PARIETAL AREA
PARIETAL AREA
[
regio parietalis
(PNA, JNA, BNA)] - the area of the cranial vault within the parietal bones.
On the skeleton, the lateral borders of the T. o. are the superior temporal lines (lineae temporales sup.) of the parietal bones; the anterior border runs along the line of the coronal suture (sutura coronalis), connecting the frontal and parietal bones, the posterior border - along the line of the lambdoid suture (sutura lambdoidea), connecting the parietal bones with the occipital bone (see Fig. 1 to Art. Head).
In T. o. The following layers are distinguished: skin, subcutaneous tissue, tendon helmet, or supracranial aponeurosis (galea aponeurotica) of the supracranial muscle, subgaleal tissue, periosteum, subperiosteal tissue, parietal bones, meninges.
Skin T. o. It is firmly connected by fibrous bridges to the tendon helmet, as a result of which it is little mobile. Subcutaneous tissue is rich in sweat glands; vessels and nerves of the parietal region pass through it. The tendon helmet is a monolithic tendon stretch that connects the frontal and occipital bellies of the occipitofrontalis muscle, under which lies a layer of loose fiber that separates the helmet from the periosteum. This determines the possibility of scalping the skin of the head along with a tendon helmet in certain types of skull trauma. The periosteum is connected to the bones of the skull through subperiosteal tissue; however, along the line of the sutures of the skull, the periosteum is firmly fused with them. The parietal bones are light and durable. In newborns, at the junction between the parietal, frontal and occipital bones, areas of connective tissue (the so-called fontanelles) are preserved, which usually ossify within 1.5 years. Non-closure of fontanelles at a later date is a significant sign of a violation of the general development of the child. On the inner surface, the bones of the skull are devoid of periosteum and are directly adjacent to the dura mater encephali. On the inner surface of the bones there are depressions from adjacent arteries, pachyonic granulations and convolutions of the brain.
According to the midline of the cranial vault, dividing the hemispheres of the brain, the so-called. the falx cerebri (falx cerebri), which is an outgrowth of the dura mater of the brain (see Meninges). Along the entire length of the sickle, in its upper part there is the superior sagittal sinus (sinus sagittalis sup.), which belongs to the venous system of the brain (see). The diameter of the sagittal sinus, together with the lacunae on both sides of the sagittal suture (sutura sagittalis), occupies within the T. o. approximately 25-30 mm, which is taken into account when trepanning in this area and assessing wounds in the sagittal suture area.
Vessels and nerves penetrate into the lake. from the forehead, back of the head and from the temporal regions, from where they are directed radially to the thoracic region. Here the vessels are connected to each other by numerous anastomoses, forming collateral networks that pass to the opposite side. Arterial network T. o. represented by branches of the supraorbital artery (a. supraorbitalis), originating from the system of the internal carotid artery (a. carotis int.), the edges anastomose with the branches of the superficial temporal (a. temporalis superficialis), posterior auricular (a. auricularis post.) and occipital (a. occipitalis) arteries, originating from the external carotid artery system (a. carotis ext.). In the venous system of the cranial vault, three types of vessels are distinguished: extracranial veins of soft tissues, diploetic veins (vv. diploicae), embedded in the spongy layer of bones, and sinuses of the dura mater. The veins of the integument of the skull and the veins of the spongy layer of bone communicate with the sinuses of the dura mater through emissary veins (vv. emissary). Of these, the most constant is the parietal emissary vein (v. emissaria parietalis), its edges open into the superior sagittal sinus.
Lymph, vessels T. o. flow into the pre-auricular (noduli lymphatici preauri-culares) and lower auricular (noduli lymphatici infraauriculares) lymph nodes.
Sensitive nerves pass into T. o. from the frontal, temporal and occipital regions, accompanying the arteries and veins.
The peculiarity of penetrating damage to T. o. (in addition to the danger of brain damage) there is a danger of violating the integrity of the superior sagittal sinus, which is accompanied by heavy bleeding (see) and requires urgent surgical intervention (see. Traumatic brain injury). Depressed (closed) fractures of the parietal bones also require surgical intervention, both in the presence and absence of neurol. symptoms of cerebral compression (see).
In T. o. dermoid cysts (see Dermoid), lipomas (see Lipoma), atheromas (see Epidermoid cyst), carbuncles (see Carbuncle), boils (see Furuncle), etc. may occur. As a rule, these processes have limited development here , which is explained by the density of the tissues covering the skull in this area.
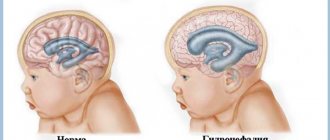
Through T. o. surgical approaches are used for certain neurosurgical operations. Most often, these approaches are used to expose the upper surface of the parietal lobe of the brain, penetrate the longitudinal fissure of the cerebrum, and to perform operations for damage to the superior sagittal sinus. Skin-aponeurotic and bone flaps for access to the parietal lobe are formed by an arcuate incision, the apex of which passes 20-30 mm from the sagittal suture, and the base reaches the temporal muscle (see Craniotomy). Access to T. o. a puncture of the corpus callosum is performed in case of hydrocephalus (see Hydrocephalus) in order to create an outflow of cerebrospinal fluid from the ventricles of the brain into the subarachnoid space (Anton-Bramann operation).
See also Head, Skull.
Bibliography:
Zolotko Yu. L. Atlas of topographic human anatomy, part 1, p. 6, M., 1964; And r g e r I. M. Neurosurgery, M., 1982; L u b o c k i y D. N. Fundamentals of topographic anatomy, p. 230, M., 1953; Ostroverkhov G. E., L u-botsky D. N. and Bomash Yu. M. Operative surgery and topographic anatomy, M., 1972; Surgery of the central nervous system, ed. V. M. Ugryu-mova, vol. 1, L., 1969.
G. E. Ostroverkhov.
Trichoscopy as a diagnosis of hair diseases
The term alopecia comes from the Greek “alopekia” - hair loss.
As you know, there are currently several diseases characterized by impaired hair growth.
- Androgenetic alopecia
- Alopecia areata
- Diffuse hair loss
Let us briefly consider each pathology.
Androgenetic alopecia
Thus, androgenetic alopecia is based on genetic predisposition, impaired sebum secretion and increased extraglandular synthesis of androgens.
With androgenetic alopecia, the typical places for hair loss and thinning are the anterior zone, the frontal-temporal angle, the anterior part of the temples, the central (horizontal) zone and the parietal region.
Alopecia areata
It is an autoimmune disease of the hair follicles, characterized by the formation of an inflammatory cellular infiltrate around the hair follicles, consisting of CD8+ and CD4+ lymphocytes, macrophages and Langerhans cells.
With alopecia areata, hair falls out on clinically unchanged skin without signs of inflammation, atrophy and subjective sensations, forming round-shaped lesions with a pronounced zone of loose hair along the periphery, which can later merge, forming large lesions.
Diffuse hair loss
The causes of this pathology are very diverse. The cause may be seborrheic dermatitis, exposure to toxic substances, metabolic disorders, deficiency conditions, physiological causes, etc.
With this pathology, hair falls out over the entire surface of the head. To diagnose such pathological conditions, the trichoscopic examination method is currently used.
Visualization diagnostics currently firmly holds its position as one of the most accessible, low-cost, painless, effective diagnostic methods in dermatology (trichology). This method has appeared relatively recently in world medicine. Thus, foreign researchers Kossard and Zagarella were among the first to study a case of cicatricial alopecia and describe its dermoscopic criteria in 1993. Then, in 2003, video microscopic criteria for the severity of androgenetic alopecia and methods for dynamic monitoring of the effectiveness of therapy were described for the first time. In 2005, video microscopic criteria for the severity of androgenetic alopecia were described.
The founder of trichoscopy can be considered Rudnicka, who in 2006 introduced the term “Trichoscopy” and began to use it in assessing the condition of hair, scalp, eyebrows, eyelashes using videodermoscopic technology.
Currently, a video camera is used for visualized diagnostics, which is connected to a laptop or desktop computer.
Fig.1.
Figure 1 shows a camera from the Korean company Aramo, which has a resolution of 410,000 pixels and magnification of 1x, 60x, 200x, 1000x, as well as disinfection of the lens using UV irradiation, which prevents the spread of infection from patient to patient and does not require additional treatment lens with disinfectant solutions.
Such a camera is optimal for use together with the domestically developed Trichoscience program, which allows you to maintain a patient database, automatically calculate hair density in any area of the head, measure hair diameter and automatically assess what phase of development the hair is in, carry out the phototrichogram method (which is used for differential diagnostics of androgenetic and diffuse alopecia, as well as to assess the effectiveness of therapy), and make an automatic diagnosis based on an assessment of visualized data.
As a rule, two areas of the head are examined:
- androgen-independent - parietal region
- androgen-dependent - occipital region, in which hair density and variability of its diameter are calculated.
Normally, hair density in the parietal zone is 25% higher than in the occipital zone and is.
| Parietal zone | Occipital zone | |
| 300±20/cm² | 195±13/cm? | for brunettes |
| 340±25/cm? | 210±12/cm? | among blondes |
Hair in the anagen stage - 80%, telogen - 10%.
The number of dysplastic hairs, the diameter of which is less than 0.04 mm, does not exceed 10%.
With diffuse hair loss, uniform hair loss is observed over the entire surface, including the parietal and occipital zones.
Parietal zone
5-displast (12%), 29-norm (88%),
260 per cm2 (norm 300±20/cm?)
Occipital zone
3-displast (10%), 27-norm (90%) 167 per square cm. (normal 195±13/cm?)
Green color indicates normal hair (terminal), red color indicates dysplastic hair (vellus).
With androgenetic alopecia, there is a significant decrease in hair density and diameter in the parietal zone with normal hair content in the occipital zone.
Parietal zone
17-displast (43%), 22-norm (56%) 217 per square cm. (norm 300±20/cm?)
Occipital zone
7-displast(18%), 31-norm(81%) 212 per sq. cm. (normal 195±13/cm?)
To diagnose alopecia areata, there are several trichoscopic signs (yellow dots and cadaverized hair).
To make an accurate diagnosis, the phototrichogram , which is used for:
- for accurate counting of the number of hairs per cm?;
- determining the amount of anagen and telogen hair in a given area;
- the amount of dysplastic and normal hair, as well as the intensity of hair loss and the degree of hair thinning;
- to carry out a differential diagnosis between androgenic and diffuse types of hair loss;
- calculating individual hair growth rate;
- Carry out dynamic monitoring of the rate of hair growth under the influence of treatment; for this purpose, it is advisable to carry out a phototrichogram once every 3-5 months.
Phototrichogram technique
In two zones (parietal and occipital), hair is shaved off with a trimmer in an area measuring 8x8mm. After 2-3 days, when the hair has grown by 1 mm (normally 0.3-0.4 mm per day) or remains the same size (anagen and telogen hair, respectively), the areas are tinted with ammonia-free hair dye, and using a trichoscope, connected to a computer, under x40 magnification they are entered into a specialized computer program (Trichoscience).
Phototrichogram for diffuse hair loss.
Parietal region
Anag.-71%(disp.14%) Tel. -28% (disp. 18%) hair density 262.55 per square cm.
(norm 300±20/cm?)
Occipital zone
Anag.-70%(disp.11%) Tel.-30%(disp.15%) hair density 140.21 per sq. cm.
(normal 195±13/cm?)
Phototrichogram for androgenetic alopecia
Parietal zone
Anag.-51%(disp.50%) Tel.-48%(disp.52%) hair density 212.28 per square cm.
(norm 300±20/cm?)
Occipital zone
Anag.-81%(disp.8%) Tel.-19%(disp.11%) hair density 262.55 per sq. cm.
(normal 195±13/cm?)
There is a decrease in density, a high percentage of telogen and dysplastic hair in the parietal zone, and in the occipital zone these indicators remain normal.
Cortical centers of the parietal lobe of the brain.
5>
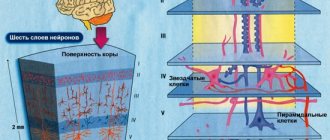
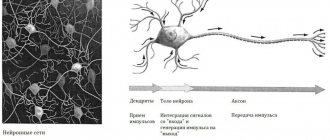
1. Center for General Sensitivities
located in the parietal lobe behind the central sulcus (Roland's sulcus) and is a bilateral center. The sensitive centers of the legs are located in the upper section, the arms in the middle section, and the heads in the lower section. If the center is damaged, there is a decrease or loss of sensitivity (temperature, pain, tactile) of the corresponding areas of the body surface.
2. Center for the perception of complex types of sensitivity
– a bilateral center, located in the superior parietal lobule, is responsible for the perception of localization, weight, and two-dimensionality of space.
3.
located inside the parietal sulcus. Lesions of the center lead to violations of the correct ideas about the size, shape, location of parts of one’s body (disorder of the “body diagram”).
4. Praxia Center
located in the supramarginal gyrus of the right and left hemispheres.
It ensures the execution of complex targeted movements in a certain sequence. When the center is damaged, disturbances in purposeful movements and actions ( apraxia
) occur while its constituent elementary movements are preserved.
There are apraxias:
– ideational
(apraxia of intention) - a disorder in the sequence of movements when performing a task (the patient performs actions that are not necessary to achieve the goal; the actions are correct, but their sequence is disrupted, imitation actions are preserved, bilateral apraxia);
– motor
(apraxia of execution) - a disorder of acting on orders or imitation; unilateral apraxia;
– constructive apraxia –
the inability to construct a whole from parts (figures from matches).
5. Stereognosia Center
located behind the middle part of the postcentral gyrus. If damaged, the ability to recognize objects by touch is impaired (tactile agnosia).
6. Lexicon Center
located in the angular gyrus of the left hemisphere in right-handed people, it is responsible for the ability to recognize printed characters and read.
alexia
occurs - a disorder in understanding written and printed characters, and the inability to read.
7. Account Center
(
calculia
) is located above the angular gyrus.
When the center is damaged, the ability to count is impaired - acalculia
.
8. Center for Semantic Aphasia
located in the convergence area of the parietal, occipital and temporal lobes. If damaged, the ability to understand complex logical-grammatical, temporal, and spatial speech structures is impaired (Fig. 11).
5>
Date added: 2017-05-02; views: 3989; ORDER A WORK WRITING