Concept and types of delirium
The word “delirium” is Latin for “delirium” or madness.” The term was first used in Ancient Rome in the 1st century AD. Delirium is an acute, mostly reversible condition that affects attention, impairs perception, and reduces the level of consciousness. It is worth clearly distinguishing delirium from schizophrenia and bipolar disorder - these are fundamentally different things. An important difference is the treatability of delirium and the mandatory presence of a provoking factor in the anamnesis. The syndrome is a neurocognitive disorder and is considered a pressing medical problem. It is often encountered in medical practice and can lead to the death of a person.
Common types of disorder depending on the underlying cause
- Psychopharmacological.
Caused by taking drugs, mainly psychotropic drugs. Neuroleptics in combination with anticholinergics, antihistamines or beta-blockers can also lead to the condition - Organic.
Triggered by pathology of the nervous system, for example: malignant or benign formation in the brain, subarachnoid bleeding, abscess - Drug or alcohol.
Associated with alcohol (popularly called delirium tremens), opiates, barbiturates, hashish. Often occurs as a withdrawal syndrome - Infectious.
Occurs against the background of pneumonia, infectious brain damage, colds, systemic pathologies - Hormone.
Symptoms are usually associated with a thyroid disorder (hypothyroidism, hyperthyroidism) - Vascular.
Acute reaction to tachycardia or bradycardia, heart failure, anemia, shock conditions - Traumatic.
Due to brain injury - Geriatric.
Geriatrics are conditions characteristic of old people. Delirium of various etiologies is often detected in old age due to a slowdown in the body's metabolic processes - Postoperative.
It is often discovered after bypass surgery or surgical correction of valves. Prolonged stay on mechanical ventilation increases the likelihood of developing the condition.
There are other possible reasons: a sudden change in the environment, urinary retention, recent surgery. A deficiency of certain substances can also lead to aggression and delirium. Most often, this is caused by an insufficient amount of B vitamins. Sometimes a combination of reasons leads to the development of delirium: infection with pneumonia due to alcohol withdrawal, a combination of alcoholic beverages and medications, intoxication due to chronic heart pathologies.
Delirium in old age
Delirium is a common clinical syndrome characterized by confusion and “acute cognitive dysfunction.” The word "delirium" was first used as a medical term in the first century AD to describe mental disorders that occur during fever or head injury. Doctors tried to describe delirium with the following terms: “acute confusion”, “acute cerebral failure”, “toxic metabolic encephalopathy”, etc. Over time, delirium began to be understood as a short-term, reversible syndrome, which is partly acute in its occurrence and flickering in its symptoms.
Clinical experience and recent research have shown that delirium can become chronic or fatal. In older patients, delirium may be a key component in the cascade of events that lead to a downward spiral of “functional decline” and ultimately death.
The overall prevalence of delirium in the general population is only 1-2%. Postoperative delirium occurs in 15%-53% of surgical patients over 65 years of age, and among elderly patients admitted to the intensive care unit, the incidence of delirium can reach 70-87%.
Delirium affects, according to experts, from 14% to 56% of all elderly patients hospitalized in psychiatric hospitals. At least 20% of the 12.5 million patients over 65 years of age who are admitted to U.S. psychiatric hospitals each year have complications during their hospitalization due to delirium.
The causes of delirium are varied and they often reflect the pathophysiological consequences of an acute medical illness, drug effect or complications. In addition, delirium develops due to a complex interaction between various risk factors. The development of delirium often depends on a combination of predisposing, as if background, factors, such as underlying dementia or severe medical illness, and the acceleration of delirium on frequently changing factors, such as the use of sedatives, infections, abnormal test results, or surgery. Among older patients, one of the most important risk factors for delirium is dementia (two thirds of all cases of delirium in this age group occur in patients with dementia). Research has shown that delirium and dementia are associated with decreased cerebral blood flow or metabolism, cholinergic deficits, and inflammation, and these similar etiologies may explain the close relationship between these pathophysiological factors.
Potentially changing risk factors for delirium
- Sensory impairments, such as auditory or visual
- Immobilization (catheters or restraints)
- Medications (eg, sedative-hypnotics, narcotics, anticholinergics, corticosteroids, polypharmacy, alcohol or other drug withdrawal)
- Acute neurological diseases (for example, acute stroke - usually right parietal, intracranial hemorrhage, meningitis, encephalitis)
- Intercurrent illnesses (eg, infections, iatrogenic complications, severe acute medical illness, anemia, dehydration, poor nutrition, fractures or trauma, HIV infection)
- Metabolic disorders
- Surgical interventions
- Environment (eg, intensive care unit admission)
- Pain
- Expressed emotional feelings
- Moderate sleep insufficiency (deprivation)
Permanent risk factors
- Dementia or cognitive impairment
- History of delirium, stroke, neurological disease such as ataxia
- Multiple comorbidities
- Male
- Chronic renal or liver failure
Age > 65 years
Current evidence suggests that drug toxicity, inflammation, and acute stress reactions may contribute significantly to disruption of central nervous system neurotransmission and ultimately to the development of delirium. Systemic inflammation may result from systemic infection, trauma, or surgery. The cholinergic system plays a key role in cognitive function and it is therefore not surprising that there is extensive evidence supporting the role of cholinergic deficits in the genesis of delirium. Anticholinergic drugs can cause delirium and often contribute significantly to the delirium observed in hospitalized patients. Increased acetylcholine levels due to the use of cholinesterase inhibitors such as physostigmine can cause delirium. Serum anticholinergic activity, which reflects the anticholinergic effects of both endogenous and exogenous drugs and their metabolites, has been shown in some studies examining the dynamics of delirium. Other neurotransmitter abnormalities associated with delirium include increased dopaminergic brain activity and a relative imbalance between the dopaminergic and cholinergic systems. The use of antiparkinsonian drugs can also cause delirium, and dopamine antagonists such as haloperidol are effective in treating symptoms of delirium. The neurotransmitters glutamate, γ-aminobutyric acid, 5-hydroxytryptamine (5-HT), and norepinephrine have also been suggested to be associated with delirium.
- Delirium is a common cause and serious complication of hospitalizations and has important consequences for the patient, both functionally and economically.
- Delirium is potentially preventable and treatable, but major barriers, including underestimation of the severity of the syndrome and poor understanding of its underlying pathogenesis, have hampered the development of successful treatments
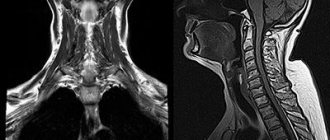
- Neuroimaging has revealed structural changes in delirium, including cortical atrophy, ventricular dilatation, and white matter lesions, which may be considered both predictors of delirium and its consequences.
- Evidence suggests that impaired neurotransmission, inflammation, or acute stress reactions may contribute to the development of delirium
- Delirium is not always short-lived or reversible and may lead to long-term cognitive changes
There is experimental and clinical evidence to suggest that trauma, infection, or surgery may lead to increased production of proinflammatory cytokines, which may precipitate delirium in sensitive patients. Peripherally secreted cytokines can provoke exaggerated responses from microglia, thereby causing significant inflammation in the brain. Proinflammatory cytokines can significantly influence the synthesis or release of acetylcholine, dopamine, norepinephrine and 5-HT, thereby disrupting neuronal communication and they can also have direct neurotoxic effects. In addition, pro-inflammatory cytokine levels have been shown by a number of researchers to be elevated in patients with delirium. delusional. The presence of low-grade inflammation associated with chronic neurodegenerative changes in the brains of patients with dementia may explain why these patients are at increased risk of delirium. The importance of high cortisol levels associated with acute stress has been suggested for the onset and/or maintenance of delirium. Steroids may cause deterioration of cognitive function (steroid psychosis), although not all patients receiving high doses of steroids will develop delirium. In elderly patients, cortisol feedback regulation may be impaired, resulting in higher baseline cortisol levels and thereby predisposing this population to delirium. A number of studies have found elevated cortisol levels in patients who developed postoperative delirium. Other studies have found an abnormal decrease in cortisol in a dexamethasone suppression test, a result that indicates dysregulated cortisol leading to increased cortisol levels in patients with delirium. The role of cortisol in the development of delirium, however, deserves further study. Delirium associated with direct neuronal damage can be caused by various metabolic or ischemic brain lesions. Hypoxia, hypoglycemia and various metabolic disorders can cause energy deprivation, which leads to disruption of the synthesis and release of neurotransmitters, as well as disruption of the propagation of nerve impulses along the nerve networks involved in the processes that ensure the functioning of the cognitive sphere. In elderly patients with delirium of various etiologies, imaging showed cortical atrophy in the prefrontal cortex, temporal cortex in the nondominant hemisphere, and atrophy of deep structures, including the thalamus and basal ganglia. Other features that are observed on imaging include: ventricular dilatation, white matter changes, and basal ganglia lesions. These changes likely reflect a state of increased vulnerability of the brain to any negative impact and an increased susceptibility to the development of delirium. A number of studies, however, have not identified any significant abnormalities in CT scans of patients with delirium. To date, relatively few studies have used functional imaging to examine brain changes in delirium. One prospective study of hospitalized patients with delirium of various etiologies used single photon emission tomography (SPECT) and found frontal and parietal hypoperfusion in half of the patients. Other studies that have used SPECT imaging, primarily in patients with hepatic encephalopathy (a form of delirium caused by liver failure), have identified various types of hypoperfusion, including involvement of the thalamus, basal ganglia, and occipital lobes. In one study with Xenon-enhanced CT, global perfusion was decreased during delirium. Rapid progress in the development of neuroimaging technologies offers exciting prospects for the use of new methods to elucidate the mechanisms of delirium. These techniques include volumetric MRI, which may be useful in assessing the rate of brain atrophy following delirium or determining threshold levels of atrophy that predispose patients to delirium. Diffusion tensor imaging and tractography can help assess damage to the fibers of neural tracts that connect different areas of the brain. Arterial spin perfusion measures blood flow and can be used to assess both cerebral perfusion and response to medications. MRI can also be used to assess the integrity of the blood-brain barrier and its role in the development of delirium. It appears that the symptoms of delirium are quite variable, but it can be classified into three subtypes - hypoactive, hyperactive and mixed - based on the characteristics of psychomotor behavior. Patients with hyperactive delirium show signs of restlessness, agitation, and increased anxiety and often experience hallucinations and delusions. In contrast, patients with hypoactive delirium, accompanied by lethargy and sedation, are slow to respond to questions and show limited spontaneous activity. The hypoactive form is most common in older patients, and these patients are often overlooked or misdiagnosed as having depression or a particular form of dementia. Patients with mixed delirium exhibit both hyperactive and hypoactive features. It has been suggested that each subtype of delirium may result from a distinct pathophysiological mechanism and that each variant of delirium may have a different prognosis.
General diagnostic criteria for delirium
- (A) Impaired consciousness (i.e., decreased clarity of awareness of the environment) with decreased ability to focus, maintain, or shift focus of attention
- (B) Cognitive changes (eg, memory deficits, confusion, speech impairment) or development of perceptual impairments that are not associated with dementia
- (C) The disorder develops over a short period of time (usually hours to days) and typically fluctuates in severity throughout the day
Criteria for delirium that has developed due to deterioration in general health
- (D) Evidence from history, physical examination, or laboratory testing indicates that the disorder is caused by direct physiological effects of general health conditions
For delirium due to substance intoxication
- (D) Evidence from history, physical examination, or laboratory testing indicates that either (1) symptoms in criteria A and B are due to substance intoxication, or (2) drug use is etiologically related to delirium
For delirium, "multiple" etiologies
- (D) History, physical examination, or laboratory tests indicate that delirium has more than one etiology
Postoperative delirium may develop on the first or second postoperative day, but the patient is often hypoactive and therefore may go undetected. Delirium is difficult to recognize in the intensive care unit because standard cognitive tests of attention are often not used because patients are intubated and unable to answer questions verbally.
Symptoms of the syndrome
To establish a diagnosis, the patient is admitted to a hospital for the purpose of a formal assessment of mental status. When making a diagnosis, three repetition tests are used. Testing and behavioral monitoring can help identify symptoms of delirium. These include:
- Manifestations of clouding of consciousness. Expressed in a violation of perception and cognition of the surrounding world. They suggest detachment from what is happening, incoherent judgment, meaningless speech, slow reactions, disorientation, complete or partial loss of memory.
- Hallucinations. The intensity of visual images that occur without external stimuli depends on the causes of delirium. The most vivid delusional pictures that distort real life are characteristic of withdrawal syndrome, delirium tremens, and hysteria. May manifest in different forms, depending on the patient; some see those same little green men, others see insects or strangers. Illusions on religious themes are not uncommon.
- Unusual motor activity. Manifested by excitement and reproduction of various actions. Sometimes the patient may think that he is at his workplace and perform characteristic movements.
- Inarticulate muttering (delirium delirium). Occurs in patients with infectious diseases, brain damage, and recovery after surgery. Accompanied by hand movements, speech contact is impossible. Sometimes it manifests itself in an abortive form - lasts less than a day and is not accompanied by disorientation.
- Tremor and tic. The anxiety state is aggravated, random movements gradually become constant and obsessive.
- Change in facial expressions. The mental state can be determined by increased emotionality, pantomime and a characteristic grotesque facial expression.
- Strange behavior. In patients, delirium can cause panic, uncontrollable anger, prolonged laughter, tears, sexual arousal, and screaming.
- Sleep disturbance. There are difficulties falling asleep, nightmares, and some fear of sleep.
The clinical picture depends on the etiology of the syndrome. Diagnosis of the condition can only be carried out by specialists. Often the manifestations are similar to those of other diseases, for example, dementia occurs in a similar way.
Stages of development of delirium
Delirium is a mental disorder that develops gradually. Each stage of the disease has its own special symptoms:
- The first stage is not always noticed by others and the patient himself. Only precursors of the disease, pre-delirium symptoms, are observed. The person becomes more talkative, experiences vivid memories of the past, and thinks in unexpected associations. The level of critical thinking decreases, orientation is disrupted. During this period, sleep disturbances often occur, and the sleep and wakefulness patterns are disrupted. If a person is sleeping, he wakes up very easily. Characterized by vivid, very “real”, believable dreams.
- At the second stage, attention deficits, difficulties with concentration, and sober perception of reality increase. It becomes difficult for a person to navigate in time. The first precursors of hallucinations appear - visual illusions. Moreover, when you try to take a closer look at the apparent phenomenon, it does not dissipate, but becomes clearer. Fear grows from imaginary dangers.
- The third stage is characterized by the beginning of real hallucinations. The patient's attention is switched to these visions. Most often these are visual images, but there can be auditory and tactile sensations. Human behavior begins to obey this augmented (or parallel) reality. He can lie in bed and tear the bed linen, move in panic, shake off apparent insects, and barricade the entrance to the home. At such moments, the patient can be dangerous both for others and for himself due to inappropriate actions. These include the use of physical force, aggression, going out onto a busy roadway, jumping out of a window on any floor, etc. It is extremely difficult to conduct a dialogue with a person in such a state. He ceases to navigate in space and has difficulty determining his location. Difficulties falling asleep and a shift in sleep patterns from night to morning are also typical.
Treatment options for delirium
Treatment of delirium involves an integrated approach aimed at getting rid of the cause and stopping behavioral disorders. There are medical non-drug and pharmacological methods of therapy. Typical use:
- Non-drug methods. The group includes various psychotherapeutic techniques, cognitive stimulation, and verbal techniques. Communication with family and loved ones plays an important role. It is recommended to maintain a balance between stimulation and calming: it is advisable to reduce any stimulating actions to a minimum.
- Drug therapy is common. The classic scheme involves the use of antipsychotics, antidepressants, and sedatives. Combinations, dosages and prescriptions are related to etiology.
Some forms of delirium (pharmacological, alcoholic, drug) should be treated without drugs or with a limited number of drugs. Excess chemicals can worsen psychosis.
Progression and consequences of untimely treatment
Delirium and the behavioral abnormalities it causes appear suddenly. The patient's age, health status, causes and nature of manifestations should be taken into account. The progression of symptoms such as restlessness, hallucinations, and anxiety depends on the nature of the syndrome. With alcoholic, psychopharmacological or drug delirium, the condition worsens rapidly. The patient exhibits cardiovascular system disorders, blood pressure fluctuations, and large-scale tremor. No less dangerous is rapidly developing delirium of an infectious nature. It is accompanied by fever, chills, and intoxication. Damage to the body by infection leads to the development of an inflammatory process, leading to improper functioning of organs and systems.
Older people are more likely to experience slow progression of delirium. This leads to the development of complications, increased cost of treatment, and profound impairment of cognitive function. There is a risk of incomplete physical recovery and some memories never return. In the next two years, death is more likely. However, if you consult a doctor in a timely manner, the prognosis is mostly favorable. The lack of competent therapy can lead to rapid deterioration of conditions, complications or even death.
Diagnosis of the disease
To make an accurate diagnosis and select a hospital profile, it is necessary to collect an anamnesis as completely as possible (with the involvement of relatives and neighbors) and conduct a proper examination.
When collecting data about a patient's life, it is important to find out the following points:
- the presence of previous disorders of consciousness;
- heredity for mental illness;
- tendency to use drugs, psychoactive substances and alcohol;
- the presence of chronic somatic diseases, acute infections;
- previous injuries and surgeries;
- facts of hospitalization in psychiatric hospitals.
The purpose of an objective examination is to determine the severity and nature of neurological and vegetative-somatic disorders. You need to try to establish contact with the patient by asking simple questions. The assessment of answers well characterizes specific thinking disorders. Hospitalization in a hospital is carried out according to regulated protocols for the treatment of this disease.
Stationary
The first aid for delirium is 24-hour hospitalization. In Moscow and other Russian cities, doctors are successfully fighting the condition and its consequences. Recovery is mainly achieved through a combination of medication and psychotherapy. The following stages are expected:
- Detecting causes and prescribing appropriate therapy;
- Minimizing the amount of medications taken;
- Detoxification is carried out if necessary;
- Creating a favorable and calm environment;
- Relieving disorientation in space, time and society;
- Drawing up a recovery plan for the body.
Before starting therapy, it is necessary to diagnose the brain using X-rays. The method of magnetic resonance or computed tomography allows identifying a condition of traumatic, organic etiology, as well as vascular, the treatment of which is important to begin immediately. Additionally, it is necessary to conduct a general blood and urine test. Laboratory tests make it possible to assess the patient’s condition, detect intoxication, inflammation, and symptoms of renal failure. The department of the hospital that treats delirium becomes specialized for the main diagnosis: narcology, gastroenterology, urology, nephrology.
Securing the patient should be strictly avoided. This leads to aggravation of the stage, the patient suffers and becomes nervous. Limb binding is used only in cases of life-threatening situations (suicide attempt) or during periods of aggression.
Methods for correcting behavioral deviations due to the syndrome
- Timely changes in diet (refusal of foods that cause drowsiness or alertness), discontinuation of psychostimulant drugs. Creating a favorable and calm atmosphere. Refusal of medications that can be avoided at this stage. In case of persistent sleep disturbance, take sedative medications.
- Illusions, delusions, auditory and visual hallucinations. Symptoms require the use of antipsychotics (aloperidol, chlorpromazine, clozapine)
- Increased emotionality in delirium. Psychotherapy usually helps. If the patient has become depressed, then it is permissible to use mood stabilizers or antidepressants.
- Excessive excitement. Recovery is facilitated by the presence of loved ones. Fixation of the limbs leads to aggravation of the condition. Possible use of sedatives or antipsychotics
- Confusion. In most cases, setting reference signals helps. For example, a clock, a calendar, familiar objects. The patient is forced to count, characterize shapes, name the days of the week
- Anxiety. Benzodiazepines are used. If the course of the disease is complicated by psychotic disorders, then antipsychotics are recommended.
The acute stage of delirium lasts about 2 weeks. Improvement is evidenced by sound, healthy sleep. The patient often treats the incident as a nightmare or does not remember anything.
Dangers of self-medication for delirium
Not all patients with delirium tremens or other types of delirium rush to seek help. On the Internet you can find a lot of advice on how to get rid of the signs of the condition: detachment, loss of orientation, chaotic movements, hallucinations. Self-medication using an algorithm from a random site can negatively affect health or life in the following ways:
- It is difficult or impossible to establish the causes without a specialist. The course of delirium can differ significantly from the description: sometimes a number of signs are completely absent. Even with severe symptoms, diagnostic procedures are required.
- Sometimes psychosis develops rapidly. The condition is characterized by a high rate of progression. Delay may result in lost functions not being restored or causing death. Psychosis accompanied by a suicide attempt is not uncommon.
- Only by receiving professional help can you cope with the disorder. As a result of improper therapy, manifestations become intense and irreversible. If treated correctly, restoration of activity takes at least 6 months after the condition has resolved.
- The symptoms of delirium are similar to other diseases. Sometimes behind the appearance of a sign there are other dangerous pathologies.
- Delirium can accompany life-threatening conditions. Detection of the process is often associated with myocardial infarction, stroke, hypoglycemia, and poisoning.
- Psychosis is fraught for others. Alcoholic delirium is considered the most dangerous. When it is repeated, patients show hatred towards others and are even capable of murder.
Considering all the dangers of self-medication, the main thing is to immediately seek medical help.
Main signs of delirium
The main manifestation of delirium is hallucinations.
Delirium has all the characteristic signs of clouding of consciousness: detachment with significant difficulty in perceiving the outside world and subsequent amnesia, disturbance of the thought process and orientation. Allopsychic disorientation is not typical. In addition, delirium is characterized by hallucinatory-illusory disorders. Their content determines the patient’s behavior and often becomes the cause of the development of sensory delirium.
The appearance of hallucinations is preceded by illusory and pareidolic disturbances and frightening dreams. A little later they are supplemented by hypnagogic (arising in waking states) hallucinations. And at the stage of advanced delirium, hallucinations become abundant, scene-like and almost constant. Their influx can be provoked by pressing on the eyeballs, which is called Lipman's symptom.
Hallucinations in delirium are true. They are subjectively indistinguishable from objects in the surrounding world and therefore are perceived by a person as real images, even if their content is clearly fantastic. Visual hallucinations predominate - abundant, bright, detailed, most often unpleasant and frightening. But auditory, tactile and olfactory perception deceptions are also possible.
Hallucinatory experiences are accompanied by a tense affect of anxiety and fear. Periods of psychomotor agitation or physical inactivity are possible. In an attempt to defend themselves or escape, the patient often poses a danger to others and himself. But in some forms of delirium, motor restlessness is limited to the bed, and no obvious affect of anxiety is noted. Most often, this indicates a deep disintegration of mental activity and is a sign of severe suffering in the brain.
The productivity of contact with the patient, the severity of disorientation and the presence of amnesia after relief of delirium depend on the degree of confusion and the volume of perception of the surrounding world. Memories of real events that occurred during this period are fragmentary or completely absent, and partial or complete amnesia of one’s experiences is also noted.
Outpatient
The second part of the therapy can be done at home. Recovery takes place under the supervision of a specialist. Therapy includes:
- A calm atmosphere and establishing contact with others. At home, the patient should be given attention, not disturb him unnecessarily and not cause negative emotions. It is important not to raise your intonation or provoke conflict. Initially, the patient may experience frequent mood swings, aggression, and tearfulness. Occasionally, a distortion of reality is recorded.
- Elimination of factors that provoke the condition. The drug that causes psychosis should be immediately removed from the patient’s field of vision. If the cause was delirium tremens, you should give up any alcoholic beverages and undergo coding. If a factor cannot be excluded (for example, a systemic disease), then it is worth minimizing its consequences by continuing therapy as indicated.
- Psychotherapy. To restore the ability to think and soberly assess the situation, as well as to track dynamics, it is recommended to continue psychotherapy. Group and individual lessons help.
- Healthy lifestyle. Lifestyle also plays a certain role. It is especially important to give up smoking, drugs, alcohol and monitor your sleep patterns. To some extent, normalization of nutrition has a beneficial effect.
Many experts talk about the beneficial effects of reflexology, massage, and swimming. With timely treatment, proper treatment and compliance with recommendations, complete remission is usually observed.
Forecast
Delirium is not a life-threatening condition, except in cases of particularly severe confusion with characteristic disorientation. However, if the disease is not treated, in later stages it threatens to develop into more dangerous conditions. In particular, there are known cases of transformation into oneiroid, a condition accompanied by mystical hallucinations. Most patients with delirium are completely cured. Recovery takes longer in older patients with multiple chronic diseases. For such people, this may take weeks or months. Some of these patients are not able to restore brain function to its original state.
During the first two years after treatment for delirium, the risk of functional and cognitive impairment remains. It is necessary to pay enough attention to health and undergo periodic examinations in order to prevent possible complications in time. In advanced cases, there is a danger of consequences in the form of organic diseases.
Prevention
It is not always possible to prevent the development of delirium due to various causes. To prevent the development of the condition, it is necessary to eliminate negative factors in a timely manner.
What causes delirium symptoms and what should be avoided if possible for prevention:
Predisposing
- Elderly age. Geriatric delirium, which is difficult to treat, is most common in people over 60-65 years of age
- Dementia of varying degrees
- Male age
- The presence of some (several) chronic pathologies. The prerequisite may be diseases of the endocrine system, urinary system, heart and blood vessels
Provoking
- Acute damage to internal blood vessels and heart, lungs, kidneys
- Violation of water-electrolyte metabolism
- Bed rest, insufficient movement for a long time
- Constipation, urinary retention
- Infection
- Installation of catheters, stomas, stimulators
- Dangerous drugs and substances that cause delirium
You should take with caution: antihistamines, antibiotics, antipsychotics, drugs with lithium, opiates, chloral hydrate, sedatives, drugs against Parkinson's disease, barbiturates, anticonvulsants, benzodiazepines
For patients with alcohol and drug addiction, prevention will include giving up bad habits. Solving the problem on your own is not easy; it is better to seek the help of professional narcologists. The greatest positive effect is provided by treatment in specialized clinics. They allow not only to overcome addiction, but also to socialize in society.
Etiology and pathogenesis
The etiology of the delirium is unknown, but it is likely to be complex, due to the influx of provoking factors on the contagious diseases that may be associated with the delirium. So the pathogenesis itself has not yet been studied. No structural changes in the brain were detected; neuroimaging studies provide superb results. The electroencephalogram (EEG) shows increased cortical background activity, the appearance of delta and theta activity, which correlates with the stage of cognitive impairment, but is not specific. The effectiveness of oxygen therapy is evident because one of the mechanisms can disrupt oxide metabolism in the brain. Neurophysiological studies revealed dysfunction of the prefrontal and thymo-scroneal cortices, subcortical structures, thalamus, basal ganglia, especially in the non-dominant ligament. The leading hypothesis for the pathogenesis is disruption of neurotransmission, inflammation and chronic stress.
There is no evidence that delirium can be mediated through disruption of cholinergic systems. Anticholinergic intoxication, which leads to behavioral and EEG manifestations of delirium, can be reversed by the infusion of cholesterase inhibitors. Hypoxia and hypoglycemia lead to a decrease in the synthesis of acetylcholine. The anticholinergic activity of the serum is associated with delirium in patients with internal and surgical diseases and in those who respond to electrovascular therapy. It is also associated with cognitive impairment in the elderly (as they experience in nursing homes for the elderly).
Dopaminergic hyperactivity can also be counteracted by delirium through infusion of acetylcholine. Levodopa can relieve delirium, and dopamine receptor antagonists (antipsychotics) can effectively treat its symptoms. There is less evidence for the participation in the pathogenesis of such compounds as norepinephrine, gamma-aminobutyric acid, glutamate, serotonin, etc.
Delirium may be caused by the influx of cytokines into the central nervous system, such as interleukin-1, 2, 6, alpha necrosis factor, interferon. The stench will penetrate the blood-brain barrier and disrupt neurotransmission. Clinical and EEG manifestations of delirium have been described in patients treated with interferon-α. Delirium is cured in half of patients with long-term cancer treated with interleukin-2 and lymphokine-activated T-killer cells.
Hypercortisolism in chronic stress causes a rapid influx on the 5-HT1A receptors of the hippocampus, which causes delirium. Overall, the clinical heterogeneity and multifactorial nature of delirium suggest multiple pathogenetic mechanisms.
conclusions
Delirium is an acute condition with sudden development, having a different etiology. It causes persistent changes in consciousness, major disruptions in vital activity and is life threatening. Patients are not aware of their actions; such mental disorders can traumatize others. The effectiveness of delirium treatment is based on the emergency adoption of somatic measures, minimizing pharmacological therapy, and creating a trusting atmosphere. Only specialists can provide first aid, carry out separate measures, and guarantee recovery. It is strictly forbidden to fight psychosis on your own or not take any measures.