Scientists say: people who have a cat in their house get sick five times less often than others. The statement is justified, because in the course of numerous experiments it was found that furry “antidepressants” normalize blood pressure, speed up recovery and even strengthen the immune system. And at the same time, a cat bite, even if superficial and received during fun, can lead to serious consequences and even shorten the life of the victim.
Moreover, the danger lies not in the wound itself, but in its infection by dangerous microbes living in the animal’s saliva. And then the prognosis is determined by the timeliness and competence of first aid. If you let the situation take its course, the infection will enter the bloodstream, spread to all organs and lead to the development of serious conditions.
What does a cat bite look like?
Even a very angry animal is not able to tear a person to pieces, because a cat's jaws are quite weak. And a cat bite that does not have a large area of damage is difficult to confuse with the bite of another animal.
Thin, elongated fangs bite sharply into the skin, leaving deep marks that require treatment - closed, slowly healing puncture wounds (in rare cases, the edges of the wound are torn). Usually, next to the punctures there are traces of scratches. After healing, the damaged skin becomes scarred.
You need to know this! As a rule, cats bite people on the hands, palms, fingers or wrists. A severe pain syndrome develops in the bitten limb, limiting the victim’s movements. Regardless of the depth of the lesion, the wound turns red and swells.
Specifics of cat bites
Pathogenic microorganisms living in the saliva of a pet are extremely dangerous to humans. By sinking its teeth into soft tissues and tendons, the animal “rewards” the person with a whole range of infections. So the danger of a cat bite is not in damage to the skin, but in the entry of the animal’s saliva into the wound.
Having sunk into the epithelial layer, bacteria rapidly multiply, causing an inflammatory reaction in the form of edema. The bitten area (most often a hand or finger) swells before our eyes. If a cat bites a joint, its mobility is impaired.
Immediate treatment of the wound and proper antibacterial therapy will stop the inflammatory process and protect the victim from serious consequences.
Signs of infection in an animal
The disease is manifested by the following symptoms:
- drooling;
- fear of approaching water or inability to take a sip of liquid;
- aggression.
In some cases, the animal becomes friendly, approaches the owner, and allows itself to be petted.
A pet develops several phases of the disease:
- prodromal;
- manic;
- depressive.
In the first stage, the pet does not attract the attention of its owners. The cat moves little, hides from people, reacts to noise and light.
Involuntary movements of the upper and lower jaws appear, and eating behavior changes. The animal tries to chew on inedible objects, drooling and vomiting occurs.
In the second phase of rabies infection, the pet becomes aggressive: it bites and gnaws on wooden objects. The animal is trying to leave the house and does not understand affection or other measures of influence.
In the third stage, the cat experiences a spasm of the larynx muscles, he cannot drink liquids or eat food. Paralysis affects the limbs.
The last phase is coma, respiratory failure, exhaustion, and death. A depressive form of the disease is possible, and rapidly progressing paralysis kills the animal within a few hours.
Possible consequences of a cat bite
Even a superficial cat bite can damage the victim’s health. After all, pathogenic microflora from the saliva of an animal that enters the body through damaged skin leads to the development of infections in 80% of cases.
Attention! Microbes dangerous to humans were found in the saliva of nine out of ten examined cats.
Diseases
Most often, cat saliva contains the following microorganisms:
- pasteurella;
- streptococci;
- staphylococci.
Most of the listed microbes belong to the group of opportunistic pathogens. This means that under the influence of unfavorable factors, completely harmless microorganisms inhabiting the body of a warm-blooded animal become causative agents of inflammatory processes. And once in a fresh wound, they can accelerate or provoke the development of the following diseases:
- Benign lymphoreticulosis or “cat scratch disease.” The causative agent is chlamydia, which enters the body through scratches and bites. Once the wound becomes infected, the affected area becomes red and swollen. After 3 weeks and after the bite site has healed, fever may appear, accompanied by chills, an increase in temperature to abnormal levels, and loss of appetite. If the disease is left to chance, the infection affects the lymphatic system, the brain: the person begins to have headaches, the lymph nodes located next to the bite become inflamed. Children who like to play with kittens are especially susceptible to infection (the older the cat, the lower the likelihood of contracting lymphoreticulosis).
- Pasteurellosis. The causative agent of this disease more often than others enters the victim’s blood after a cat bite. Immediately after the bite, redness and swelling of the injured area are noted. Symptoms of acute infection: fever, chills, fever, skin inflammation. The advanced stage of pasteurellosis leads to systemic inflammatory reactions: arthritis, osteomyelitis, etc.
- Tetanus. When bitten by a cat, especially a stray, there is a risk of contracting tetanus. The causative agent of a dangerous disease lives in soil, feces or objects. In a small closed wound, anaerobic conditions are created (and this is an ideal environment for the development of bacteria). If antitetanus serum is not administered to the victim, death is inevitable.
- Rabies (hydrophobia). From the moment of infection to the manifestation of the clinical picture, rabies in cats develops from 9 to 51 days. And only after this, a week before death, the animal begins to hide from bright light, attack people, meow loudly and protractedly, and violently gnaw inedible objects. Paralysis of the larynx and sagging of the lower jaw leads to drooling. If you notice an animal with the described symptoms, move away to a safe distance and call the sanitary service. Otherwise, the animal will do a lot of trouble. If a sick animal does attack, you should immediately consult a doctor. If you miss the moment, the rabies virus will provoke damage to the central nervous system that is incompatible with life.
- Staphylococci, streptococci. After pathogenic bacteria penetrate the body, a person develops aching bones, skin rashes, cough, dermatitis, suppuration of the bite site, severe damage to the respiratory system (pneumonia, bronchitis, etc.).
Cats tolerate staphylococcal and streptococcal infections no more easily than humans. An infected animal has difficulty breathing, discharge from the eyes and nose, and joints and bones become inflamed.
If you notice the described symptoms in your pet, immediately take him to the veterinarian. Thus, you will protect yourself and your loved ones from dangerous infection.
Swelling and pus
Swelling and pus may appear in the bitten area. This often happens if, when a cat bites, the wound is not washed and treated with a disinfectant solution.
If the wound is clean, swelling is barely noticeable and there is very little pus. If the cat just scratched, the scratch swells slightly and heals within a couple of days.
With a deep bite, swelling and suppuration do not go away within 3-5 days. And throughout the entire healing period, the wound needs daily disinfection. If the healing process is delayed or the suppuration intensifies, you cannot do without the help of a doctor.
What is rabies in cats?
Almost all people know what rabies in cats is and are terrified of this virus. The fear is not unfounded; rabies is one of the common viruses for humans and animals that cannot be cured after the first symptoms appear. Unfortunately, rabies is widespread throughout the globe, despite aggressive and strictly controlled prevention measures.
A virus that has entered the body of a healthy animal or person actively multiplies and infects the tissues of the brain and spinal cord. Due to the destruction of neural connections, the behavior of the infected animal becomes inadequate, which leads to further spread of the virus.
The lifespan of an infected cat is short, usually ranging from 10 to 16 days. During this time, the clinical picture rapidly develops and the infected animal becomes aggressive. If the cat is domestic, the owner, his entire family and other pets living in the house are at risk.
Signs of infection
After a cat bite, you should listen to how you feel and pay attention to the condition of the wound. This safety requirement will make it possible to identify pathology at the initial stage and relieve the victim of painful symptoms and life-threatening complications.
Note! If a cat bite causes suppuration and severe swelling of the injured area, the infection can “leak” into the periosteum, joint or bloodstream.
Swelling
Any cat "mark" will swell and swell, whether it's a deep bite or a superficial scratch. It happens that the swelling surrounding the wound turns red and hurts. This indicates the penetration of pathogenic microorganisms under the skin. Provided the bitten area is thoroughly treated and the victim follows hygienic requirements, the swelling will disappear in a few days.
Fever
When a cat is bitten, the temperature may rise to subfebrile levels (37.1 - 37.7 C°) and not subside for 1-2 days. If the mercury column has jumped to 38 C° or higher, and the inflamed area of skin literally “boils” - this is an alarming symptom indicating a serious inflammatory process. In this case, without qualified medical assistance, the victim’s condition will only worsen.
Redness
Human skin responds to any damage with irritation and redness. When there is a cat bite and the wound becomes infected, severe redness is accompanied by overheating of the injured area. Purulent discharge may appear.
Important! A cat bite is more dangerous than a cat bite. Males disappear on the street for days, communicate with relatives, and can have a snack in the trash heap for company. As a result, cadaveric poison, which is extremely dangerous for humans, remains on the animal’s teeth.
What can you get infected from cats?
Bites from cats, even domestic and vaccinated ones, need proper treatment. If the injury was caused by a stray animal, it is necessary to see a doctor as soon as possible in order to promptly stop the development of the following diseases:
- tetanus;
- rabies;
- blood poisoning;
- allergic reactions of varying severity;
- infectious cellulitis;
- dermatitis, dermatoses;
- inflammation of the lymph nodes.
Tetanus infection from a cat bite
Tetanus is a bacterial disease that affects the central nervous system and bone/muscle tissue and leads to seizures. An infected cat exhibits convulsive contractions of the masticatory muscles and lack of coordination (the animal skids when walking). If a person is bitten by a cat suffering from tetanus, he will experience characteristic symptoms:
- temperature rises;
- severe headaches begin;
- the bite site swells;
- lymph nodes become enlarged and painful;
- muscle tension is felt, turning into cramps.
Without urgent drug therapy (antibiotics and antitetanus serum), death is inevitable.
Infection
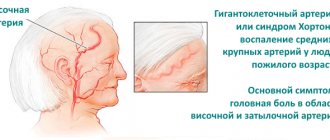
The rabies virus can enter the body unnoticed. The starting point is the place through which the infection occurred. From there, the virus begins to spread, approaching the brain. In parallel with this, its cells actively multiply, increasing their efficiency. Every hour they rise higher, and the patient’s body experiences new problems. After some time, damage to the brain and spinal cord occurs, and the central nervous system ceases to function fully.
Infection at points close to the head is especially dangerous. This is because the time required to reach the brain will be very limited. As a result, doctors may not have time to take all necessary measures to prevent the development of the virus in the infected person’s body, which will make death inevitable.
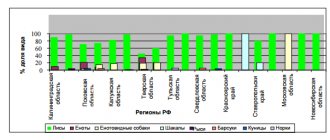
The main carriers of the virus are wild animals and livestock: foxes, wolves, hedgehogs, badgers, raccoons, rodents, sheep, cows, pigs, goats and some other species. You can also get infected from a cat or dog, and most of the diseases have been registered in the case of the latter. Everyone knows how rabies is transmitted from dogs to humans. This happens through a bite. They can also become infected from other animals.
The virus is contained in the salivary glands, where it enters 1-7 days before the first symptoms appear, and spreads best when it enters the blood of a healthy body. That is why, after being bitten by a sick animal, you should not hesitate. Other routes of infection cannot be excluded:
- Damage to the skin from the claws of a sick animal;
- Contact of damaged skin with an object containing saliva from a sick animal;
- Contact with saliva on the mucous membranes of the eyes, nose or mouth;
- Cutting up the carcass of an animal with rabies;
- Airborne (when in a cave with sick bats).
The virus can also be transmitted to the fetus from an infected mother during pregnancy or to people during internal organ transplantation, but only isolated cases have been reported. Is rabies transmitted from person to person in everyday life? Theoretically, you can become infected through a kiss if a healthy person has wounds in his mouth. However, the probability of transmission of the virus from person to other people is so small that the vast majority of experts tend to consider it zero.
More than 50 thousand people die from rabies every year, and most cases of infection occur in the spring and summer months.
Signs of rabies in humans
Rabies is the most dangerous consequence of a cat bite. The spread of the virus leads to damage to the brain, nervous and motor systems. An infected animal has no chance of survival.
To save a person infected with rabies, the administration of rabies vaccines is required. The main thing is not to be late in seeing a doctor before symptoms appear:
- temperature rise;
- inflammation of the bitten area;
- loss of appetite;
- gagging;
- emotional lethargy or nervousness.
This will be followed by respiratory arrest, cardiac paralysis and painful death of the victim.
How does a person become infected with rabies from a cat?
As a rule, domestic cats become infected with rabies from hedgehogs, foxes and stray animals (over 70% of infections occur during out-of-town trips). The rabies virus is transmitted from a cat to a person through infected saliva: through a bite or contact of saliva with damaged skin.
During the incubation period, a healthy-looking animal already poses a danger. And if you are bitten by a cat, do not tempt fate and do not delay in seeing a doctor.
The first signs of rabies in humans
After a long incubation period, sometimes accompanied by itching, burning and aching pain in the wound, the person experiences the first abnormalities in the nervous system:
- fear of bright light;
- problems swallowing;
- unnaturally loud reaction to loud sounds;
- headache;
- general weakness;
- temperature rise to subfebrile levels;
- lack of appetite;
- dyspeptic disorders: abdominal pain, diarrhea, vomiting;
- cough and runny nose.
After the manifestation of the listed symptoms, the person is doomed. The virus occupies the central nervous system and causes progressive, fatal inflammation of the brain and spinal cord. Therefore, at this stage of development, rabies is recognized as an incurable disease.
You need to know this! The first manifestations of the deadly virus begin a few weeks after infection, but until then, the spread of deadly microorganisms can be stopped with the help of vaccination.
Features of the lush form
Patients with violent rabies are hyperactive, overexcited, afraid of water and drafts (in rare cases). The sight and sound of pouring water is terrifying, and there is drooling and excessive sweating.
The swallowing muscles are contracted from fear and the thirsty person is unable to drink. Paralysis of the heart or respiratory muscles can occur at any moment.
The patient's condition may unexpectedly improve: fears and spasms will disappear along with the depressive state. But after three days the condition worsens again:
- blood pressure drops sharply;
- heartbeat becomes faster every hour;
- paralysis appears;
- body temperature rises to 42 C°;
- death occurs as a result of cardiac or respiratory arrest.
Paralytic form
The paralytic (atypical) form of rabies develops in only 20% of infected people. One lasts longer and less dramatically than the violent one. The muscles gradually become paralyzed, starting from the bitten or scratched area.
Over time, the person falls into a comatose state and dies. The absence of symptoms characteristic of rabies leads to frequent medical errors, which is why data on the disease are underestimated.
Incubation period after rabies infection
In most cases, the incubation period for rabies lasts 2–3 months. However, depending on the physical condition of the victim, the functioning of his immune system, the place of entry of the virus and the viral load, this indicator can vary from 7 days to 1 year. From the moment of infection until the first symptoms appear, a person does not feel sick.
Bites to the face, neck, hand joints or genitals are extremely dangerous - areas enveloped in a larger network of nerve endings through which the infection spreads. For every hour, the rabies virus spreads through the nerves by 3 mm until it covers the brain area.
How does a person become infected with rabies from a cat?
Rabies is transmitted from a cat to a person by a bite when an infected animal attacks a person. Infected saliva enters the human nervous system.
Rabies is transmitted from a cat to a person by a bite
The virus remains at the site of the bite for up to 10 days. After this, the infection spreads along the nerve fibers throughout the body. The propagation speed is 3 mm/h.
It is impossible to detect the virus in the blood. The infection reaches the spinal cord and travels through the nerve endings to the brain. The virus also settles in the salivary glands.
Brain damage leads to severe impairment. A person loses control over himself, hallucinations and aggressive behavior appear.
The patient has difficulty breathing and swallowing. Salivation increases, attacks occur: the patient throws his head back, stretches his arms forward.
You can become infected with rabies from a cat that has no symptoms of the disease. If the animal has become infected in the last two weeks, then signs of infection have not yet appeared.
What to do if bitten by a cat?
If a person is bitten by a cat, then it is necessary to provide first aid to the victim:
- Rinse the wound under running water for 10 minutes. Use soap.
- Treat the edges of the wound with a disinfectant.
- Apply a sterile bandage. Wrap loosely.
- Go to the hospital emergency room.
Be sure to read:
Panleukopenia in adult cats and kittens: the first signs of the disease, how to treat and what to do
These actions will help avoid bacterial infection, but will not protect you from illness. If someone else's cat has bitten you, the doctor will suggest giving you a rabies injection.
The injection is placed in the forearm area or at the site of injury. Refusal of the injection in case of infection will lead to the death of the patient.
If you are bitten by a domestic cat that has not been exposed to other animals for the past two weeks, you can refuse the vaccine.
What not to do in case of a cat bite:
- stop minor bleeding;
- apply pressure to the affected area;
- engage in self-diagnosis and treatment if bitten by an unfamiliar cat.
You should seek medical help in the following cases:
- heavy bleeding;
- multiple bites;
- when feeling unwell;
- the appearance of inflammation;
- bite in the face or neck area.
If you are scratched by a cat
If you are bitten by a domestic cat that has not been exposed to other animals for the past two weeks, you can refuse the vaccine.
The rabies virus is not transmitted through cat scratches. The exception is a wound that has received saliva from a sick animal. If a domestic cat is vaccinated, there is no chance of contracting rabies.
But through cat scratches, Bartonella bacillus, staphylococcus and streptococcus enter the human body.
In case of injury, the following precautions must be taken:
- wash the wound with warm water and laundry soap;
- treat the wound with antiseptic solutions (chlorhexidine, miramistin, hydrogen peroxide);
- apply a sterile, loose bandage;
- Observe the scratch; in case of inflammation or suppuration, consult a surgeon.
Other routes of infection and precautions
The main route of infection with rabies is through the bite of a sick animal.
The main route of infection with rabies is through the bite of a sick animal.
But other routes of infection are extremely rare:
- Through wounds on the skin. For infection to occur, a sick cat must lick a human wound. Without this, infection will not occur.
- During the autopsy of the body of an infected animal.
- From a person with rabies through clothing, water, or by airborne droplets.
To prevent the spread of the virus, veterinary services are taking measures to exterminate carriers of the infection and destroy the bodies of sick animals.
Domestic cats and dogs are vaccinated against infection.
To prevent infection, city residents must follow the following rules:
- vaccinate your cat according to the vaccination schedule;
- do not let pets go outside alone;
- In case of animal bites, contact a surgeon or a hospital emergency room.
Incubation period after rabies infection
In cats, manifestations of the disease begin on the 10th day, sometimes a little later. The animal behaves as usual or becomes restless and looks for a secluded place. After 2 weeks, the cat becomes aggressive and drooling increases.
Be sure to read:
Colds in cats: symptoms and treatment, causes of the disease, how to determine whether it is transmitted to humans
In humans, the asymptomatic period lasts longer, reaching several months.
Time is determined depending on factors:
- age;
- bite site;
- size of the animal;
- the ability of the nervous system to resist the virus.
In children, the disease manifests itself faster than in adults. A bite to the upper torso reduces the time of brain damage. Small animals leave less virus in the wound.
What to do after a cat bite
If the cat's teeth have not pierced clothing or reached the skin and the victim of the attack feels well, there is no need for medical attention. If tissue injury occurs, it means that the animal’s saliva has gotten under the skin and the victim must:
- Treat the bite site.
- Go to the emergency room (it would be a good idea to take your immunization card with you).
- If possible, catch the attacking cat, place it in a closed carrier and take it with you to a medical facility (observing the animal will allow you to quickly and accurately determine the possible consequences of the bite).
What to do if bitten by a cat
After a cat bite, the wound should be washed, treated with a disinfectant solution and seek medical help at the nearest medical facility.
If the cat scratched
The procedure is the same as after a bite. Most zoonotic infections live not only in saliva, but also on the claws of the animal. And saliva from a cat infected with rabies or tetanus easily penetrates damaged skin.
First aid
If you are bitten by a cat, especially a stray one, immediately treat the injured area. Timely and competent first aid will reduce the risk of infection, if infection occurs, and will slow down the spread of pathogenic microorganisms.
In case of slight bleeding, wait until the cat saliva is removed from the wound along with the blood (this will neutralize most of the pathogenic bacteria and speed up the recovery process). And only after that proceed to first aid:
- Prepare a soap solution (20%): grate a third of a bar of gray laundry soap and a piece of toilet soap on a fine grater.
- Dissolve the resulting powder until smooth in 500 ml of warm water.
- Wash the wound with cooled soapy water for 15 minutes. If the skin is simply scratched, 5 minutes is enough. An alkaline environment does not allow bacteria into deep tissues.
- Apply Levomekol antibacterial ointment to the wound or rinse with chlorhexidine. Fill deep skin damage with 3% hydrogen peroxide, iodine or medical alcohol (you can use vodka or furatsilin).
- Cover the wound with a clean bandage and secure (not tightly).
- To relieve pain, wrap ice in a waffle towel and apply to the bandaged wound.
If the wound is bleeding profusely, raise the affected limb to chin level and press down on the damaged vessel with your finger. As soon as the bleeding stops, proceed to the measures described above.
Errors in first aid
- forced cessation of minor bleeding;
- covering the affected area with an adhesive plaster;
- cauterization or self-suturing of the bite;
- neglect of medical care.
Treating the wound with medications
To treat a cat bite, you will need medications that can be found in any home medicine cabinet:
- hydrogen peroxide;
- iodine;
- medical alcohol;
- chlorhexidine solution or Miramistin;
- Vishnevsky ointment, tetracycline or Levomekol.
Antibiotics
If you get bitten by a cat, especially a stray one, be prepared to take antibiotics. Infections cannot be cured without antibiotic therapy.
Broad-spectrum drugs that kill most known pathogens are often prescribed: Ceftriaxone, Amoxiclav, Doxycycline, Biseptol. The duration of treatment is from 5 to 21 days.
How is the treatment carried out?
If a domestic vaccinated cat has bitten and all first aid requirements have been met, there is no need to visit a doctor and further treatment. After an attack by an unfamiliar animal, life-saving treatment is as follows:
- Tetanus vaccination (if more than 5 years have passed since the last vaccination).
- Administration of anti-rabies serum (to prevent the spread of the rabies virus).
- Taking antihistamines (to stop the development of an allergic reaction, relieve itching at the site of the bite).
- Taking broad spectrum antibiotics.
- Regular treatment of the bite site.
Surgical removal of dead tissue, sanitization, oxygenation of the wound and suturing are required in the following cases:
- head or neck injury;
- due to the violation of the vascular walls, severe bleeding began;
- death of the wound surface (in advanced cases).
Home treatment using pharmaceutical drugs
If the condition of the bitten person does not cause concern and does not require immediate hospitalization, treatment of the cat bite is carried out at home. After examining the wound surface and receiving test results, the doctor prescribes pharmaceutical drugs:
- Antiseptics destroy pathogenic microorganisms and protect against infection: Miramistin.
- NSAIDs to relieve inflammatory symptoms and inflammation itself: Ibuprofen, Ketoprofen.
- Glucocorticoids (hormones) stop the inflammatory process when the infection is widespread: Medipred, Prednisol.
- Antibiotics in the form of ointments on the wound surface: “Levomekol” and in the form of injections when the body is infected: “Amoxiclav”. Be sure to combine the use of antibacterial drugs with Bifiform or Linex, intended to preserve intestinal microflora.
- Diuretics to remove excess fluid during severe swelling: Furosemide. To prevent important microelements from being “washed out” of the body, Asparkam should be taken simultaneously with a diuretic. Otherwise, problems with joints and bones will begin.
- Pharmacy analgesics will help to cope with pain during the first day: “Tempalgin”, “Baralgin”.
- Antihistamines will relieve swelling and itching from the bitten area: Suprastin, Loratadine.
Medicines to relieve swelling
If the hand is swollen far beyond the bite, it will not be possible to stop the spread of infection without antibiotics. To relieve swelling, the doctor prescribes injections of antibacterial agents into the inflamed area. Suitable for indoor use:
- "Amoxicillin";
- "Lincomycin";
- "Klavunat";
- "Ceftriaxone".
Swelling subsides after 5–10 days, provided that the prescribed drug is taken daily. If swelling is accompanied by severe pain, the patient is placed in a hospital under the close supervision of doctors.
A remedy to relieve the condition before visiting a doctor
When the bite site is swollen, but a visit to the doctor is postponed for some reason, a special bandage that slows down the spread of infection throughout the body will help alleviate the condition.
After washing the wound with a solution of laundry soap, apply a bandage generously soaked in Levomekol or other antibacterial ointment and alcohol. Every 4-6 hours, moisten the bandage with alcohol and reapply.
Result:
- The pores will open.
- The ointment will penetrate the affected tissues faster and the heat at the site of swelling will subside.
- Secure your hand in a sling.
This temporary treatment option is not used for longer than 48 hours or for conditions that can be treated without the help of a surgeon.
Folk remedies and recipes from healers
After a bite from a domestic cat, when the risk of contracting rabies or tetanus is minimized, you can stop the inflammation using traditional medicine recipes. Already on the second day of active treatment, the pain goes away, the wound dries up and begins to heal. Consider popular recipes:
- 1 tbsp. lie Pour chamomile, sage, calendula and eucalyptus into a container and pour 200 ml of boiling water. Wrap in a terry towel and wait until it cools down. Apply a gauze pad soaked in the infusion to the wound and secure it. Repeat herbal lotions 3-4 times a day.
- Swelling caused by infection and the development of a purulent process is treated with aloe leaves. But only if the outbreak is small. Place the cut leaf with the fleshy side on the wound and secure. Vishnevsky ointment or “ichthyolka” are no less effective in drawing out pus from a cat bite.
- The soda-saline solution draws pus from a moderately swollen arm and cleanses the wound. Dissolve 2 teaspoons in 200 ml of cool water. soda and salt, immerse your hand there and hold for about 20 minutes. Repeat three times a day.
Despite the natural ingredients, healers’ recipes can be harmful if the following conditions are not met:
- agreement with the doctor;
- exclusion of infection with tetanus bacillus or rabies virus;
- combination of folk recipes with pharmaceutical drugs.
Dog incubation period
Rabies is a viral disease associated with inflammation of the brain.
The incubation period of the disease directly depends on:
- size of the infected person;
- location and depth of the bite;
- the health status of the bitten person.
The smaller the animal, the faster signs of rabies appear.
In children, the disease develops in a shorter period of time compared to adults. The development of the virus occurs faster in the case of damage to the neck, face, and head. Accordingly, when extremities are bitten, the incubation period increases.
The incubation period for human infection is up to 3 months. Wounds in the head area significantly accelerate the development of the disease. Cases have been recorded where symptoms appeared within a week after the attack. If the extremities are affected, the virus may not manifest itself for up to 1 year. There have been cases where the disease entered the active stage after 2-3 years.
At the moment, it is known that the virus remains dormant for 6 years. It was recorded in an emigrant who arrived in America from the Philippines.
The incubation period can be short (several days), but it can be quite long - several months
In animals, the timing of the development of the disease differs slightly from that in humans. The incubation period ranges from 10 to 21 days. With shallow lesions and good immunity of adults, symptoms appear after 5-9 months.
Rabies is a virus for which treatment is powerless.
Only relief of the patient's condition is possible. The disease is transmitted when the epidermis is injured and salivary fluid penetrates the surface of the wound. In other cases, the likelihood of spread is minimal. Professional help and vaccination can prevent the development of the disease.
What not to do
It is unacceptable to use antiviral drugs in the treatment of bacterial diseases (treatment suitable for one case may have a detrimental effect in another). This rule also applies to the treatment of a cat bite.
Mistakes in home treatment
- Warming up the bite (inflammation intensifies, the spread of infection accelerates).
- The use of healing agents on a contaminated wound (lack of sanitation leads to deepening of the lesion and the development of a purulent process). Even if a cat bites your finger, you can lose your hand.
- Open an abscess at home.
If the situation is out of control and inflammation progresses, do not experiment with your health. It is better to seek medical help immediately.
Cases when you need to see a doctor right away
Sometimes a cat bite leads to conditions that are impossible to cope with without the help of a specialist. Let's take a closer look at them.
Urgent actions
Only a qualified doctor can treat the following conditions without harm to the patient’s life:
- it is obvious that the animal is infected with rabies;
- a child, pregnant woman or elderly person was injured;
- the infection is developing rapidly;
- the injured limb hurts unbearably;
- the victim lost consciousness;
- convulsions and trembling in the limbs appeared;
- an acute allergic reaction develops (the victim has difficulty breathing, the face swells, etc.);
- large deep wound with heavy bleeding;
- the patient has a fever, his general condition quickly deteriorates.
Deep bite
The deeper the bite, the greater the likelihood of infection in the body.
Bleeding
Severe, prolonged bleeding indicates damage to the artery. A dangerous sign that requires urgent stitches is a pulsating stream of blood.
Bite on the face or hands
If the face or arm is injured, therapy should be started as soon as possible. An advanced stage of inflammation will lead to an enlargement of the lesion and the formation of noticeable scars after the wound heals.
Attention! Never leave domestic cats alone with small children!
Bitten by a street cat
The greatest danger comes from stray cat bites. Here you cannot do without the help of a doctor and a detailed examination. The process of identifying the type of microbe can take a long time, because it is not known what the attacking animal is sick with. So, you shouldn’t delay visiting the emergency room, because with some “feline” infections the days count.
Vaccination
Tetanus and rabies are the most terrible complications of a cat bite, requiring urgent immunization.
Rabies vaccine is administered in an amount of 1 ml on days 1, 3, 7, 14, 28. No later than 10 days from the moment of the bite. For adults in the shoulder, for children under 5 years old - in the hip.
Anti-tetanus serum must be administered after a street cat bite or when the previous vaccination has expired. Emergency administration of a prophylactic drug is prescribed within 6–8 hours after the bite. If more than 48 hours have passed since the bite, administering the serum is not advisable.
Rabies
Measures to prevent rabies in animals include regulating the density of wild animals; catching stray dogs and cats; compliance with the rules for keeping domestic dogs (registration, use of muzzles, keeping them on a leash, etc.); mandatory annual preventive immunization against rabies in dogs. A course of preventive immunization is carried out for persons professionally associated with the risk of contracting rabies (dog catchers, commercial hunters, veterinarians, etc.).
Dogs, cats and other animals that have bitten people or animals must be immediately delivered by the owner to the nearest veterinary hospital for examination and quarantine under the supervision of specialists for 10 days. The results of such observation of animals are reported in writing to the medical institution where the affected person is vaccinated. If the animal does not die during the observation period, then it is probably healthy.
Nonspecific prevention The best preventive measure is local wound treatment. The bite area should be immediately thoroughly cleaned with a 20% solution of mild medical soap. Deep bite wounds are washed with a stream of soapy water using a catheter. Cauterization of the wound or suturing is not recommended.
Specific prevention (immunoglobulin + vaccine) The best specific prevention is passive immunization with rabies immunoglobulin or rabies serum followed by active immunization (vaccination). Passive and active immunization are carried out simultaneously, but different drugs cannot be administered to the same place.
Indications for vaccination against rabies General secondary prevention (vaccine prophylaxis) begins immediately for: - all bites, scratches, salivation of the skin and mucous membranes caused by clearly rabid, suspected rabies or unknown animals; - when injured by objects contaminated with saliva or brain of rabid or suspected rabid animals; - when bitten through clothing if it is damaged by teeth; - when bitten through thin or knitted clothing; - when biting, salivating and scratching a healthy animal at the time of contact, if it became ill, died or disappeared during a 10-day observation; - when bitten by wild rodents; - in case of obvious salivation or damage to the skin of a person with rabies.
When vaccination against rabies is not necessary Vaccinations are not carried out: - for bites through intact thick or multi-layered clothing; - when injured by non-predatory birds - when bitten by domestic mice or rats in areas where rabies has not been recorded in the last 2 years; - accidental consumption of thermally processed meat and milk of rabid animals; - if the animal remains healthy within 10 days after the bite. - when bitten by an animal 10 days or more before their illness; - in case of salivation and bites of mild and moderate severity caused by animals that were healthy at the time of the bite, with favorable data (rabies does not occur in the area, the animal is kept in isolation, the bite was provoked by the victim himself, the dog is vaccinated against rabies). However, in this case, the animal is subject to 10-day veterinary observation in order to begin vaccinations if it shows signs of rabies, as well as death or disappearance; — in case of provoked salivation of intact skin by an unknown domestic animal in rabies-free areas; - in cases of contact with a person with rabies, if there was no obvious salivation of the mucous membranes or damage to the skin.
Rabies vaccination procedure Active immunization begins immediately. The vaccine is administered intramuscularly, 1 ml 5 times: on the day of infection, then on the 3rd, 7th, 14th and 28th day). This regimen always creates satisfactory immunity, so routine serological testing is not recommended. WHO also recommends a 6th injection 90 days after the first.
Adverse reactions of the rabies vaccine There may be mild reactions at the injection site in the form of soreness, swelling and induration. In some cases, these reactions may be more severe. In addition, there may be an increase in temperature to 38 degrees Celsius or higher, enlarged lymph nodes, arthritis and dyspeptic disorders. Sometimes headache, general malaise, chills, myalgia and allergic reactions are observed.
Special instructions Vaccinations against rabies are carried out both on an outpatient and inpatient basis. Persons with severe bites living in rural areas are subject to hospitalization; re-vaccinated; persons with diseases of the nervous system or allergic diseases; pregnant women, as well as persons vaccinated with other drugs during the previous two months.
Corticosteroids and immunosuppressants may suppress the immune response to the vaccine. Therefore, if vaccination is necessary while taking these drugs, determining the level of antibodies is mandatory to decide on an additional course of treatment
During vaccinations, it is necessary to monitor the patient's health status. If there are complaints of deterioration of the condition, hospitalization is necessary, and vaccinations are temporarily suspended. The victim should be examined by a neurologist and therapist. The issue of continuing or stopping vaccinations is decided in consultation with a neurologist, radiologist and therapist.
In order to ensure proper immunity and prevent post-vaccination complications, the use of any alcoholic beverages during the vaccination course and for 6 months after its completion is contraindicated for those vaccinated. It is necessary that during the vaccination period the patient does not overwork and avoid hypothermia and overheating. In some cases, it is recommended to transfer to easier work or issue sick leave.
The use of other vaccines simultaneously with rabies is not allowed. However, if necessary, emergency tetanus prophylaxis can be carried out. People with rabies are not vaccinated.
Tips for preventing cat bites
To eliminate the risk of a cat bite, follow these rules:
- Do not interact with unfamiliar cats.
- Do not force affection on your pets.
- Do not take away or interfere with food intake.
- Do not take kittens from a nursing cat.
- Train your cat from a young age.
- Provide your cat with a scratching post and teeth-sharp trainers.
- Don’t skip scheduled vaccinations (yours and your pet’s), have him examined and treated promptly by a veterinarian.
Vaccinating cats against rabies: when to vaccinate
There is no cure for rabies. The only way to avoid the disease is timely vaccination. The vaccination is given to a kitten at the age of 3 months.
The animal must be healthy. 2 weeks before the injection, the kitten must be given anthelmintic drugs.
Vaccines that have proven positive:
- Rabikan;
- Quadriket;
- Leucoriphenin;
- Nobivak.
Be sure to read:
Viral and infectious peritonitis in cats: deadly coronavirus, how long do they live with FIP
They are easily tolerated by cats and do not cause discomfort. Before the first vaccination, contact of the animal with sick individuals should be avoided.
It is not advisable to let your cat outside. Vaccinations in Russia are provided free of charge in state veterinary clinics.