carrier of the mutated HEXA gene. These procedures have a risk of miscarriage of less than 1%.
In the case of artificial insemination, genetic abnormalities of the fetus can be detected even before it is implanted in the uterus. For this purpose, preimplantation genetic diagnosis is performed, an analogue of prenatal diagnosis. Its main advantage is that the procedure is non-invasive and absolutely safe. It is possible to select only healthy embryos for implantation, thereby reducing the risk of having a child with Tay-Sachs disease to almost zero.
Diagnostics
The diagnosis of Tay-Sachs disease can be confirmed by a thorough clinical assessment and specialized tests, such as blood tests that measure the level of hexosaminidase A in the body. Hexosaminidase A is reduced in patients with Tay-Sachs disease and is absent or almost absent in infants.
Molecular genetic testing can confirm the diagnosis of Tay-Sachs disease. Molecular genetic testing can detect mutations in the HEXA gene, which are known to cause the disorder but are only available as a diagnostic service in specialized laboratories.
In some cases, it is possible that the diagnosis may be suspected before birth (prenatally) based on specialized tests such as amniocentesis and chorionic villus sampling (CVS). During amniocentesis, a sample of the fluid surrounding the developing fetus is removed, while CVS involves removing tissue samples from part of the placenta. These samples are studied to determine whether hexosaminidase A is present or, as in people with Tay-Sachs disease, absent or present at significantly low levels. This is called an enzyme assay. Prenatal diagnosis is also possible through molecular genetic testing of tissue samples obtained by IVS or amniocentesis if a specific disease-causing mutation in the HEXA gene is known in the family.
Blood tests can determine whether people are carriers of the disease (that is, whether they have one copy of the disease gene). Relatives of people with Tay-Sachs disease should be tested to determine whether they are carriers of the disease gene. Couples who are planning to have a child and are of any Jewish background (not just Ashkenazi) are encouraged to undergo carrier testing before becoming pregnant.
Establishing diagnosis
Doctors are not always able to make the correct diagnosis when it comes to such a rare pathology as Tay-Sachs disease. The symptoms, genetics and treatment of the disease are being actively studied by specialists. Regardless of the form of the disease, there are several diagnostic procedures that are performed if its presence is suspected. One of them is the determination of the activity of the enzyme hexosaminidase in blood serum, leukocytes or fibroblasts. In patients with Tay-Sachs disease, the activity of hexosaminidase B is always below normal, the enzyme hexosaminidase A is practically absent or its activity is significantly below normal.
Another important diagnostic criterion is the presence of a bright red spot on the cornea of the eye, which can be easily noticed by a therapist or ophthalmologist using an ophthalmoscope. A red spot on the cornea was found in all patients, regardless of age.
Unlike other lysosomal storage diseases (Gaucher disease, Standhoff syndrome, Niemann-Pick disease), Tay-Sachs disease does not cause enlargement of the liver and spleen (hepatosplenomegaly).
Standard Treatments
There is no specific treatment for Tay-Sachs disease. Treatment is aimed at addressing the specific symptoms that occur in each person. Treatment may require the coordinated efforts of a team of specialists. Pediatricians, neurologists, speech therapists, specialists who evaluate and treat hearing problems (audiologists), eye specialists, and other health care providers may need to systematically and comprehensively plan treatment for an affected child. Genetic counseling can be helpful for survivors and their families. Psychosocial support is recommended for the whole family.
Because of the potential for feeding difficulties, infants should be monitored for nutritional status and proper hydration. Nutritional support and supplements may be required, and sometimes a feeding tube may need to be inserted. In addition to nutritional support, a feeding tube may be needed to prevent food, liquid, or other foreign substances from accidentally entering the lungs (aspiration).
Anticonvulsants may be used to treat seizures associated with Tay-Sachs disease, but not in all patients. In addition, a person's type and frequency of attacks may change, requiring a change in the type or dosage of medication.
Once a quarter
According to the drug's developers, it is too early to judge its clinical effectiveness, but it is expected that the effects of one injection will last for three months after administration of the drug. This is due to the relatively low ability of the cells to divide, since they are planned to be taken from adult donors.
But at the same time, the use of these biomaterials will not carry additional risks associated with the occurrence of tumors, into which “earlier” embryonic stem cells can degenerate.
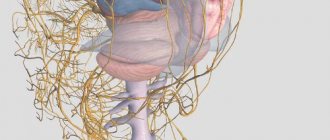
Photo: neurology.org
MRI of the brain of a child with Tay-Sachs disease
Currently, scientists are preparing to conduct a clinical trial, which should start at the Scientific and Clinical Center for Precision and Regenerative Medicine of the Kazan Federal University.
Diabetes: why the number of children suffering from diabetes is growing
Experts note that type 2 diabetes, characteristic of adults, is noticeably younger
“This is not the first attempt to create a cure for Tay-Sachs disease. In particular, clinical trials of the drug Zavesca were previously conducted for this purpose, which did not bring a positive result,” noted Stanislav Otstavnov, deputy head of the laboratory for analysis of public health indicators and digitalization of healthcare at the Moscow Institute of Physics and Technology. “If the Russian development shows its effectiveness, its use may indeed become the only chance for such patients.
According to the expert, the work of scientists from KFU looks extremely promising and their research needs to be further supported.
Forecast
Tay-Sachs disease is a progressive neurodegenerative disease.
- The classic infantile form is usually fatal by 2–3 years of age. Death usually occurs due to intercurrent infection.
- In the juvenile form, death usually occurs at the age of 10-15 years; preceded by several years of a vegetative state with decerebrate rigidity. Death usually occurs due to infection.
- In the adult form, most patients have a normal life expectancy.
Treatment
There are currently no drugs to cure Tay-Sachs disease. The symptoms and treatment of the disease are still the subject of scientific research.
The infant form of Tay-Sachs disease is the most dangerous. If a sick child cannot swallow on his own, it is recommended to resort to artificial nutrition; it is impossible to restore physical skills. There are no drugs that can stop or reverse the development of the disease, despite all the efforts of scientists. Sick babies, even if they receive the best care, rarely survive past the age of four.
In the juvenile form of the disease, it is important that the child is constantly under medical supervision. Following the instructions of a specialist and undergoing all necessary medical procedures helps to extend the life of a sick child to 12-16 years.
The adult form of the disease progresses more slowly than others and is often treatable. For mental disorders, patients are prescribed lithium or cesium chloride. Clinical trials have shown that pyrimethamine can significantly slow down, and in rare cases completely stop, the progression of the disease by increasing the activity of hexosaminidase B.