Learn more about diseases starting with the letter “D”: Debility, Double-wave viral meningoencephalitis, Dementia with Lewy bodies, Depressive neurosis, Dermal sinus, Cerebral palsy, Jacksonian epilepsy, Diastematomyelia (diplomyelia), Discogenic myelopathy, Dystrophic myotonia Rossolimo-Steinert-Kurshman, Diabetic encephalopathy, Dyscirculatory encephalopathy, Diffuse axonal damage to the brain, Benign rolandic epilepsy.
Dementia with Lewy bodies is a progressive neurological disease caused by degenerative processes in the nervous system, in which inclusions that are not characteristic of them are formed inside nerve cells. The clinical picture is characterized by a combination of four pathological components:
- increasing dementia;
- mental dysfunctions with signs of parkinsonism;
- deviations of sleep and autonomic regulation.
The diagnosis is established taking into account the clinic, the results of the examination in establishing the neurological and neuropsychic status. Additional diagnostic methods include magnetic resonance imaging and PET scan of the brain. Treatment uses drugs aimed at improving the patient’s life.
general description
In dementia, pathological inclusions are formed inside the neuron, which include alpha-synuclein and ubiquitin. They were called Lewy bodies, since they were first discovered by the German morphologist F. Lewy in 1912. For a long time they were considered diagnostic signs of Parkinson's disease.
In 1950, scientific researchers from Japan described Lewy inclusion dementia as a distinct form of parkinsonism. “Diffuse Lewy body disease” became an independent nosology only in 1984.
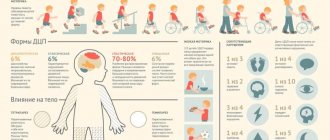
The first international symposium concerning the pathognomonic criteria of this pathology was held in 1995. In the course of it, this complex disease was given a current name – dementia with Lewy bodies (DLB). LNK includes 10-15% of cases of the total number of diagnoses - dementia. Elderly people over 60 years of age are more likely to get sick.
Dementia with Lewy bodies
Lewy body dementias (LBD) include both Lewy body dementia (DLB) and Parkinson's disease with dementia (PDD), and differentiating LBD from other neurodegenerative dementias can be quite challenging. There are currently several biomarkers that can aid in early diagnosis, reflect the severity of LBD symptoms, and provide indicators of treatment response. Traditionally, biomarkers in LBD have focused on neuroimaging modalities; however, since biomarkers should be simple, inexpensive, and noninvasive, neurophysiological approaches may also be useful as biomarkers for LBD.
Dementia with Lewy bodies (DLB) is the second most common cause of degenerative dementia in older adults after Alzheimer's disease (AD), with approximately 10–15% of dementia cases demonstrating Lewy body pathology at autopsy. In Parkinson's disease, dementia is common, and up to 80% of patients with Parkinson's disease eventually develop dementia as the underlying disease progresses. Collectively, DLB and Parkinson's disease dementia (PDD) can be grouped under the umbrella term Lewy body dementia (LBD) due to the overlap in symptom profile, similar response to treatment, and common underlying neuropathology of alpha-synuclein aggregation.
Cognitively, patients with Lewy body dementia have significant deficits in executive and visuospatial/visuo-perceptual function, as well as differences in levels of arousal and attention; the latter are usually called "cognitive fluctuations". Additional clinical features include spontaneous movements typical of parkinsonism and non-motor manifestations such as visual hallucinations, autonomic dysfunction, syncope, repeated falls, rapid eye movement disorder (RBD), delirium and depression are also typical of LBD and may pose significant problems for patients and their environment.
There are a number of treatment challenges for LBD. Severe cholinergic deficits occur in LBD and are even more evident than in AD. Restoring cholinergic function through the use of cholinesterase inhibitors such as donepezil, rivastigmine, and galantamine may have cognitive and neuropsychiatric benefits, including improvements in overall cognitive function, particularly attention and daily functioning. However, individual differences are often observed in response to these treatments. Stratification of responders is also observed, using appropriate biomarkers, which will help the clinical management of patients with LBD. Apart from cholinesterase inhibitors, there are few effective pharmacological treatment options, and agents such as memantine have been tried with varying success.
Existing candidate biomarkers that have been used in LBD have included clinical, biochemical, genetic, and neuroimaging markers such as cerebrospinal fluid (CSF) alpha-synuclein or beta-amyloid levels or alpha-synuclein gene mutations. Generally, the utility of these potential biomarkers is supported only in a research context, with the exception of dopamine transporter imaging, which, due to its high specificity in differentiating DLB from AD, is currently clinically recommended as a method to confirm the diagnosis of DLB in uncertain cases. However, imaging of dopamine transport remains expensive, exposes humans to radioactivity, and provides little or no information about disease progression or prognosis. In addition, this method does not clearly correlate with the severity of cognitive or neuropsychiatric symptoms in dementia with Lewy bodies. Similarly, although magnetic resonance imaging (MRI) has been shown to be a useful tool in the differential diagnosis of dementias, its use in LBD is relatively limited and compared to other modalities because MRI imaging has the disadvantage of being relatively high in cost . Alternatively, cerebrospinal fluid (CSF) testing has also been considered as a potential biomarker in LBD, where testing may include assessment of alpha-synuclein levels. Another disadvantage of using CSF as a biomarker is that it cannot be done in a non-invasive manner.
Various EEG analytical techniques have been used in LBD, such as the use of the global summary EEG (GTE) score (a differentiated composite measure that takes into account the presence of EEG features such as diffuse slow wave or focal abnormalities), analysis of frontal intermittent rhythmic delta activity, and the use of compressed spectral arrays . A long-described EEG feature of DLB is the presence of posterior (transient) transient slow or sharp waves; diagnostic criteria for DLB include these as a supporting feature of the condition.
Etiology of DLB
The causative factors for the development of this type of dementia have not yet been clarified. It is known that the basis of dementia is destructive mechanisms leading to the destruction of neurons. Scientists are trying to find a possible connection with genetic transmission factors. Thus, in half of the cases, the diagnosis was established in patients who have first-degree relatives suffering from Parkinson’s disease or senile dementia. But due to the clinical polymorphism of this disease, it is extremely difficult to find a connection with hereditary transmission between relatives.
In publications on neurology, a case was discussed describing the observation of a mutation in the parkin gene park2 in a Japanese family, in which the development of Parkinson's disease and DLB was traced depending on the severity of the defect in this gene.
Indicators of genetic research, in the presence of which the risk of developing the disease significantly increases, include:
- allele ε4 on chromosome 19;
- mutations in the GBA gene of chromosome 1;
- mutations in the LRRK2 gene of chromosome 12;
- changes in locus 2q35-36.
Features of the disease
There are specifics in the development and course of dementia with Lewy bodies. The disease begins between the 6th and 8th decades of life. Men get sick 1.5–2 times more often than women. Gerontological doctors identify three main differences between this disease and other forms of dementia.
Behavioral disorders are uneven. Disorders of memory and mental performance can become more or less pronounced: the patient moves from activity to apathy, from the desire to communicate to the inability to carry on a conversation, from clear memory to the inability to remember, recognize relatives or friends. Such fluctuations can occur over several hours (they are small and usually related to the time of day). Changes can also be extended over several days or several weeks. Long-term, “large” fluctuations are usually associated with health status, well-being, exacerbation of diseases, infectious diseases, and other factors. Fluctuations usually begin with sleep disturbances, with the appearance of psychotic disorders, after which the person ceases to navigate time and space, loses memory, and his speech deteriorates. The patient may suffer from nightmares - so severe that they provoke sudden awakenings, fear of falling asleep, and falling out of bed. At the “peak”, hallucinations or complete apathy, isolation, and lack of contact are possible. After some time, cognitive functions begin to recover: the person begins to communicate, memory improves. Such recovery may be incomplete - so that after each new cycle, cognitive functions gradually weaken.
Severe lack of concentration. When an elderly person is ill, it is especially difficult to concentrate on anything: he cannot concentrate on a conversation or a task at hand, he is easily distracted, and gets tired. Impaired concentration is much more pronounced than in Alzheimer's disease - so much so that it is difficult for a person to plan actions, carry them out, evaluate their results - he simply cannot concentrate on a goal or process, and quickly switches to abstract things. Because of this, an elderly person may become fixated on one task, starting to do it many times, but not finishing it.
Difficulty recognizing objects. A characteristic symptom of dementia with Lewy bodies is visuospatial disturbances. The patient feels that his vision has deteriorated, he cannot recognize, recognize objects, and may also experience visual illusions or hallucinations in which inanimate objects seem animate (for example, instead of a clothes hanger, the patient sees a person). Hallucinations often appear in the evening or at night.
Already at an early stage of dementia with Lewy bodies, patients develop movement disorders and parkinsonism. Movements become constrained, muscle tone increases significantly, trembling of the limbs appears, it becomes difficult for the patient to maintain balance, he loses stability. The gait changes quickly - the step becomes shortened, shuffling, and frequent falls are possible.
The disease progresses at a rapid rate - impairments develop faster than in other forms of dementia, and patients reach a severe stage on average within five years after the first symptoms are detected.
You have questions?
We will call you back within 30 seconds
or call the number
Clicking the "Submit"
, you automatically consent to the processing of your personal data and accept the terms of the User Agreement.
Pathogenesis
In 35% of elderly people, Lewy bodies can be found in a small number of nerve cells and are normal, which is associated with the natural mechanisms of aging of the body. In connection with what mechanisms the processes of brain aging are accelerated in dementia with Lewy bodies, science is not yet known. Scientists assign a certain importance to the process of inhibition of antioxidant systems and activation of the glutamatergic system, as a result of which calcium rushes into neurons and changes the charge of its membrane.
At the beginning of the manifestation of DLB, metabolic processes in the occipital region of the brain are disrupted in the direction of their slowdown, which causes changes in spatial orientation and the development of visual hallucinations in patients.
When neuronal degeneration spreads to the substantia nigra and striatum, patients develop signs of parkinsonism, and damage to the brainstem nuclei causes dysfunction of the autonomic regulation of vascular tone.
Differential diagnosis
Dementia with Lewy bodies has a similar clinical picture to Parkinson's and Alzheimer's diseases. In this regard, doctors need to carry out differential diagnosis between these diseases.
Parkinson's disease is characterized by an earlier onset of motor impairments compared to mental and intellectual impairments. Tremor of the limbs is present even at rest, muscle rigidity is more pronounced.
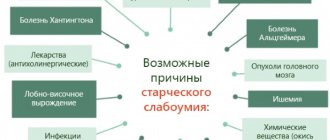
Alzheimer's disease can be differentiated from dementia with Lewy bodies using MRI results. Tomography allows you to establish the exact localization of the pathological process and the extent of its spread. In addition to Alzheimer's and Parkinson's disease, dementia with Lewy bodies must be distinguished from the following conditions:
- Neoplasms of the brain. As the tumor grows, nearby brain structures are compressed. This is manifested by a decrease in intellectual abilities, mental and neurological disorders.
- Neurosyphilis. Diagnosed against the background of untreated syphilis. As a result, the causative agent of the disease penetrates the brain and spinal cord.
- Hypothyroidism. Sleep disturbances, decreased intellectual abilities and slowed speech occur due to decreased levels of thyroid hormones.
- Hydrocephalus. It is characterized by excessive accumulation of cerebrospinal fluid in the region of the ventricular system of the brain.
Symptoms of DLB
The clinical symptoms of this pathology are morphologically diverse; they can be divided into the following blocks:
- Impaired cognitive functions. At the onset of the disease, patients are unable to concentrate their attention to perform complex tasks. Then, quite soon, signs of impaired visual perception (agnosia) appear, characterized by failure to recognize ordinary objects and familiar people; a little later, patients find it difficult to remember close relatives. As the disease progresses, the patient cannot recognize his own reflection. A characteristic symptom is early visual hallucinations. Memory dysfunctions arise later and manifest themselves in impaired search and retrieval of information stored in the brain. Speech changes are not typical.
- Mental disorders characteristic of DLB are various types of hallucinations, depressive and dissociative disorders, delusional states, delirium, apathy, psychomotor agitation. This wide range of psychotic disorders has an intermittent nature. That is, periods of deterioration in the patient’s consciousness are replaced by bright episodes. Moreover, the time interval between “clouding and enlightenment” of consciousness can be different, from several minutes to several days. In 20% of cases, mental disorders develop in the final stage of DLB.
- Motor disorders in 50% occur at the onset of the disease. These include slowness of movement, muscle hypertonicity, instability of posture and gait, and tremor. With further progression of dementia, symptoms characteristic of Parkinson's disease develop with a frequency of 80%. Sometimes myoclonus occurs.
- Autonomic dysfunction caused by impaired vascular regulation leads to the development in patients of bradycardia, orthostatic hypotension with the possibility of fainting, functional disorders of the digestive tract, dysuric phenomena (involuntary urination at night, strong urge to urinate and urinary incontinence). The change in phases of sleep and wakefulness is disrupted, patients sleep during the day and are awake at night. Restless sleep, accompanied by screams and motor agitation.
Is treatment for dementia possible and how is it carried out?
There are no medications or any manipulations to get rid of a specific protein - Lewy bodies, but you can reduce the severity of symptoms and reduce the frequency of attacks. The most effective treatments are cholinergic drugs, such as Donepezil or Rivastigmine. They help improve concentration and other cognitive functions. These drugs also help with behavioral and psychotic disorders.
Therapy for Lewy dementia is symptomatic and complex:
- Elimination of signs of parkinsonism. Levodopa is most often used, but it helps less in dementia than in Parkinson's disease. The use of antiparksonian drugs can cause psychotic disorders. In order to overcome muscle stiffness, Baclofen is prescribed.
- To treat hallucinations in dementia, antipsychotics are used, but in minimal doses, since they are poorly tolerated by such patients. If a person is injected with a drug that is usually prescribed against hallucinations in other diseases, this leads to depression of consciousness, aggravates rigidity and often causes death.
- The best treatment for dementia is depression. When selecting antidepressants, it is important to consider how they interact with other prescribed drugs, whether they cause drowsiness and disorders of the autonomic system.
- To relieve symptoms that are similar to Alzheimer's disease, medications that inhibit amyloid production should be used. It is also necessary to prescribe antioxidants, nootropics, and agonists.
- Electroconvulsive therapy is used to treat parkinsonian symptoms and depression, but the stimulation must be carried out very carefully, since this method of treatment can often depress cognitive function.
There are also therapies that are not medical:
- sessions with a psychotherapist individually and with your family;
- occupational therapy, aromatherapy, music therapy;
- classes with a speech therapist;
- physiotherapy.
An integrated approach to treatment will help to significantly improve the patient’s quality of life.
Complications
The main complications include loss of self-care skills, and therefore patients require continuous monitoring and care.
If treatment is prescribed to a patient at the wrong time or incorrectly, the patient may develop the most severe complications. Thus, increased mental changes occur when dopamine is prescribed. And when antipsychotics are prescribed to reduce mental disorders, the patient develops a dangerous neuroleptic syndrome, characterized by the development of acute failure of the main organs and systems, up to the death of the patient.
Clinic
Clinically defined as parkinsonism syndrome and progressive cognitive disorder without any particular memory impairment. Cognitive impairment manifests itself primarily in the progressive limitation of visual-spatial perception and attention. The occurrence of intellectual dysfunction in the presence of parkinsonism is typical for no more than one year. Pronounced fluctuations in cognitive impairment and wakefulness during the day are specific, partly even with a lack of reaction to treatment, a “absent” look. Repetitive, pronounced and memorable visual hallucinations (animals, people, scenes). Frontal functions may be limited, but still not very pronounced, they also do not deteriorate so much during the course of the disease. However, in contrast to visuospatial perception, these deficits clearly improve with initiation of levodopa treatment (Williams-Gray et al. 2009). Apparently, this is explained by a deficiency of dopamine in the frontal lobes, while the parietal-occipital cortex is responsible for visual-spatial perception.
Revised diagnostic criteria for DLB (after McKeith et al. 2005)
1. Prerequisite
Diagnosis of LBD is a progressive dementia syndrome. Severe or persistent memory impairment is not necessary in the initial stage of the disease, but usually occurs later. The clinical picture is usually dominated by deficits in attention and visual-spatial perception.
2. Cardinal
symptoms are:
- fluctuations in brain function, especially with regard to wakefulness and attention.
- recurring visual hallucinations, usually detailed and well defined.
- parkinsonism syndrome.
the diagnosis of DLB is possible
one
of the cardinal symptoms
is present The diagnosis of DLB is probable
if at least
two
cardinal symptoms are presented.
3. Typical
symptoms:
- violation of the REM stage of sleep (Schenk syndrome - talking or screaming during the REM stage of sleep, motor expressions of dreams).
- severe sensitivity to neuroleptics
- decreased striatal DAT binding in SPECT or PET studies.
If one or more typical symptoms occur in the presence of one or more cardinal symptoms, a diagnosis of “ probable
” DLB is possible.
If there are no cardinal symptoms,
at least one typical symptom possible The diagnosis of “probable” DLB cannot be made based on typical symptoms alone
4. Supporters
symptoms:
- Recurrent falls or fainting
- Brief loss of consciousness
- Severe autonomic dysfunction
- Hallucinations of other senses
- Systematized nonsense
- Depression
- Relative preservation of meseotemporal structures in SPECT or PET, including occipital structures.
- Marked slowing in the EEG with transient temporal sharp waves.
5. The diagnosis of DLB is unlikely
:
- For cerebrovascular diseases with focal loss of function or structural abnormality in or MRI
- For other brain or systemic diseases that may explain the clinical picture.
- When parkinsonism occurs in an advanced stage of dementia
6. Time order
symptoms: the diagnosis of DLB is valid only if dementia occurs no later than one year after the onset of symptoms of parkinsonism. The diagnosis of Parkinson's disease with dementia is valid when symptoms of dementia occur against the background of advanced parkinsonism.
Hardware diagnostics
Computed tomography and magnetic resonance imaging - as a rule, minor brain atrophy is detected. SPECT/PET: characterized by hypoperfusion and decreased metabolism in the occipital and parietal regions, dopamiergenic disruption of associations in the striatum, in FP-CIT-dopamine transport SPECT and in fluoride-dopamine-PET
Diagnostics
With this pathology, a diagnosis can be made only by clinical signs, since the disease has several pathognomonic characteristics:
- A combination of several neurological changes - dementia, signs of parkinsonism, hallucinatory syndrome, autonomic dysfunction, dyssomnia.
- The intermittent nature of the course of clinical symptoms, with the presence of “good and bad” days.
- The order of appearance of symptoms is dementia at the beginning of the disease, then the phenomena of parkinsonism. Possible simultaneous appearances.
The next step in making a diagnosis is to determine the neurological and mental status through examinations by a neurologist and psychiatrist.
At the beginning of the development of the disease, the neurological status is characterized by slow thinking, inability to concentrate, and behavioral disorders. At later stages, when extrapyramidal dysfunction develops, the neurologist will detect a decrease in the volume and amplitude of the patient’s movements, difficulty raising legs when walking with the formation of “shuffling,” a decrease in facial movements, plastic-type muscle hypertonicity, myoclonus and tremor.
To establish the mental status, the psychiatrist conducts neuropsychological testing with the patient, based on the results of which the doctor assesses not only the general psychostatus, but also determines the degree of dementia on the Mattis scale and the speed of functioning of mental processes. Difficulties in diagnosis may arise if the patient, even in the initial stages of dementia, can hide the presence of hallucinatory manifestations.
Instrumental diagnostic methods include magnetic resonance imaging and PET-CT of the brain, polysomnography.
The following features are found on the brain tomogram: mild diffuse cerebral atrophy, damage to the structures of the occipital zone, total damage to the subcortical ganglia.
According to PET-CT of the brain, a decrease in the level of metabolism in neurons and perfusion indicators in the occipital zone is detected, as well as significant damage to subcortical structures.
A characteristic sign of DLB is considered to be a combination of indicators of damage to the occipital lobes of the brain according to MRI (atrophy) and PET-CT (hypometabolism in neurons).
When performing polysomnography, psychomotor agitation is detected in a patient in the REM sleep phase, which is considered typical during the development of degenerative processes in the nervous tissue.
The diagnosis of DLB is differentiated from other mental illnesses that occur with the phenomenon of dementia:
- Alzheimer's disease;
- secondary parkinsonism;
- Parkinson's disease, which was combined with the vascular genesis of dementia;
- Pick's disease;
- other forms of dementia.
The Alzheimer's type of dementia develops at a later age (from 65 years of age), with it cognitive impairment is rapid and total, hallucinations develop later, and degeneration in the brain is more pronounced and widespread.
Unlike Parkinson's disease, with BTL, cognitive impairment first develops, and then the phenomena of parkinsonism develop. The difference from Pick's disease is the presence of extrapyramidal disorders.
Clinical manifestations
In the case of a disease caused by the appearance of Lewy bodies in the nervous tissue, the clinical picture is clearly expressed and specific, which makes it possible to make an accurate intravital diagnosis. The specificity of diagnostic criteria is 92%. The age of onset of symptoms in dementia associated with Lewy bodies varies between 40-90 years. More often, the pathology debuts at the age of 70-80 years.
Signs of parkinsonism occur against the background of damage to the substantia nigra and structures of the striatum. Sleep disturbance is associated with damage to the brainstem region. Autonomic dysfunction develops as a consequence of damage to the stem ganglia and involvement of peripheral components of the autonomic nervous system in the pathological process, which leads to denervation (disorder of nervous regulation due to impaired innervation) of the heart in the early stages of DLB.
The syndrome caused by the appearance of Lewy bodies includes cognitive deficits, motor dysfunction, autonomic disorders, sleep disturbances, including pathological deviations in the alternation of sleep and wakefulness phases. Cognitive-mnestic dysfunction in the initial stages is manifested by a disorder in the ability to concentrate attention, the inability to maintain attention on an object for a long time.
Visuospatial disturbances are a clinically significant sign of DLB. The progression of the disease leads to errors in recognizing visual images - the faces of familiar people, household objects. The visual perception of oneself is disrupted when the patient, looking at the reflection in the mirror, perceives it as another person.
Visuospatial disorders are associated with the occurrence of visual hallucinations. The memory function usually suffers to a lesser extent, more often manifested by a violation of the reproduction and comparison of stored information with new data. Behavioral disorders associated with a sudden deviation from normal behavior patterns are typical.
For example, transient episodes of deterioration in concentration, decrease in activity with pronounced unresponsiveness (lack of reactions to external stimuli) and aspontaneity (lack of urges to engage in any activity - motor, mental, speech). Often during such periods there is darkness and a decrease in the level of consciousness. The duration of the episodes usually varies from a few minutes to hours.
Long-term fluctuations (episodes of behavioral abnormalities) can last up to several days. Psychotic disorders are considered clinically significant criteria. However, it should be borne in mind that in about 20% of patients, mental dysfunction is observed only in the later stages of the course.
Within the framework of psychotic disorders, along with visual, auditory, and tactile hallucinations, disorders are identified - an unreasonable sensation of the presence of objects and people, illusions, delusional states, delirium (confusion with impaired perception, attention, emotions, and mental activity). Often in the early stages there is the development of depression and increased anxiety. Signs typical of later stages:
- Apathy, loss of interest in the surrounding reality.
- Psychomotor agitation, agitation.
- Disinhibition of drives and behavior.
These manifestations complicate patient care. Motor dysfunction in the early stages is detected in 50% of patients, mainly manifested by parkinsonism, which often debuts with damage to the left side of the body. Main movement disorders:
- Postural instability, causing the inability to maintain balance, frequent falls.
- Hypomimia (weakening of the expressiveness of the facial muscles or loss of the ability to form facial reactions, lack of facial expressions).
- Dysphonia (decreased strength and sonority of the voice).
- Dysarthria (speech disorders caused by impaired innervation of the muscles of the speech apparatus).
- Gait disturbance, freezing in one position, bradykinesia.
Disturbances in the frequency of sleep and wakefulness often appear before other signs. During sleep, rapid movements of the eyes are often observed, which is associated with psychomotor agitation. Another common symptom is daytime sleepiness.
Treatment of DLB
At this stage of medical development, specific treatment has not yet been developed. Current therapy can only alleviate the main symptoms of the disease in order to improve the quality of life of the patient and those caring for him.
In order to correct cognitive and mental abnormalities, cholinesterase inhibitors (rivastigmine, donepezil) are prescribed, which have a positive effect on the patient’s memory, sleep, behavior and motor activity, and reduce the manifestations of hallucinatory syndrome. Side effects often occur when taking them. An NMDA antagonist (memantine) is also used, which alleviates mental disorders, but does not restore cognitive functions.
Treatment of manifestations of parkinsonism is carried out with small dosages of levodopa, which is prescribed for severe symptoms, since this drug can aggravate mental changes.
Caring for a patient is a very labor-intensive process, which is often performed by relatives. For the purpose of adequate care, it is necessary to conduct counseling explaining the features of caring for the patient, and possibly psychological assistance to the caring person.
A promising direction in the development of drugs that inhibit degenerative processes in neurons is the discovery of drugs that prevent the aggregation of α-synuclein, which will stimulate the dissolution of intracellular Lewy bodies.
Treatment
Dementia that develops as a result of damage to the brain by abnormal alpha-synuclein proteins has no permanent cure. The pathological process of destruction of interneuron synaptic connections is highly transient. If life expectancy with Alzheimer's dementia varies on average from 7 to 10 years, then Lewy bodies shorten a person's life to 5 years.
Treatment of dementia with Lewy bodies is usually complicated by the negative reaction of patients to classical antipsychotics. This feature has become another specific sign by which the disease can be recognized. Erroneous prescription of even moderate doses of standard antiparkinsonian drugs can provoke visual hallucinations and other severe psychotic disorders in patients. Dopamine agonists and anticholinergic drugs, which can cause a significant deterioration in the patient's condition, are also contraindicated.
Important! Hypersensitivity to antipsychotic medications often results in paralysis, acute respiratory and liver failure, myocardial infarction, and sudden cardiac arrest.
Supportive symptomatic therapy includes atypical antipsychotics, acetylcholinesterase inhibitors, memantine, levodopa, and antidepressants. An important place is given to the organization of quality care with an optimal diet, physical and intellectual activity, sleep and rest.
Despite the spread of the pathology, dementia with Lewy bodies remains a disease with many questions. The main problem of this disease is the presence of similarities with other more well-known types of acquired dementia and relatively mild symptoms during the period of manifestation. In case of an erroneous diagnosis and incorrect treatment, the patient’s suffering can only intensify.