Shingles or herpes zoster is a disease characterized by skin signs, infectious manifestations, and disorders of the central and peripheral nervous system. The disease is caused by a certain type of virus, which is also the causative agent of a well-known childhood disease - chickenpox (varicella). The danger to humans is not so much the disease itself as the complications and consequences of herpes zoster that develop after it.
Who develops complications and when?
Hidden asymptomatic carriage of the virus that causes herpes zoster in adults is observed in 15% of the population of the former CIS countries. After chickenpox in childhood, the virus goes into a dormant form and continues to persist in the nerve ganglia of various nerves.
After a long time, when a person’s immunity decreases due to natural (age) or acquired causes, herpes reactivates and causes herpes zoster. This is a syndrome that is accompanied by pain and a characteristic rash (vesicles on reddened skin).
Those at risk of contracting herpes zoster and developing severe complications include:
- People over 50 years of age who had chickenpox in childhood. At a certain age, this category of people experiences a natural physiological decline in immunity.
- Patients of any age who have been diagnosed with HIV infection. HIV is a disease that is accompanied by suppression of the immune system. Herpes zoster in young and middle-aged people is considered a marker of HIV.
- In women with severe complicated pregnancies. During pregnancy, moderate natural immunosuppression occurs, hormonal levels change and the herpes virus is easily reactivated.
- Patients with decompensated and oncological diseases.
- People receiving immunosuppressive therapy (cytostatics, etc.).
Skin care in areas affected by herpes zoster
Treatment is not limited to taking medications. To ease the intensity of pain, eliminate unbearable itching and burning, complete care is necessary.
Some recommendations on what to do for herpetic rashes:
- Treat the problem area affected by shingles daily with soap and water;
- It is recommended to wear loose, comfortable clothes, since the dermis, where the rash is localized, is sensitive to friction;
- you can cover the problem area with an elastic bandage after applying a sterile napkin to the wound area;
- Cold compresses for shingles eliminate itching and have an analgesic effect.
External care along with proper therapy will eliminate the painful syndrome and achieve long-term remission after recovery. Postherpetic neuralgia requires a special approach, as it is accompanied by unpleasant symptoms.
Complex therapy for herpes zoster is a complex and lengthy process. With inadequate treatment, quite severe complications and disability may develop. If inflammation affects the organs of hearing or vision, partial loss of their functions is possible. Therefore, at the first signs of herpes, you should consult a doctor.
What are the possible consequences of herpes zoster?
With adequate timely treatment, the incidence of complications of herpes zoster is low. The state of the immune system and the presence of concomitant diseases play a major role in their development.
Death as a complication of herpes zoster occurs in 1–2% of patients. These are cases when the infection causes generalized failure of all organs and systems.
The main possible complications of the disease:
- postherpetic neuralgia;
- polyneuritis of the cranial nerves;
- Ramsay Hunt syndrome;
- meningitis or meningoencephalitis;
- cerebellite;
- vasculopathy;
- myelopathy;
- herpes on the eyes;
- other rare complications.
All these complications after shingles will be described in more detail below.
Postherpetic neuralgia
This is the most common complication of herpes zoster. The disease does not pose a threat to human life, but is accompanied by excruciating pain attacks.
Predisposing factors for the development of neuralgia after herpes zoster:
- senile and old age;
- late start of taking antiviral drugs;
- severe pain during illness. The stronger the pain attacks during herpes zoster, the greater the likelihood of developing neuralgia in the future;
- location and extent of the rash. With massive lesions in the torso area, the likelihood of developing this complication increases.
With postherpetic neuralgia, pain persists after the rash on the body or face disappears. Such pain may remain for several years after the infection.
Neuralgic attacks can be constant or episodic. They occur independently or in response to an external stimulus (temperature, mechanical touch).
Pain impulses spread along the nerve where there were previously rashes. Externally, the skin remains unchanged. In addition to pain, patients complain of tingling, numbness, and discomfort in the affected area.
Prevention of this complication of herpes is the timely initiation of treatment for herpes zoster. To eliminate pain, different groups of drugs are used: anticonvulsants, analgesics, antidepressants, etc.
Polyneuritis of the cranial nerves
Among this group of consequences of herpes zoster, the greatest problems for the patient are:
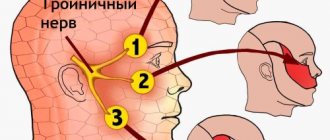
- Neuralgia of the cranial nerves. With this lesion, both the motor and sensory functions of the nerves are preserved. The disease is accompanied by excruciating pain attacks that last for years. When the trigeminal nerve is damaged, pain is provoked by touching the face, eating, and wind. With neuralgia of the glossopharyngeal nerve, taste perception is disrupted, the pain is localized in the area of the tonsils, the root of the tongue, and intensifies during the act of swallowing.
- Ganglionitis of the facial nerve (Hunt's neuralgia). It is characterized by pain in the ear canal, as well as paresis of the facial and other muscles that this nerve innervates. In addition to movement disorders, patients complain of numbness in the affected area of the face. With timely treatment, the prognosis is favorable; in rare cases, symptoms persist for a long time.
- Ganglionitis of the gasserian (trigeminal nerve) ganglion. One of the most unpleasant complications. It occurs with severe excruciating pain in the facial area, which is poorly relieved by taking analgesics. Half of the face on the affected side is swollen, red, and body temperature may rise. Painful attacks are most pronounced at the exit points of the trigeminal nerve on the face: above and below the eyebrows, in the upper jaw and at the corners of the mouth.
Ramsay Hunt syndrome
This syndrome includes damage to the facial and vestibulocochlear nerves in various variations. The disease begins acutely, the patient is concerned about the weakness of the facial muscles, which will subsequently lead to its asymmetry. The face warps in the healthy direction, the nasolabial fold is smoothed out.
The resulting pain spreads to the ear canal, back of the head and neck. There is a change in sensitivity in the ear area: from numbness to increased reactivity.
When the auditory nerve is involved in the pathological process, there is a decrease in hearing or deafness on the affected side, ringing and noise in the ears. If the vestibular part of the nerve is affected, then loss of coordination, dizziness and involuntary eye movements (nystagmus) occur.
Painful sensations may be accompanied by autonomic symptoms. The patient begins to swell, lacrimate, blood vessels protrude, and the skin of the face turns red.
The prognosis for treatment is favorable, but there are exceptions. In the absence of therapy, the disease causes a decrease in working capacity and social activity, depression develops, and cases of suicide occur.
Eye disorders
In practice, there are various ophthalmological disorders (herpes on the eyes) of an inflammatory nature, as a consequence of herpes zoster. Damage occurs when the eyeball and nearby structures are involved in the process:
- Herpetic conjunctivitis. Typical symptoms: eyes become red and swollen, vision deteriorates, tears flow profusely.
- Uveitis. The retina swells and there is a pronounced deterioration in vision.
- Herpetic keratitis. Clouding of the cornea occurs and vision decreases.
Meningitis or meningoencephalitis
Involvement of the membranes and substance of the brain in the process leads to severe disorders and is observed when herpes zoster is localized in the back of the head, face or neck.
Herpetic encephalitis (irritation of the brain substance) is characterized by the following symptoms:
- heat;
- convulsive syndrome;
- nausea, vomiting;
- delusions, hallucinations;
- impaired coordination, speech, writing;
- loss of consciousness: stupor, coma, etc.
In addition, paresis or paralysis of the limbs may occur. With paresis of the lower part of the body, there is a dysfunction of the pelvic organs (urinary incontinence, involuntary defecation).
A complication of herpes zoster can be swelling of the medulla oblongata and its wedging into the foramen magnum. The centers of breathing and heartbeat are located there, so this condition inevitably leads to death in a matter of minutes.
Complex therapy, pain relief
A patient suffering from a neuralgic disorder must be treated with painkillers. Doctors do not recommend enduring pain steadfastly - this can provoke an increased reaction and the development of a chronic syndrome.
Painkillers should be taken until the discomfort disappears. To relieve the syndrome, the following groups of drugs are prescribed:
- NPS – “Ketorolac”, the drug “Aspirin”, the drug “Ketorolac”, “Ibuprofen”.
- Antidepressants (tricyclic) - Clomipramine, medication Imizin.
- Anticonvulsant medications - Pregabalin or Gabapentin.
- Blockades using novocaine, electrical stimulation of injured nerves.
- Potent analgesics that can reduce the intensity of the syndrome are Tramadol.
- Local medications that contain capsaicin - “Mataren Plus” ointment.
NPS are used at the height of the disease. To alleviate the painful syndrome, a neurologist may prescribe:
- "Nimesulide", simple "Aspirin";
- "Ibuprofen" or "Desketoprofen";
- "Ketoprofen".
NPS allow you to numb the problem area and relieve inflammation during the period when neuralgia begins to progress. The drugs are taken orally in the form of a suspension, capsules or syrup. To relieve herpetic syndrome, topical agents with hot pepper extract are prescribed along with medications of this group. Lidocaine-based gel provides effective pain relief.
Important! If the patient suffers from unbearable pain during an exacerbation of the disease, in which an anti-inflammatory drug in combination with capsaicin-based ointment has no effect, then a strong analgesic, an antidepressant (tricyclic), is used to relieve the syndrome.
After recovery, postherpetic neuralgia is treated with novocaine blockades, drugs of the NPS group, using other methods at the discretion of the doctor and taking into account the individual characteristics of the body.
Other possible complications
In addition to the above-mentioned consequences of herpes zoster, the following may occur:
- Vasculopathies are inflammatory lesions of blood vessels and adjacent tissues.
- Myelopathies are a set of various pathologies at the level of the spinal cord. Accompanied by paralysis of the limbs, dysfunction of the pelvic organs, etc.
- Cerebellitis - acute ataxia (disorder of movement coordination). Manifested by gait disturbance, dizziness, nystagmus, etc.
- Damage to internal organs. The literature describes cases of acute liver necrosis and other diseases of internal organs. The development of complications had a clear connection with herpes zoster.
Herpes zoster develops against the background of a decrease in natural immunity and is characterized by the appearance of pain along the affected nerves. The disease is quite treatable, but in some cases it can cause serious complications.
Immunostimulants and physiotherapy in the treatment of lichen
The main reason why herpes can appear is a weakening of the body's defenses. It is difficult to answer how long the remission period lasts, since everything depends on external factors, the presence of concomitant diseases that can provoke the appearance of shingles.
Complex treatment will strengthen the body’s vitality and protect it from aggressive influences. For these purposes, a neurologist may prescribe immunomodulators:
- rectal suppositories "Viferon";
- "Arbidol" or "Cycloferon";
- drug "Neovir".
To strengthen the body and increase immunity in case of herpes zoster, multivitamin complexes are used. Sedative medications, herbal medicine, and vitamin decoctions can help eliminate nervous tension. It is useful to lubricate the rash with rosehip or sea buckthorn oil; it can also be taken orally.
Do they give sick leave?
Treatment of herpes zoster without complications with a mild course is carried out on an outpatient basis. Indications for hospitalization are:
- severe course of the disease (febrile fever, massive rashes, damage to the brain, eyes and hearing organs, incessant pain);
- bacterial complications and parallel exacerbations of concomitant chronic diseases;
- the presence in the family of a child or a pregnant woman who did not have chickenpox.
For herpes zoster, sick leave is given for outpatient and inpatient treatment: both for mild and complicated cases. Outside the period of exacerbation, in the absence of symptoms, sick leave is not required.
You should not self-medicate, the disease is mediated by immunosuppression and is viral in nature, so the treatment regimen should be drawn up only by a doctor.
Suppressing pain during relapse of herpes and neuralgia is not the primary goal of therapy. Suppression of virus replication and restoration of cellular immunity is the primary task in treatment and in the fight against pain.