Neuroinfections can lead to damage to the structures of the central nervous system - what they are, how exactly they manifest themselves and what therapy to choose to combat them, we will consider in detail. By neuroinfections, experts mean a fairly wide group of neurological diseases that can develop in people of any gender and age.
Children and older people are more susceptible to them, since the disease is more severe in them, and the consequences appear more often. If you seek medical help early, there is a chance of complete recovery. Therefore, it is not recommended to delay consultation with a specialist if you suspect such a pathology.
Classification
Since neuroinfection of the brain is difficult to describe from any one aspect, neuropathologists traditionally adhere to the following classification of the disease:
According to the timing of penetration of the pathogen into the brain and the occurrence of the main symptoms:
- rapid neuroinfection - clinical manifestations of replacement 3-8 hours from the moment of infection;
- acute course of the disease - signs of inflammation are observed towards the end of the second day;
- smooth neuroinfection - such a disease is characterized by the appearance of symptoms within 2-7 days from the moment of infection;
- chronic neuroinfections, which are characterized by a long process, usually occur in people whose bodies are already weakened by serious diseases (HIV, tuberculosis).
Upon the appearance of a focus of inflammation:
- primary neuroinfection - when a pathogen enters the central nervous system directly from the outside;
- the secondary option is a complication of a focus of infection already existing in the human body.
By type of pathogen: bacterial neuroinfection, viral variant, fungal form, parasitic attack.
When explaining to a patient what a neuroinfection is, doctors are guided by the above criteria for classifying the disease, only sometimes adding other signs to the diagnosis. For example, the route of transmission, existing complications.
Types of neuroinfections
Classification is necessary to prescribe standard and effective treatment to patients. There are several approaches to dividing the disease. The main classification is based on the location of the lesion:
- Encephalitis is damage to the nervous tissue of the central nervous system structures. Focal neurological symptoms and signs of intoxication predominate. Tick-borne encephalitis is often detected, as well as those associated with the herpes virus, chickenpox and rubella.
- Meningitis - manifests itself as inflammatory changes in the meninges. Patients experience cerebral and meningeal symptoms against the background of severe intoxication phenomena. If the disease is caused by viruses or the causative agent of tuberculosis, meningitis is serous in nature. With bacterial or fungal infection, a purulent type of meningitis is noted.
There are also specific forms of neuroinfections: polio, abscesses, neurosyphilis, herpes zoster, botulism and neuroAIDS. They are characterized by the development of pathological changes in certain structures of the central nervous system against the background of infection with a specific microorganism.
Depending on the course of the disease, a diagnosis of acute, subacute or chronic neuroinfection is made. Types of the disease differ in the nature of the onset of symptoms, the duration of their persistence in the patient and the consequences for his body.
How is neuroinfection transmitted?
Viral neuroinfection is characterized by airborne transmission - from one person to another during close contact , prolonged stay in the same room, coughing, sneezing. When settling on the mucous membrane, especially if it is damaged, droplets of liquid from the air, with many viral particles, become a source of infection. Then pathogenic microorganisms enter the bloodstream and reach the membranes of the brain.
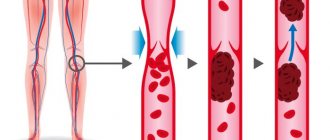
The hematogenous route will be characteristic of the bacterial form of neuroinfection, when pathogens move from an existing primary focus along the lymphatic pathways and blood vessels to the structures of the central nervous system. Pathologies predisposing to this: abscesses, sinusitis, otitis, frontal sinusitis.
However, cases of household contact infection are extremely rare . Therefore, there is no need to fear that a neuroinfection of the brain will appear due to the use of shared cloths or utensils.
The vertical path - from mother to her child - is also practically impossible. When diagnosing neuroinfections in children, airborne infection is usually considered to be the culprit.
NEUROINFECTION
What is a neuroinfection?
The term “neuroinfection” does not refer to any single disease. This is a whole section of fairly common neurological pathologies (more than 42% of total statistics). It included damage to the nervous system caused by an infectious agent. In other words, neuroinfection is the general name for infectious diseases, the causative agent of which is localized in the nervous tissue and causes inflammation:
- brain or its membranes;
- spinal cord;
- peripheral nerves.
The etiological spectrum of neuroinfections is quite wide - viruses, bacteria, fungi, and some types of protozoa. Mixed infections, in which a symbiosis of pathogenic flora is detected, become of great importance. For example, herpetic neuroinfection - meningoencephalitis, encephalomyelitis.
Taking into account the duration of the disease, there may be neuroinfections that are chronic (sluggish) in nature, or acute and subacute forms of damage to the nervous system.
Acute neuroinfection
In neurological practice, the most serious are considered to be neuroinfectious lesions that develop acutely and have a severe course with a high percentage of deaths. The most common emergency conditions include:
- meningitis - inflammatory processes occur in the membrane of the brain and/or spinal cord;
- encephalitis - damage to brain tissue;
- myelitis - inflammation localized in the spinal cord;
- arachnoiditis is a pathology of the arachnoid membrane of the brain.
Chronic neuroinfection
Chronic neuroinfections are characterized by a long course of the pathological process, in which remissions alternate with periods of exacerbations. Common representatives of this category of diseases:
- brucellosis;
- neurosyphilis;
- neuroAIDS;
- damage to the central nervous system due to tuberculosis.
Classification of neuroinfection
All neuroinfections are divided into two significant groups:
- primary (true) - independent diseases, the causative agent of which is neurotropic, it initially affects the cells of the nervous tissue;
- secondary - damage to the nervous system occurs due to dissemination from a primary focus already existing in the body (for example, toxoplasmosis, tuberculosis, influenza, syphilis).
From the point of view of the pathomorphological picture, several types of neuroinfections are distinguished:
- primary and secondary purulent meningitis and meningoencephalitis;
- serous meningitis of various origins;
- viral neuroinfection - encephalomyelitis and encephalitis;
- demyelinating (slow) neuroinfections.
Neuroinfections in children are included in a special category. Due to the fact that their immunity has not yet been fully formed, children are most susceptible to infectious diseases of the nervous system. The most typical are chickenpox meningitis and herpesvirus neuroinfection.
Symptoms of neuroinfection
Signs of neuroinfection have varying degrees of manifestation, depending on the severity of the condition. Despite the variety of types, all acute neuroinfections are clinically associated with cerebral edema against the background of general infectious symptoms. They include five main syndromes:
- intracranial hypertension - increased intracranial pressure is accompanied by increasing headaches, nausea, vomiting, dizziness;
- disturbances of consciousness - varying degrees of psychomotor agitation, retardation, delusional states, depression, inadequate reactions, coma;
- convulsive;
- pronounced meningeal - inability to tilt the head forward (stiff neck muscles), Kernig's symptom (if you first bend the patient's leg at a right angle in the area of the hip and knee joints, then he will not be able to straighten it voluntarily);
- focal neurological lesions - manifestations depend on the areas of the brain that have undergone pathological changes (for example, nystagmus, foot clonus).
When a neuroinfection develops, symptoms of general intoxication of the body are manifested by severe hyperthermia (an increase in body temperature almost always to critical levels), general weakness, and a significant decrease in performance.
Neuroinfection treatment
Treatment of patients diagnosed with a neuroinfection of the brain must be carried out in a hospital. Methods of drug therapy carried out in the treatment of neuroinfections always depend on the pathogen that provoked the disease and the localization of the pathology. Treatment measures are aimed at comprehensively solving the main triad of problems:
- elimination of the infectious agent and ways of its spread;
- boosting immunity;
- restoration of impaired functions of the nervous system.
Symptomatic therapy is carried out - if necessary, antipyretic, sedative, and anticonvulsants are prescribed. In case of severe neuroinfection, treatment includes prescribing an appropriate course of rehabilitation. For example, to restore speech, the ability to dress independently, move around, write, etc.
Consequences of a neuroinfection
It is extremely rare that infectious diseases of the nervous system resolve without complications for the patient’s health. The consequences of a neuroinfection depend on the type of disease and the time of treatment. Patients may be left with headaches or back pain that worsen with changes in weather. After recovery, memory, vision or hearing may deteriorate. Against the background of neuroinfections, concomitant diseases may be activated. For example, with myelitis, paralysis almost always occurs. The most serious are the consequences of a neuroinfection of the brain suffered in the prenatal period. They entail developmental anomalies and various defects of internal organs and systems.
Causes of neuroinfection
The human brain is firmly protected from external aggressive factors by the bones of the skull, and from the inside by tissue membranes. However, despite such protection, pathogenic microorganisms are still sometimes able to penetrate nerve cells and provoke inflammation in them.
The causes of neuroinfection of the brain can be:
- suffered traumatic brain injuries, which is especially dangerous - with prolonged compression of brain tissue;
- hypothermia – general and directly to the head;
- performing surgical interventions in the area of the skull using poorly processed instruments or without surgical gloves is absolutely unacceptable;
- low quality dental services - unsterile instruments.
Neuroinfection can appear as a consequence of a disease already existing in the body, which weakens the protective barriers of brain tissue. Doctors indicate provoking factors:
- state of immunodeficiency – HIV infection, tuberculosis;
- chronic focus of purulent infection - tonsillitis, otitis, caries;
- traumatic brain injuries without follow-up examination.
Knowledge of what was the cause and background against which the focus of inflammation formed in the brain tissue helps specialists select effective treatment tactics.
Kinds
During their development in the human body, infectious agents can cause diseases such as:
- meningitis (inflammation of the cerebral cortex);
- encephalitis (nervous tissue of the brain is affected by infection from an encephalitis tick bite);
- myelitis (inflammation localized in the spinal cord);
- amyotrophic sclerosis (lateral) – destruction occurs at the cellular level of the parts of the brain responsible for the movement of muscles and ligaments;
- herpes zoster ;
- polyneuropathy (peripheral parts of the nervous system are affected);
- arachnoiditis (inflammation of the arachnoid membrane of the brain, resulting from previous head injuries or advanced ENT diseases).
In addition to the listed diseases, during the development of neuroinfection there are pathologies of a combined nature, for example, encephalomyelitis, in which inflammatory processes affect both the brain and spinal cord. This form of development of an infectious disease is difficult to diagnose, even taking into account the capabilities of modern medicine.
Symptoms and signs of meningitis
When the lining of the brain is affected by the inflammatory process, experts talk about the occurrence of meningitis. If the causative agent is a viral microorganism, it is a viral neuroinfection. Whereas bacterial agents will provoke bacterial meningitis.
The following symptoms help make a diagnosis:
- tension in the muscles of the shoulder girdle and the back of the head - it is difficult for the patient to tilt his head to the sternum;
- headache – intense, diffuse, cannot be treated with standard analgesic drugs;
- vomiting – frequent, profuse, does not bring relief to the person;
- temperature is high from the very first hours of infection.
Nonspecific signs - pallor of the integumentary tissues, sweating, loss of appetite, increasing weakness, fluctuations in blood pressure.
Diagnosis is based on a thorough history taking. Information will be required about contact with an already sick person, stay in the source of infection, as well as laboratory and instrumental studies - blood tests, cerebrospinal fluid tests, brain tomography. Such a detailed examination makes it possible to distinguish between neuroinfection in children and adults, and subsequently to select the optimal treatment regimen.
Symptoms
The symptoms of neuroinfections depend on the type of the main pathogen, the form of its penetration into the tissues of the nervous system and the severity of the disease. A number of the main signs of the manifestation of neuroinfections include general cerebral syndromes of an infectious nature, namely:
- disturbance thermoregulation , accompanied by low-grade fever;
- increased erythrocyte sedimentation rate;
- increase in heart rate;
- leukocytosis;
- headaches that occur predominantly in a lying position, especially in the morning;
- dizziness;
- low systolic blood pressure;
- general weakness of the body;
- acute sensitivity of the epidermis;
- dislike of irritants of the organs of hearing and vision, for example, loud sounds or bright lights.
Neuroinfections, the development of which is localized on the membranes of the brain, cause the manifestation of meningeal syndrome, namely stiffness of the neck muscles, as well as Kerning and Brudzinski symptoms.
If the central part of the nervous system is involved in the development of pathology, then this begins to provoke the formation of a focus of neurological symptoms, such as paresis, extrapyramidal syndrome and disorders at the psycho-emotional level.
Injury to the nerve fibers of the peripheral nervous system is manifested by an increase in flaccid paresis, characterized as temporary immobilization.
Listeriosis
Listeriosis is a zoonotic disease of infectious origin that affects nerve cells and mononuclear cells, and also develops in an angioseptic form.
Moreover, the lesions mostly affect the legs, which subsequently affects changes in a person’s gait. With increased palpation of the legs, especially the calf muscles, pain is noted in the area where the largest nerve trunks are located.
When the pathological process of development of an infectious disease complicates, paralysis may occur.
Symptoms and signs of encephalitis
If an inflammatory focus appears directly in the brain tissue, we are talking about encephalitis. Such an infection is extremely dangerous for people’s lives - in the absence of quick and comprehensive treatment, death is possible.
For encephalitis, as a neuroinfection, symptoms will be:
- pain – over the entire surface of the head, intense, exhausting, unresponsive to analgesics;
- disruption of brain activity – loss of consciousness, coma;
- nausea, vomiting – these signs are not specific, but with encephalitis, vomiting does not make the patient feel better;
- temperature – the disease begins with a sharp rise, the numbers remain high throughout the course of the disease;
- the appearance of paralysis/paresis - on the side where the focus of inflammation has formed;
- sensory organ disorders – deterioration of vision, hearing, smell.
Among the general manifestations, the patient is worried about severe weakness, lack of appetite, sleep disturbance, increased heart rate, and the inability to fully self-care.
Neuroinfections in children are more severe - the symptoms of brain damage are pronounced, and the disease more often leads to complications. The child almost immediately loses consciousness, is unable to answer questions about his well-being, and experiences convulsions and epileptic attacks.
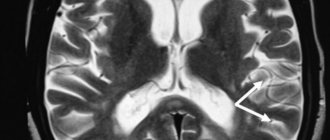
Diagnosis of encephalitis is based not only on the collection of complaints and examination of the patient, but also on information from modern methods of brain research - encephalography, computed tomography or magnetic resonance imaging.
Treatment must take place in a hospital setting ; drugs are selected by the doctor taking into account the identified causative agent of encephalitis, the age of the patient, and the severity of negative symptoms.
Tick-borne encephalitis as a type of neuroinfection: symptoms, causes
Tick-borne encephalitis is a neuroinfection of natural origin. Encephalitis is transmitted to humans by the bite of a tick infected with the virus. The tick attaches itself to the skin of its victim and begins to slowly suck the blood out of it, while the “parasite” increases significantly in size. The distribution area of tick-borne encephalitis is the Far East, Siberia, China. Rare cases of the disease can also be observed in Central Europe.
There is a fairly high probability of getting a neuroinfection in spring or summer, and occasionally in early autumn. At this time, the number of ticks increases significantly, and you can become infected with them in the forest, park, or just at a picnic by the river.
The disease can be acquired directly through the bite of a tick, or through dairy products that have not been heat-treated and come from infected animals (the tick can also infect domestic cows and goats). The disease is quite serious; failure to seek help in a timely manner can lead to complex neurological disorders, and in some cases, to the death of the patient. People infected with tick-borne encephalitis do not pose a danger to others.
The incubation stage of the disease usually lasts 7-14 days, but sometimes you can observe a very rapid development of the disease - the first symptoms may appear a day after infection. It happens that the encephalitis virus can sit in the body for more than a month before it manifests itself - this form of the disease is considered protracted.
If the infection enters the body through food, the disease may appear on days 4-7.
It is worth noting that not every person bitten by a tick gets sick - the stronger the immune system, the higher the resistance to infections.
There are three forms of tick-borne encephalitis, depending on the most severe symptoms of the disease:
- Febrile form - this type of encephalitis is accompanied by fever and chills, and occurs in more than half of patients;
- Meningeal form - neuroinfection affects the membranes of the spinal cord and brain in 30% of victims;
- The focal form of encephalitis is observed in 20% of patients, and the brain matter is directly affected.
With neuroinfection of the brain, the symptoms in adults and children are the same. The disease manifests itself spontaneously, with an increase in temperature and a sharp deterioration in general condition. Symptoms can include migraines, weakness, fatigue, and sometimes vomiting (this symptom is often observed in children with an increase in body temperature).
In the febrile form of the disease, the patient’s temperature rises to high levels and can last for several days, and after a short decline it rises again - this picture is observed for about 10 days.
When the patient’s body heat index returns to normal, general well-being is gradually restored, but the patient continues to complain of drowsiness and poor appetite.
The meningeal form is characterized by the appearance of symptoms of meningitis on the 4th day after infection, with a terrible headache, soreness of the skin when touched, nausea and vomiting. Over time, the following neurological features are added - Kernig syndrome (when the patient is unable to straighten a leg bent at the knee while in a supine position) and Brudzinski syndrome (involuntary sharp flexion of the lower extremities when the chin is tilted to the chest and at the same time pressing the pubis with a hand).
All symptoms are combined into the concept of “meningeal syndrome,” which indicates that the virus has nevertheless reached the membranes of the spinal cord and brain. Some symptoms may persist 14 days after infection; complete recovery occurs no earlier than a month later. Muscle weakness, reaction to loud noises and bright lights can occur even after recovery.
The most dangerous and complex form of tick-borne encephalitis is considered focal, the outcome of which is most often unfavorable. The pathogen penetrates the main substance of the brain and spinal cord, affecting the human nervous system. At the same time, the body temperature rises sharply to 40 degrees, the patient’s condition is sleepy, lethargic, and the reaction rate is slow. At high temperatures, chills begin and convulsions may occur.
When the substance of the brain is affected, the patient may experience hallucinations, become delirious and cease to normally perceive the reality around him. The further the infection spreads, the more symptoms appear, and the worse the victim feels.
If the infection affects the brain stem, the functioning of vital organs such as the respiratory system and heart function may be disrupted. When the tissue of the small brain, which is responsible for coordinating movements, is infected, vestibular disorders, tremors of the limbs, and loss of balance are observed.
In addition to tick-borne encephalitis, the following secondary encephalitis can be distinguished, which manifest themselves as a consequence of a specific disease: influenza, measles encephalitis, as well as post-vaccination neuroinfections. The latter most often occur as a result of vaccinations - ADS, DTP and measles vaccine.
Treatment consists of relieving the most acute symptoms.
Manifestations of arachnoiditis
The appearance of an inflammatory process in the arachnoid membrane of the brain indicates a neuroinfection such as arachnoiditis. Its development may be preceded by: traumatic brain injuries, timely poorly treated ENT diseases, rheumatism.
Increased inflammation in the arachnoid membrane of the brain provokes an intense, persistent headache in a person . It deprives the patient of the opportunity to care for himself and perform work duties. Other symptoms of arachnoiditis:
- vision - significantly deteriorates from the flickering of flies before the eyes to a sharp decrease;
- weakness – appears from the first day of infection and constantly intensifies;
- nausea - almost always ends in vomiting;
- temperature – reaches high numbers in the first days of the disease, can be kept within 37.2–37.5 degrees in case of chronic neuroinfection.
In severe cases of the disease, higher nervous activity—memory, intellect, and thinking—suffers. Consciousness is either deteriorated or completely absent.
Treatment tactics are aimed at suppressing the inflammatory process, restoring proper blood circulation, and generally strengthening the patient’s body.
Preventive actions
There are two types of prevention - specific, aimed at preventing infection of the body with a specific pathogen, and nonspecific. For some types of neuroinfections, specific preventive measures have been developed, for example, vaccination against tick-borne encephalitis, polio and herpetic viruses.
Nonspecific prevention includes avoiding contact with infected people, treating concomitant diseases, using immunomodulators, etc.
You may also be interested in:
Treatment tactics
After analyzing all the information from diagnostic examinations, the doctor selects optimal schemes to combat the manifestations of neuroinfection, which is not always possible to do quickly due to the severity of the patient’s condition.
The main task of specialists is to choose drugs that will help quickly restore the full functioning of the brain:
- anti-inflammatory drugs - antibacterial medications that can penetrate nerve cells;
- analgesics – powerful, even narcotic drugs;
- medications that improve blood circulation in the brain structures;
- hormonal drugs - to increase the body's defenses, suppress the activity of the pathogen in the bloodstream;
- to increase immunity - vitamin complexes;
- to reduce temperature - antipyretics, means to combat temperature.
If a person does not seek medical help in a timely manner or does not fully comply with the doctor’s orders, the acute stage of the disease is accompanied by the appearance of complications. The consequences of neuroinfection are tragic: disability - severe disruption of brain activity does not allow a person to take care of himself and death.
To prevent such complications, as well as the occurrence of neuroinfection itself, experts recommend adhering to the basic rules of prevention - hardening, eating right, treating infections in a timely manner, and leading a healthy lifestyle.
Diagnosis and treatment of neuroinfection
A neurologist makes a diagnosis based on the picture of symptoms. The doctor examines the patient, his main goal is to differentiate a neuroinfection from any other acute neurological disease, as well as to determine the pathogenesis of the disease.
To confirm the diagnosis, laboratory diagnostics are often required, which involves testing blood and urine. All the characteristic features of an inflammatory reaction are observed in the blood: with bacterial meningitis - an increased number of white blood cells, with viral meningitis - their decrease from the generally accepted norm.
If a neuroinfection is suspected, a lumbar puncture is taken from the patient. Cerebrospinal fluid is collected to diagnose the severity of the disease and determine the causative agent. An increased amount of protein in the cerebrospinal fluid indicates the presence of a neuroinfection.
Depending on the type of meningitis, the level of glucose in the cerebrospinal fluid also differs - with tuberculous and fungal meningitis, a deviation in the glucose level is observed towards a decrease. When glucose is almost zero, this phenomenon is typical for purulent neuroinfections.
Brain swelling and high pressure inside the skull can be seen on a CT scan. The presence of inflammation in the brain tissue and meninges is visualized using an MRI procedure.
When a neurologist admits the presence of a neuroinfection in a patient, it is strongly recommended that the latter be hospitalized. If the patient comes to the clinic in serious condition, he is given prednisolone and benzylpenicillin. In the first three days, benzylpenicillin can be used directly into the spinal canal.
Based on the complexity of the course of neuroinfection of the brain, after establishing symptoms in adults, treatment is prescribed for the patient.
Treatment of meningitis consists, first of all, in the destruction of neuroinfection pathogens, pathogenetic therapy and relief from associated symptoms. At the first stage, the patient should take broad-spectrum antibiotics until the exact pathogen is identified. Etiotropic therapy also includes taking antiviral drugs.
During pathogenetic therapy, the patient is prescribed medications aimed at removing toxins from the body, and steroid drugs to stop the inflammation process.
It is important to get rid of the symptoms accompanying the neuroinfection. For example, vomiting and diarrhea can lead to dehydration, so the antiemetic drug Metoclopramide is prescribed. Insomnia causes constant fatigue; the body does not have enough of its own strength to fight the disease. To normalize sleep, sedatives are prescribed - Seduxen or Diazepam. If the patient experiences convulsions, it is advisable to stop them with Carbamazepine tablets.
All medications should be taken strictly as prescribed by the attending physician, do not change the dosage or skip medications.
Many patients are concerned about the consequences of neuroinfection, or more precisely, the question of how to recover after treatment and prevent relapse of the disease. After suffering an illness, it is recommended to periodically visit a neurologist in order to predict all possible complications of the disease.
Rehabilitation after meningitis:
- Nutrition. The body after an illness is quite weak, so nutrition should be balanced and healthy so as not to complicate the work of the gastrointestinal tract. Fried, fatty, smoked, overly salty and spicy foods will not be beneficial. It is recommended to consume lean meat and fish, preferably boiled or steamed. Fish can also be baked in the oven with vegetables. The porridge should be boiled with a small piece of butter. It is advisable to cook soups with a light broth without adding frying. It is allowed to include heat-treated dairy products in the diet.
- Physiotherapy. In case of dysfunction of the musculoskeletal system or problems with muscle groups, a neurologist may prescribe electrophoresis of vitamins to improve the patient’s condition. To restore the functioning of the central nervous system, magnetic laser treatment or electrosleep are used.
- Physiotherapy. Helps to rehabilitate after meningitis, if it is necessary to restore simple movements again.
- Occupational therapy. Treatment that helps the patient return to normal activities after illness. It includes a set of methods that allows a person to adapt in everyday life - to his usual lifestyle.
- Cognitive therapy. Classes with a specialist help restore memory, improve brain activity, and improve attention.
To prevent the disease, it is recommended to get vaccinated according to the schedule, promptly treat ARVI and other diseases, harden the body and take a course of vitamins and immune-strengthening drugs in the autumn-spring period.