Frontal syndrome is a clinical symptom complex that occurs primarily with bilateral damage to the frontal lobes of the brain. The components of the syndrome are disorders of praxis, emotional-volitional sphere, behavior, possible disturbances in speech, posture and walking. It is diagnosed based on clinical data, and the nosology is verified using cerebral neuroimaging (CT, MRI) and cerebral circulation studies. Therapeutic tactics for frontal symptom complex are determined by the etiology of the lesion and may include drug therapy (prescription of vascular, neuroprotective, psychotropic drugs), neurosurgical treatment (removal of a tumor, hematoma) followed by rehabilitation.
General information
Active study of the frontal (frontal) parts of the brain began in the 70s of the 19th century. Researchers in this area have encountered a number of contradictions. It turned out that “switching off” the frontal lobes is not accompanied by a gross disorder of the motor, sensory, and reflex spheres, which led some scientists to the conclusion that there is no certain functional significance of these cerebral structures. Subsequent study of the issue revealed significant changes in behavior and psycho-emotional sphere with damage to the frontal zones of the cortex, which made it possible to attribute the latter to the apparatus responsible for the implementation of higher mental functions. This statement is confirmed by the significant development of the frontal parts of the human brain in comparison with the animal brain.
Flow options
Depending on which part of the frontal part of the brain is affected, neuropsychologists distinguish different variants of frontal syndrome.
Pathologies of convexital sections
The convexital sections lie on the surface of the frontal lobe cortex. These include premotor and prefrontal areas. The syndrome in question is 90% caused by their damage. Profound personality changes occur due to the fact that it is from here that numerous two-way connections come from the cortical and subcortical structures of the entire brain as a whole. They directly contact the motor and speech areas. That is why motor and verbal impairments are so pronounced. A person cannot perform a chain of sequential actions and formulate detailed statements. In neuropsychology, this condition is called dynamic aphasia.
Each convexital region has its own syndrome:
- Premotor
It manifests itself as motor awkwardness, expressed in a change in the usual handwriting, as the automation of the actions performed disintegrates. Dysarthria and acalculia are observed. If the remaining areas of the frontal lobes are not damaged, goal setting and motivation may not be affected and remain, but the operational aspect of carrying out activities is impaired. In neuropsychology, this phenomenon is called the loss of smoothness of “kinetic melodies.”
- Prefrontal
Compared to premotor syndrome, more global disturbances occur here in the area of motivational, goal-oriented, conscious activity. This manifests itself in a lack of desires, criticism, verbal instructions, and self-reflection. The person becomes passive, inert. The program of his actions is simplified as much as possible, and a transition to stereotypes is observed.
- Areas lying "anterior to the premotor area"
Pathology is an intermediate link between the previous two. Motor functions are slightly impaired. In behavior, deviations manifest themselves in the form of lethargy, spontaneity, adynamicity, and inactivity. People with this diagnosis cannot switch from one action to another, get stuck on one thing, and are unable to solve intellectual problems.
Pathology of the mediobasal regions
- Basal (orbital)
The syndrome of damage to the basal parts of the frontal lobes is considered one of the most severe, since this area is closely connected with the structures of the First block of the brain and the neural structures of the thalamus. The result is disinhibition of mental processes, pronounced changes, hypertrophy of feelings, premonitions, desires, impulses, impressions, and experiences.
- Medial
There is a violation of neurohumoral regulation. A person loses the ability to navigate in space and time, cannot concentrate attention on one thing, entire fragments of life fall out of memory, suffers from false memories, illusions and confusion.
Causes of frontal syndrome
The frontal zones of the brain are considered the youngest and less differentiated cerebral regions with high interchangeability of components, therefore, pronounced frontal syndrome is observed only with extensive bilateral damage. The cause of pathological changes are:
- Traumatic brain injuries . Injuries to the frontal zones in TBI are quite common and are the result of a blow to the forehead or a counter-impact in a trauma to the back of the head. Post-traumatic intracerebral hematomas cause compression of cerebral tissues, epi- and subdural hematomas cause compression of the cortex. Direct damage to neurons and interneuronal connections occurs with brain contusion.
- Strokes. The blood supply to the frontal lobes is carried out by the anterior and middle cerebral arteries. Impaired blood flow through these vessels or their branches causes the development of ischemic stroke - neurons die due to acute hypoxia. When the vessels of this pool rupture, a hemorrhagic stroke occurs with hemorrhage into the brain tissue.
- Vascular anomalies . Arteriovenous malformations are dangerous due to local expansion of the vessel, thinning and breakthrough of its wall. The blood released as a result of the rupture is organized into a hematoma. As the latter increases, compression and death of neurons occurs, causing frontal syndrome.
- Tumors. Growing into the frontal tissues, cerebral neoplasms cause their destruction and/or compression. The function of the frontal neurons is gradually lost. Clinically, the frontal symptom complex manifests itself when the tumor is large and spreads to the opposite lobe.
- Degenerative diseases. Progressive atrophic processes with damage to the frontal regions are observed in Pick's disease, frontotemporal dementia, and corticobasal degeneration. Frontal dysfunction occurs as a result of degenerative changes and subsequent apoptosis of nerve cells, their replacement by glial and connective tissue elements.
Pathogenesis
The frontal regions perform integrative and regulatory functions that provide complex behavioral reactions, programming and implementation of a sequence of actions. Damage to the structures of the frontal lobes, their connections with other cerebral parts leads to the collapse of conscious active activity - ideational apraxia. Complex actions are replaced by simpler, habitual, automated, uncontrollably repetitive ones. The ability to evaluate the result of an action is lost, and there is no motivation.
Side effects are disinhibited and there is no goal-directed behavior. Impulsivity of reactions and violation of control cause antisocial behavior. Damage to the posterior frontal parts of the dominant hemisphere leads to the development of dynamic aphasia, and Broca's center leads to the development of efferent motor aphasia. Extensive damage to the frontal lobes is accompanied by a violation of cortical coordination of skeletal muscle tone, which leads to a loss of coordination of muscle contractions necessary to maintain posture and movements.
Problems
One of the specific behavioral disorders after damage to the frontal lobe is attention disorder; patients exhibit distractibility. They are characterized by poor memory, sometimes called “forgetting to remember.” Their thinking is concrete, they show persistence and stereotyping.
Learn more Symptoms, signs and treatment of Lejeune's syndrome (cry of the cat)
Persistence, with an inability to move from one line of thinking to another, leads to difficulty with arithmetic calculations such as successive sevens or subtraction.
Aphasia is sometimes observed, but it is different from Wernicke's and Broca's aphasia. Luria called it dynamic aphasia.
Other features of frontal syndrome include decreased activity, inability to plan, and lack of restlessness. Sometimes this is associated with bouts of restless, aimless, uncoordinated behavior.
The patient shows indifference to the outside world. Clinically, the picture resembles a serious affective disorder with psychomotor retardation.
Euphoria and disinhibition are sometimes described. Euphoria does not refer to a manic state. Disinhibition leads to pronounced deviations in behavior, sometimes associated with outbursts of irritability and aggression.
Classification
The frontal lobe includes several zones with different functional purposes. The predominance of one or another frontal symptom complex depends on the location of the lesion. This criterion formed the basis of the classification used in clinical neurology, according to which frontal syndrome is divided into:
- Apraxic. It is determined by damage to the premotor cortex. The clinical picture is dominated by disorders of the organization of complex movements and actions; articulation disorders (dysarthria) and acalculia occur secondarily.
- Apatico-abulic. Observed in pathology of the convexital zones of the prefrontal region. The clinic is dominated by lack of initiative, apathy, and lack of will (abulia). Characterized by a lack of interests, desires, and inability to initiate any action aimed at satisfying basic needs.
- Mental disinhibition syndrome. Develops during pathological processes in the mediobasal regions of the frontal lobe. Typically disinhibited behavior without taking into account social and ethical norms, logorrhea, carelessness, foolishness, and sometimes aggressiveness.
Frontal lobe
According to T.I. Yudin (1941), when the frontal lobes of the brain are removed, a person loses the ability to navigate new complex situations and make new plans for the future, which is somewhat reminiscent of symptoms quite typical of schizophrenia. T.I. Yudin believed that the frontal lobes contain mechanisms through which the future is planned. Modern neuropsychological studies show that damage to even both frontal lobes may not be accompanied by either aspontaneity or changes in temperament, but it does reduce the patient from his creative level.
| | MRI allows you to diagnose changes in the size of the frontal lobe, and you can track brain activity in these areas using EEG |
In 1974, K. Ingvar and T. Franzen showed that patients with schizophrenia have a decrease in the volume of blood flow in the frontal lobes of the brain. Insufficient blood supply (hypofrontality) of the frontal lobes was so noticeable in patients with schizophrenia with severe mental disorders that it allowed us to talk about a special “hypofrontality phenomenon” in schizophrenia.
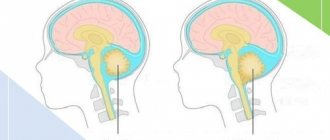
Frontal lobe changes in schizophrenia
- The phenomenon of hypofrontality (reduced blood flow in the frontal lobes of the brain)
- Reduction of volumes of the anterior cingulate, orbitofrontal, dorsolateral and ventromedial cortices
- Disruption of connections between the frontal lobes and deep brain structures
- Disruption of connections between the anterior parts of the right and left hemispheres
Using MRI slices in schizophrenia, decreased volumes of the anterior cingulate, orbitofrontal, dorsolateral and ventromedial cortices were found.
In other studies, on the contrary, hyperfrontality was identified, but such data were found significantly less than the results indicating a decrease in the functional activity of the frontal cortex, especially in schizophrenia with severe negative symptoms.
Recent studies have shown that in patients with schizophrenia, connections between the frontal lobes and much deeper brain structures are weakened. The cause of these changes is likely due to either increased activity of these brain structures or suppressed activity of the frontal cortex.
Many psychopathological syndromes that are observed in schizophrenia probably have their own pathoanatomical substrate, most likely manifesting itself at the level of the relationship between certain brain structures, for example, along the main pathways of the ascending dopaminergic tract: mesocortical, nigrostriatal, mesolimbic.
Some authors, noting anomalies in schizophrenia, associate them with a violation of cell migration from the cortical plate to the gray matter of the cortex during the process of brain maturation in ontogenesis.
This assumption is partly confirmed by research in the field of neuropsychiatry. Anosognosia and symptoms of depersonalization, which in some cases occur in schizophrenia, can be explained by predominant damage to the right hemisphere of the brain.
The clinical picture of damage to the left frontal lobe is characterized by aspontaneity, up to “paralysis of initiative,” a decrease in emotional experience regarding oneself and the world around (Bely B.I., 1987).
In addition to anosognosia, lesions of the right frontal lobe are characterized by fragmented perception with a tendency to interpret the entire proposed picture as a whole on the basis of randomly perceived individual episodes, uncriticality of one’s own mistakes, false recognitions, instability of attention, absent-mindedness, slipping into unrelated topics, difficulty switching attention, exhaustion, tendency to stereotypes. At the same time, the range of symptoms of damage to the right frontal lobe also includes other symptoms: confabulatory additions to what is perceived, mobility, verbosity, familiarity. The second group of symptoms, although found in schizophrenia, is recorded less frequently than the first. It is a fair assumption that the degree of anatomical damage to the right frontal lobe in schizophrenia is not as total as in tumors of this area of the brain, where both groups of symptoms are often noted in the clinical picture of the disease.
In the initial stages of the malignant variant of the course of schizophrenia, one can detect symptoms quite characteristic of damage to the basal-frontal regions: inadequacy of emotional reactions, verbosity, sloppiness, increased appetite (Sternberg E.Ya., 1967).
In schizophrenia, thinking is impaired, the ability to plan actions is weakened, and there is difficulty solving problems, which may indicate damage to the frontal lobe of the brain.
Symptoms of neurocognitive deficits and negative symptoms, as a rule, are more pronounced where there is damage to the frontal lobe of the brain, an indirect sign of which can be considered the expansion of the subarachnoid spaces around some areas of this lobe. According to our observations, the severity of delirium and lack of criticism of one’s condition are more noticeable in those patients who demonstrate changes in the frontal lobe of the brain when studied using modern neuroimaging methods.
The frontal lobes have been found to be involved in initiating actions. Response suppression, in turn, depends on interactions between the frontal cortex and the underlying areas of the brain that process sensations.
Some researchers believe that impaired functioning of the frontal lobe in schizophrenia is associated with a deficiency of dopamine, others speak of insufficient glutamatergic activity in this area of the brain.
It is interesting to note that with exacerbation of paranoid symptoms, there is an accumulation of dopa in the striatum. However, at present, the relationship between the concentration of dopa decarboxylase and dopamine synthesis remains unclear, since there is no direct relationship between them. At the same time, insufficient activation of the prefrontal cortex during the Wisconsin test is accompanied by the accumulation of dopa in the striatum. As a result of the above, it can be assumed that in schizophrenia, dysfunction of the frontal lobes is correlated with excessive activation of dopaminergic structures in the striatum.
In the frontal cortex, dopamine is considered a neurotransmitter that enhances the activity of neurons (D1 receptors), and increased activity of the glutamatergic system tends to enhance the activity of the dopaminergic system. Because of the above, a lack of glutamate in the frontal lobe of the brain may also contribute to increased negative symptoms and manifestations of neurocognitive deficits. A decrease in the severity of negative symptoms in schizophrenia as a result of taking atypical antipsychotics is also associated with changes in the activity of the serotonergic system of the brain.
In schizophrenia, neuropsychological studies indicate a disruption of the relationship between the anterior parts of the brain hemispheres.
Usually a normal person can control his actions (“model of subsequent message”), as if dosing their intensity; in schizophrenia, this process is disrupted.
Patients with mental automatism syndrome do not detect differences in time, manipulation of handling both small and larger objects. Let us recall that normally, when a person operates with smaller objects, his movements become slower.
Suppression of responses to sensations that a person induces through his actions occurs under the influence of signals coming from areas of the brain associated with the formation of actions.
Return to Contents
Symptoms of frontal syndrome
A mild degree of damage is manifested in a decrease in the patient’s interests, his inattention, and inactivity. Isolated frontal syndrome is not accompanied by paresis or sensory disorders. Habitual simple actions are completely preserved; difficulties arise when it is necessary to perform a complex multicomponent action or a given sequence of movements. Purposeful activity is interrupted by side impulsive actions. For example, seeing a bell button, the patient unconsciously presses it, implementing a habitual movement under the influence of a momentary impulse. Similarly, when cooking soup, the patient can put any inedible object that comes to hand into the pan.
Characteristic is “getting stuck” (perseveration) on performing a certain action: repeating a question, reading the same phrase, repeatedly squeezing a given hand, etc. The most demonstrative perseverations are when trying to draw a series of geometric figures according to a model. The first 2-3 figures can be displayed correctly, then the last figure is repeated. With more severe violations, an attempt to draw a circle leads to repeated repetition of the action with the loss of the ability to stop it independently.
With significant pathological processes, frontal syndrome occurs with astasia - a violation of the ability to maintain a certain body position (standing, sitting), abasia - the inability to walk. At the same time, in the prone position, movements are preserved in full. Disinhibition of oral automatisms is often observed, leading to the appearance of constant smacking and stretching of the lips with a tube. A grasping reflex is noted: the patient squeezes an object placed in his palm into a fist.
Severe apathetic-abulic syndrome is accompanied by a profound breakdown of voluntary motor activity. Patients are unable to initiate action, for example, when thirsty, they cannot make a request or take a nearby glass of water. Active speech is sharply reduced, answers to questions are monosyllabic, echolalia (repetition of the interlocutor’s phrases) is typical. A distinctive feature is the impossibility of both starting and stopping movement. Patients do not take the object offered to them; when placing it in their hand, they squeeze it tonically or repeatedly, unable to stop the action they have started. The automatic repetition of a motor act determines the tendency of patients to constantly fiddle with the edge of the bed, scratch the wall next to the bed, and fidget with their fingers.
Mental disinhibition syndrome is characterized by increased agitation, excessive speech production, and motor activity. Actions are aimed primarily at satisfying biological needs; there are no moral and ethical restrictions. Patients are euphoric, constantly making jokes, making puns, and fooling around. Behavior is often devoid of common sense and can be antisocial and aggressive. There is no criticism of one’s own condition.
Complications
The lack of a critical attitude towards one’s condition and susceptibility to impulsive actions causes social maladjustment and requires that the patient be under constant control from loved ones. Apathetic-abulic frontal syndrome in the absence of proper care leads to exhaustion of the body. Astasia-abasia syndrome is accompanied by repeated falls that injure the patient and force him to lie in bed. Bed patients are susceptible to the formation of bedsores, the addition of intercurrent infections with the risk of developing septicemia.
Violations of psychophysiological functions
Perceptions
Impaired perception occurs when performing complex tasks that require active activity. The patient cannot analyze the stimulus and acts either accidentally, impulsively, or formally, in accordance with stereotypes. For example, he cannot perceive shades of primary colors. Even if you tell him in detail about emerald, mint, turquoise, olive, in the end the person will say that all this is green.
Movements and actions
There is an inability to plan and implement a conscious program of activities. Even outside instructions cannot correct the situation. With such a diagnosis, difficulties arise not only with drawing up a plan, but also with retaining it in short-term memory. The result is uncontrolled, unconscious, impulsive actions. Sometimes patients automatically perform the skills that they acquired earlier, but they do it reflexively. They don't see their own mistakes.
Attentions
Attention impairment manifests itself in the inability to concentrate on something, absent-mindedness, and constant distraction to external stimuli.
Memory and speech
Speech and memory with frontal syndrome are also seriously impaired. Mnemonic abilities are minimized. The patient does not remember information well and can only reproduce what was said (seen) last. When repeating, frequent errors occur due to attention disorders. They are not noticed and, accordingly, are not corrected. A person can remember well the material that he learned before the disorder, but he can reproduce it only unconsciously, without any purpose.
Due to social maladjustment, speech skills that were previously acquired are lost. There is an inability to formulate clear statements of complex structures and speech spontaneity.
Thinking
The patient does not remember the final question and the conditions of the task, and in the absence of a motive does not strive to complete it. Grabbing some fragment, he begins to work with it, performing completely different actions than necessary. A striking example. 2 pictures are given. One complete, complete. The second is her unfinished cast. Assignment: complete the second one in the likeness of the first. A person with such a disorder may begin to color the first or finish the second, but in a completely different way. Or, when solving a distance problem, instead of multiplying the speed by the time, he adds them up and then cannot explain why he did this.
Emotional-personal sphere
Violations in this area are the most striking manifestations of the disease. Inappropriate attitude towards oneself and others, unbridled joy, childish antics, and indifference are diagnosed. Lost interest in family, hobbies, and work. Damage to the right lobe is accompanied by euphoria, anger, and aggression; left - lethargy, inactivity, lethargy and depression, depression.
Diagnostics
Diagnostic difficulties are due primarily to the mental nature of the clinical manifestations of the disease. Apathetic-abulic states resemble depression, mental disinhibition resembles the manic phase of bipolar disorder. Observing changes in the patient’s personality and behavior, relatives often initially turn to a psychiatrist, who refers the patient to a neurologist. Neurological examination includes:
- Assessment of neurological status . Behavioral disturbances, difficulties in performing several consecutive movements according to instructions, perseveration of one of the indicated movements, mirror image when performing the Head test (copying the posture of the doctor’s hands) are noted. Possible astasia in the Romberg position, gait disturbance, speech disorder. Symptoms of oral automatism and grasping reflex are revealed.
- Neuroimaging. It is of paramount importance in establishing the morphological substrate causing frontal syndrome. CT scan of the brain is more informative in post-traumatic conditions and meningeal hematomas. Cerebral MRI can detect post-stroke lesions, tumors, and degenerative changes in the frontal lobes.
- Cerebral hemodynamics study . It is carried out if a vascular disorder is suspected. It is carried out using Doppler ultrasound, MRI, duplex scanning of cerebral vessels. Identifies areas of chronic cerebral ischemia, localization and nature of blood flow disturbances (spasm, thromboembolism, aneurysm, AVM).
Frontal syndrome is a clinical symptom complex that indicates an area of cerebral damage, but is observed in many diseases. To establish a final diagnosis, it is necessary to differentiate frontal symptoms of various etiologies. Peculiarities of the development of the clinical picture and accompanying symptoms help to clarify the nature of the causative pathology. In case of injuries, strokes, frontal symptoms arise acutely against the background of almost complete well-being; in case of tumors and degenerative processes, clinical manifestations gradually increase.
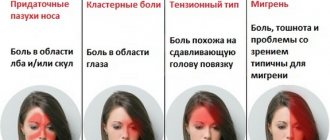
Symptoms
| Occurrence (how often a symptom occurs in a given disease) | |
| Goofiness | 70% |
| Bouts of mood elevation | 60% |
| Self-indifference | 50% |
| Frontal headache (migraine) | 50% |
| Difficulty speaking (speech disorder, speech disorder, speech problems) | 50% |
| Perversion of smell (smells are perceived not in accordance with generally accepted norms) | 50% |
| Olfactory hallucinations | 50% |
| Attacks of seizures with or without loss of consciousness (convulsions, convulsive seizures, convulsions, convulsions) | 50% |
| Vomiting of various types, including indomitable | 50% |
| Nausea | 50% |
| Impaired coordination of movements | 45% |
| Aggressive behavior | 40% |
| Headache that occurs or gets worse in the early morning hours | 40% |
| Numbness of the face | 40% |
| Memory loss (memory impairment, poor memory, memory impairment, forgetfulness) | 40% |
| Gait disturbance (dysbasia, gait disturbance) | 35% |
| Depressed mood | 35% |
| Frequent stumbles and falls | 20% |
| Involuntary grimaces (spasms) of the face | 10% |
| Involuntary movements in the limbs | 10% |
| Transient speech impairment (absence or difficulty speaking during the day) | 10% |
Treatment of frontal syndrome
Therapy is carried out comprehensively, combining etiopathogenetic and symptomatic treatment with subsequent rehabilitation. If necessary, neurosurgeons, speech therapists, psychiatrists, and rehabilitation specialists take part in carrying out therapeutic and rehabilitation measures. Depending on the etiology of the disease, two main methods are used in treatment:
- Medication. For strokes, vascular, thrombolytic, and coagulant therapy are used differentially. For severe mental disorders (excitement, apathy), psychotropic drugs are prescribed. According to indications for intracranial neoplasms, polychemotherapy is carried out. In order to quickly restore nerve tissue in the post-traumatic, post-stroke period, nootropic, neuroprotective and neurometabolic pharmaceuticals are used as maintenance therapy for degenerative diseases.
- Neurosurgical. The indication for surgical treatment is frontal syndrome caused by neoplasia, hematoma, or vascular anomaly. Neurosurgical interventions are carried out with planning of the course of the operation after accurately determining the localization of the formation using MRI or CT. When removing tumors, microsurgical equipment is used to differentiate altered tissues from healthy ones.
Prognosis and prevention
The outcome of the disease depends on the etiology, extent of the lesion, and the age of the patient. In young patients, recovery from TBI and neurosurgical interventions is easier than in older patients. Regression of neurological deficit is facilitated by comprehensive rehabilitation. Progressive degenerative processes and malignant neoplasia have an unfavorable prognosis. Preventive measures consist of preventing exposure to factors that cause pathological changes in the frontal regions. Preventive measures include prevention of head injuries, exposure to carcinogens, and cerebrovascular diseases. Prevention of degenerative processes is difficult because their etiology remains unclear.
| Literature1. Frontal syndrome and its clinical variants in penetrating brain injuries / Kartsovnik I.I. – 1949.2. Acquired epileptic frontal syndrome / Mukhin K.Yu., Golovteev A.L.// Russian Journal of Child Neurology. – 2008.3. Disturbance of emotions due to damage to the frontal lobes of the brain: Abstract of the dissertation / Batova N.Ya. – 1984.4. Post-stroke disorders of higher functions: phenomenology, prognosis, rehabilitation: Abstract of the dissertation / Shakhparonova N.V. – 2012. |
LiveJournal