Symptoms of damage to the hypoglossal nerve
With neuropathy of the hypoglossal nerve, weakness of the tongue appears when speaking and difficulty swallowing. As the disease progresses, tongue weakness increases. Depending on the level of nerve damage, central or peripheral paresis develops. Peripheral damage occurs when the nucleus of the hypoglossal nerve, as well as the nerve fibers emanating from it, is damaged. Hypotonia of the tongue muscles on the affected side is noted, the surface of the tongue becomes wrinkled and uneven; muscle atrophy gradually appears in the tongue. A distinctive feature is fibrillary twitching in the muscles of the tongue. The tongue deviates in the direction of the lesion. Damage to the nerve on both sides is more severe (20%) - glossoplegia (immobility of the tongue) and speech impairment in the form of dysarthria occur.
| Peripheral type lesion of the left hypoglossal nerve | Damage to the left hypoglossal nerve of the central type |
Causes
Damage to the hypoglossal nerve is more often diagnosed in older men. In many cases, the cause is smoking. In addition to bad habits, the development of the disease is facilitated by:
- hypothermia of the ganglia;
- prolonged course of oral pathologies (stomatitis, gingivitis and others);
- tuberculosis;
- syphilis;
- extensive sepsis;
- chronic alcoholism;
- operations in the oral cavity;
- cysts in the mouth;
- vitamin B deficiency;
- inflammation of the submandibular lymph nodes.
Disturbance of the innervation of the tongue is characteristic of a number of rarer pathologies:
- amyotrophic lateral sclerosis;
- brain tumors;
- bulbar palsy;
- cerebrovascular accidents;
- vascular atherosclerosis.
In addition, neuritis and paralysis of the hypoglossal nerve occur as a result of acute intoxication of the body caused by exposure to heavy metals, tonsil injuries, compression of adjacent muscle fibers, hypovitaminosis, as well as endocrine pathologies and allergic reactions.
Treatment of hypoglossal nerve damage
- Anticholinesterase drugs, B vitamins.
- Oral hygiene.
- Treatment of the underlying disease.
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist.
Essential drugs
There are contraindications. Specialist consultation is required.
- Prozerin (inhibitor of acetylcholinesterase and pseudocholinesterase). Dosage regimen: orally for adults, 10-15 mg 2-3 times a day; subcutaneously - 1-2 mg 1-2 times a day.
- Milgamma (B complex of vitamins). Dosage regimen: therapy begins with 2 ml intramuscularly 1 time per day for 5-10 days. Maintenance therapy - 2 ml IM two or three times a week.
Drug therapy
Treatment of the mylohyoid nerve is carried out in two directions.
The first option involves receiving:
- anti-tuberculosis drugs;
- vitamins B12 for anemia;
- antibacterial medicines for sore throats and other bacterial infections.
Tuberculosis treatment is carried out only in specialized dispensaries. If necessary, the treatment regimen is supplemented:
- medications whose action is aimed at improving blood circulation;
- drugs that improve tissue metabolism;
- adrenergic blockers;
- ganglion blockers;
- blockers of the cholinergic system.
The main course of treatment is accompanied by symptomatic therapy. Drugs are used to eliminate the symptoms characteristic of the disease. Non-steroidal anti-inflammatory drugs are mainly prescribed: Baralgin, Ketanov or Ketorolac. In addition, diuretics and antispasmodics are used. If absolutely necessary, to eliminate pain caused by muscle spasms, tricyclic antidepressants are recommended instead of these medications.
Doctors also prescribe medications that normalize the patient’s condition in case of endocrine pathologies.
Recommendations
A consultation with a neurologist and magnetic resonance imaging of the brain are recommended.
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| Doctor of Medical Sciences, Head of the Department of Russian State Medical University, Professor, Academician of the Russian Academy of Medical Sciences Gusev E.I. | |
| • | Leading specialists and institutions for the treatment of this disease in the world: |
| G. AVANZINI, Italy. |
Symptoms
The main symptom of the problem is pain that starts at the root of the tongue and gradually affects the tonsils, soft palate and ear structures. In some cases, symptoms may appear in the eye area, lower jaw or neck. The attacks always appear only on the right or left side of the face.
The duration of the pain symptom is from 1 to 3 minutes. It can occur when eating foods that burn the tongue, talking, or yawning. People suffering from the problem often sleep on one - healthy side.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
Lying on the affected side, the person has to swallow saliva and experience bouts of pain. In addition, patients note dry mouth, and after the pain symptoms disappear, increased salivation.
Some patients experience the following symptoms during attacks:
- weakness;
- darkness in the eyes;
- decrease in pressure;
- loss of consciousness.
These manifestations of pathology are associated with inflammation of the branch of the glossopharyngeal nerve. This condition leads to inhibition of the vasomotor center.
The pathology is characterized by periods of exacerbation and remission. The duration of the last period can be 1 year or more. As the problem progresses, the period of remission becomes shorter and shorter, and the pain becomes more intense and more frequent. Sometimes the pain is so acute that the patient begins to scream from unbearable spasms.
People whose glossopharyngeal neuralgia has become chronic notice symptoms constantly. Their intensity increases when swallowing food or talking.
In such patients, there is numbness in areas that are innervated by the glossopharyngeal nerve - tonsils, pharynx, soft palate, a decrease in taste sensations, and a decrease in the amount of saliva produced. In advanced stages of the disease, patients find it difficult to chew and swallow food.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 0 | 0.3 | 0.5 | 0.8 | 0.8 | 0 | 0 | 0 | 0.3 | 0.5 | 0.8 | 0.8 |
Kinds
In neurology, there are 2 forms - primary (idiopathic) and secondary (symptomatic).
- Primary
It is impossible to say definitely for what reasons idiopathic neuralgia of the glossopharyngeal nerve develops. There are only assumptions, but they require scientific justification and evidence. According to one of them, genetic predisposition is to blame.
- Secondary
Unlike the idiopathic form, the symptomatic form develops against the background of traumatic brain injury, tumor or infectious processes. Secondary is much more common than primary and has more pronounced symptoms.
Differential diagnosis
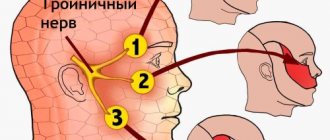
Some diseases occur with symptoms similar to those of glossopharyngeal neuralgia. In each case when a patient presents with such symptoms, the doctor conducts a thorough differential diagnosis, because the nature of these pathologies is different, which means that the treatment has its own characteristics. So, pain attacks in the facial area are accompanied by the following diseases:
- trigeminal neuralgia (much more common than others);
- ganglionitis (inflammation of the nerve ganglion) of the pterygopalatine ganglion;
- neuralgia of the ear ganglion;
- various natures of glossalgia (pain in the tongue);
- Oppenheim syndrome;
- neoplasms in the pharynx;
- retropharyngeal abscess.
Treatment
Treatment of glossopharyngeal neuralgia is prescribed primarily by a neurologist and is predominantly conservative.
Medications
The primary goal of treatment is to relieve pain paroxysm. For this purpose, local anesthetics (lidocaine hydrochloride or dicaine) are used. They lubricate the base of the tongue and the oral cavity during an attack. They relieve the condition for quite a long time. If they are ineffective, an injection of a 2% novocaine solution is given.
Along the way, various medications are prescribed for treatment:
- non-narcotic analgesics;
- anticonvulsants;
- sedatives, hypnotics;
- antidepressants and neuroleptics;
- vitamins: primarily thiamine, as well as multivitamins;
- immunomodulators: Immunal, ATP (sodium adenosine triphosphate), FiBS, Echinacea tincture, ginseng preparations.
Independent use of drugs for the treatment of glossopharyngeal neuralgia is excluded.
Physiotherapy
Physiotherapeutic techniques effectively relieve pain, reduce the frequency of attacks, activating local blood flow in the affected area. Usually with this diagnosis the following are prescribed:
- diadynamic therapy - pulsed electric current therapy;
- SMT-physiotherapy (amplipulse therapy) - exposure to sinusoidal currents;
- galvanization - treatment with continuous electric current of low strength and minimal voltage;
- ultrasound;
- electrophoresis;
- magnetic therapy;
- laser puncture;
- massage of the cervical-collar region.
Physiotherapeutic treatment is carried out during the period of exacerbation of the disease.
Folk remedies
A neurologist may advise supplementing the main course of treatment with folk remedies. Help relieve attacks of pain:
- decoction of willow bark (drink orally);
- freshly squeezed juice from black radish or horseradish (rub into the root of the tongue);
- infusion of valerian root with the addition of rue leaves (drink orally);
- applications made from a decoction of eucalyptus leaves and honey;
- applications made from fresh potatoes, honey and horseradish.
Surgery is possible if glossopharyngeal neuralgia has developed due to nerve compression. The main goal is to remove what is causing pressure (tumor, osteophyte, hypertrophied styloid process).
It takes quite a long time to treat glossopharyngeal neuralgia, often for several years. If all medical recommendations are followed, the prognosis is favorable - recovery without consequences. However, doctors do not give any guarantee that the attacks will not return under the influence of provoking factors.
Anatomy and function of the nerve
As mentioned above, the term “glossopharyngeal nerve” (in Latin – nervus glossopharyngeus) refers to the IX pair of cranial nerves. There are two of them, left and right. Each nerve consists of motor, sensory and parasympathetic fibers, which originate in the nuclei of the medulla oblongata.
- Its motor fibers provide movement of the stylopharyngeal muscle, which elevates the pharynx.
- Sensitive fibers extend to the mucous membrane of the tonsils, pharynx, soft palate, tympanic cavity, auditory tube and tongue and provide sensitivity to these areas. Its taste fibers, being a type of sensory fibers, are responsible for the taste sensations of the posterior third of the tongue and the epiglottis.
- Together, the sensory and motor fibers of the glossopharyngeal nerve form the reflex arcs of the pharyngeal and palatal reflexes.
- Parasympathetic autonomic fibers of this nerve regulate the functions of the parotid gland (responsible for salivation).
It is important to know that the glossopharyngeal nerve passes in close proximity to the vagus nerve; therefore, in many cases, their combined lesion is determined.