What is cerebral gliosis
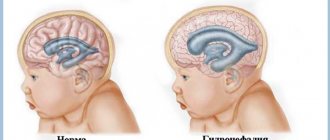
The natural process of replacing dead neurons, which is protective in nature, is called gliosis of the white matter of the brain. Normally, over 10 years in a healthy body, about 4% of all neurocytes are destroyed, so gliosis is one of the manifestations of aging.
With the development of pathological processes that cause the death of a large area of nervous tissue, gliocytes replace dead impulse cells, although they cannot generate and conduct nerve impulses. Thanks to this, the spread of the pathological process slows down, and the metabolism of the affected area is preserved in full.
What causes the development of gliosis of brain tissue, what it is and at what point the process becomes dangerous
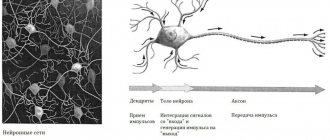
The CNS includes three types of cells:
- Neurons are the main functional cells of the nervous system, forming and transmitting impulses from the brain to effectors (executive organs that provide a response to a specific stimulus).
- Ependymal cellular elements lining the ventricles of the brain and the central spinal canal.
- Cells of glial tissue with supporting and protective functions. They form a scar after the death of neurocytes for various reasons, including due to demyelinating diseases.
Glial tissue (neuroglia) is located between the functional elements and is the support for all cellular structures. Normally, it protects the brain from injury due to sudden movements, as well as from the development of infectious processes.
Making up about 40% of the volume of all tissues of the skull, glia creates the conditions for the normal functioning of the nervous system. In critical situations, it forms a kind of scar, which does not allow metabolic processes to stop and partially takes over the tasks of other cells. In addition, neuroglia participate in the formation of new nerve fibers that isolate the lesion and protect healthy tissue.
Gliosis of the white matter of the brain - what is it?
For some reason, nerve cells may begin to die in the human brain. Some diseases and conditions can provoke this.
The disease begins with a single area of such a lesion, gradually this area grows, and in place of dead neurons, glia - scar-like tissues that protect the organ from various infections and injuries. Large accumulations of glia form gliosis.
The job of glial cells is to protect the brain. Forming at the site of damage to organ tissue, glia protect the damaged area by enveloping it. If the death of neurons occurs in large numbers, glia cover large areas of the brain, then the nervous system ceases to function normally.
The degree of brain damage is determined by the number of lesions; depending on this, doctors diagnose the type of disease.
Gliosis comes in several types, depending on the location and degree of proliferation of gliosis cells.
Kinds
- Anisomorphic gliosis is diagnosed if the cell fibers are located chaotically.
- The fibrous appearance of this disease is determined by the more pronounced formation of glial cells than the cellular component.
- The diffuse type of the disease means that the area of damage to the brain is very large.
- The isomorphic form of this disease occurs in patients when the glial fibers are located relatively correctly.
- Marginal gliosis is caused by the proliferation of glial cells only in the intrathecal areas of the brain.
- The perivascular type of this disease occurs with atherosclerosis of cerebral vessels. Glial fibers are formed surrounding the affected vessels.
- The subependymal appearance means that the glial growth zone is located under the epindyma.
of diseases that cause gliosis of the white matter of the brain. Even the most banal ailments, which occur quite often, can act as a provocateur of this disease.
Here you can read in detail about gliotic changes in the brain.
Symptoms
Clinical signs of neurogliosis depend on the underlying disease that caused its development. Single small lesions do not cause specific symptoms and are detected during MRI for another disease. The following symptoms cause concern:
- headaches that develop for no apparent reason, are long-lasting, of high intensity and do not go away after taking antispasmodics;
- unstable blood pressure (sharp decrease or increase in blood pressure within a short time);
- periodic dizziness;
- increased fatigue and decreased performance;
- emerging changes in auditory and visual perception;
- memory and attention disorder;
- the occurrence of motor disorders (with large lesions, up to convulsive conditions).
There is a direct dependence of clinical manifestations on the location of the focus of gliosis
- Supratentorial gliosis is manifested mainly by visual disorders - distortion of the size, shape and outline of objects, hallucinations, loss of visual fields, inability to recognize an object by appearance.
- Damage to the temporal lobes is characterized by prolonged and frequent headaches. If the lesion is vascular in nature, then the pain syndrome is accompanied by sharp changes in blood pressure.
- Gliotic changes in white matter can cause dizziness, increased seizure activity and the development of epileptic seizures. More often, such symptoms develop as a result of traumatic brain injuries or as a complication of surgery.
- The localization of the lesion in the frontal lobes in most cases is an age-related change. If there were no diseases that could activate the proliferation of glial cells, the process refers to the primary pathology:
- developing in older people
- manifested by impaired memory and attention, slowed reactions, and imprecise fine motor skills.
In the absence of adequate treatment of the underlying disease, glial lesions increase in size. This leads to the progression of clinical manifestations and the development of complications.
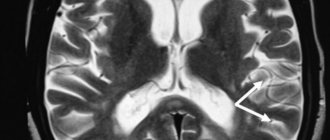
Periventricular lesions on brain MRI
DIFFERENTIAL DIAGNOSIS OF WHITE MATTER LESIONS
The differential diagnostic range of white matter diseases is very long. MRI-detected lesions may reflect normal age-related changes, but most white matter lesions arise during life and as a result of hypoxia and ischemia.
Multiple sclerosis is considered the most common inflammatory disease, which is characterized by damage to the white matter of the brain. The most common viral diseases that lead to the appearance of similar lesions are progressive multifocal leukoencephalopathy and herpesvirus infection. They are characterized by symmetrical pathological areas that need to be differentiated from intoxication.
The complexity of differential diagnosis in some cases necessitates additional consultation with a neuroradiologist in order to obtain a second opinion.
WHAT DISEASES ARE FOCIED IN THE WHITE MATTER?
Focal changes of vascular origin
- Atherosclerosis
- Hyperhomocysteinemia
- Amyloid angiopathy
- Diabetic microangiopathy
- Hypertension
- Migraine
Inflammatory diseases
- Multiple sclerosis
- Vasculitis: systemic lupus erythematosus, Behcet's disease, Sjögren's disease
- Sarcoidosis
- Inflammatory bowel diseases (Crohn's disease, ulcerative colitis, celiac disease)
Infectious diseases
- HIV, syphilis, borreliosis (Lyme disease)
- Progressive multifocal leukoncephalopathy
- Acute disseminated (disseminated) encephalomyelitis (ADEM)
Intoxications and metabolic disorders
- Carbon monoxide poisoning, vitamin B12 deficiency
- Central pontine myelinolysis
Traumatic processes
- Radiation therapy related
- Post-concussion lesions
Congenital diseases
- Caused by metabolic disorders (they are symmetrical in nature and require differential diagnosis with toxic encephalopathies)
Can be observed normally
- Periventricular leukoaraiosis, grade 1 according to the Fazekas scale
MRI OF THE BRAIN: MULTIPLE FOCAL CHANGES
The images reveal multiple pinpoint and “spotty” lesions. Some of them will be discussed in more detail.
Watershed-type heart attacks
- The main difference between heart attacks (strokes) of this type is the predisposition to localize foci in only one hemisphere on the border of large blood supply basins. The MRI shows an infarction in the deep rami basin.
Acute disseminated encephalomyelitis (ADEM)
- The main difference: the appearance of multifocal areas in the white matter and in the area of the basal ganglia 10-14 days after infection or vaccination. As with multiple sclerosis, ADEM may involve the spinal cord, arcuate fibers, and corpus callosum; in some cases, lesions may accumulate contrast. The difference from MS is that they are large in size and occur predominantly in young patients. The disease has a monophasic course
Lyme disease
- It is characterized by the presence of small lesions 2-3 mm in size, simulating those in MS, in a patient with a skin rash and influenza-like syndrome. Other features include hyperintense signal from the spinal cord and contrast enhancement in the root zone of the seventh pair of cranial nerves.
Sarcoidosis of the brain
- The distribution of focal changes in sarcoidosis is very similar to that in multiple sclerosis.
Progressive multifocal leukoencephalopathy (PML)
- Demyelinating disease caused by John Cunningham virus in immunocompromised patients. The key feature is white matter lesions in the area of the arcuate fibers that do not enhance with contrast and have a volumetric effect (unlike lesions caused by HIV or cytomegalovirus). Pathological areas in PML can be unilateral, but more often they occur on both sides and are asymmetrical.
Virchow-Robin spaces
- Key sign: hyperintense signal on T2WI and hypointense on FLAIR
Vascular lesions
- For zones of a vascular nature, deep localization in the white matter is typical, with no involvement of the corpus callosum, as well as the juxtaventricular and juxtacortical areas.
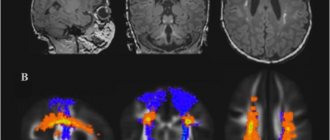
DIFFERENTIAL DIAGNOSTICS OF MULTIPLE FOCI ENHANCED WITH CONTRAST
MRI scans demonstrated multiple pathological zones accumulating contrast agent. Some of them are described in more detail below.
Causes of gliosis
Gliosis is not an independent disease; it is a morphological manifestation of a number of pathologies. The reasons that caused the accelerated proliferation of neuroglial cells may be:
Genetically determined diseases
- lysosomal storage disease (Tay Sachs disease), characterized by the death of a large number of neurons in children from six months of age;
- tuberous sclerosis, manifested by the formation of multiple benign tumors in various organs;
- multiple sclerosis – demyelination (destruction of the covering myelin sheath) of nerve fibers of various parts of the central nervous system.
Congenital and intrauterine pathologies
The cause of the appearance of foci of gliosis in the white matter of the child’s brain in this case is:
- oxygen starvation (hypoxia) during fetal development or childbirth;
- birth injuries of varying severity;
- increased levels of carbon dioxide in the blood (hypercapnia);
- infectious diseases transmitted in utero.
Classification
- Astrocytomas are the most common type of glioma, localized in the white matter of the brain. Depending on the type, astrocytic glioma of the brain can be fibrillary (protoplasmic, gemistocytic), anaplastic, glioblastoma (giant cell, gliosarcoma), pilocytic astrocytoma, pleomorphic xanthoastrocytoma, and subependymal giant cell astrocytoma.
- Ependymomas - can occur in 5-7% of cases of brain tumors, are characterized by typical localization in the ventricular system of the brain.
- Oligodendrogliomas account for 8 to 10% of all brain tumors and develop from oligodendrocytes.
- Chiasmal glioma - spreads along the optic nerve into the orbital cavity, can grow into the hypothalamus, and affect the third ventricle of the brain. This tumor causes endocrine imbalance, metabolic disorders, decreased vision, and is characterized by intracranial hypertension, depending on the location and size of the tumor.
- Mixed gliomas – oligoastrocytomas, anaplastic oligoastrocytomas.
- Neuromas make up 8 to 10% of tumors.
- Choroid plexus tumor is a rare type of glioma, occurring in 1-2% of cases.
- Neuroepithelial tumor of unknown origin - this group includes astroblastoma and polar spongioblastoma.
- Diffuse glioma of the brain stem is a tumor with a high degree of malignancy, cancer of the central nervous system. People of any age are affected, but the tumor is rare in adolescents and children. The survival prognosis for this type of tumor is poor. Diffuse glioma develops in the area of the brain in which all the important nerve connections are located, providing communication between the analyzing nerve centers of the brain and the impulses of the musculoskeletal system of the extremities. The tumor very quickly causes paralysis.
- Neuronal and mixed neuronal-glial tumor - occurs in extremely rare cases (up to 0.5%). This group includes gangliocytoma, ganglioglioma, neurocytoma, neuroblastoma, neuroepithelioma).
- Gliomatosis cerebri.
Forms and degrees of development
According to morphological characteristics:
- isomorphic form of gliosis – characterized by ordered proliferation of neuroglia;
- anisomorphic type of disease – characterized by a predominance of cellular structure and chaotic growth;
- fibrous form – signs of a predominant fibrous structure are clearly expressed.
Based on the nature of the process and its prevalence, they speak of:
- The focal type of the course is a limited area of gliosis (usually in the parietal or temporal lobes), the cause of which was trauma, an infectious or inflammatory process.
- Diffuse type of course – multiple lesions of various sizes and locations. Cystic-gliotic formations of vascular origin are often found.
Depending on the location of the foci, gliosis is divided into:
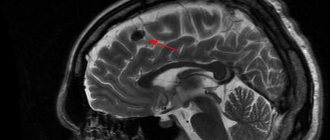
- Periventricular gliosis - glial proliferations are localized in the area of the ventricles of the brain.
- Perivascular location of foci (vascular gliosis) is the most common type of course. It is distinguished by the presence of glial growths along atherosclerotic vessels. Diagnosed as microangiopathy with the presence of single or multiple foci of gliosis. The variety is the subtentorial type (a few lesions appear as a result of birth injuries or age-related changes, and multiple lesions arise as a consequence of circulatory disorders).
- Subependymal - single lesions localized on the inner lining of the ventricles.
- Marginal - foci of glial degeneration are located in the intrathecal region.
- Marginal - areas of replacement glial tissue are located on the surface of the brain.
Types of gliosis
A glial focus is an accumulation of a large number of glial cells. Gliotic lesions in the brain are divided into the following subtypes based on location:
- Periventricular gliosis - changes form in the ventricles; as a rule, the pathological process is accompanied by the development of cysts.
- Diffuse - foci of gliosis form in the white matter of the brain, the total number of pathogenic foci is so large that pathological changes cover the entire area of the brain, and also spread to the spinal region.
- Perivascular - pathological changes develop due to sclerosis of blood vessels.
- Anisomorphic - pathological changes are located chaotically in the brain area.
- Marginal - glial cells are localized under the tissue membranes.
- Isomorphic - glial changes are correctly located in the brain.
In addition to the main types of gliosis, there is also a supratentorial focus of gliosis, which is of vascular origin. Such lesions can be isolated; they most often develop during the process of a newborn receiving a birth injury, and are also caused by physiological aging. Multiple foci of gliosis in the brain are formed due to disruption of the circulatory process. Single foci of gliosis almost always do not pose any threat to the body, but it is important to prevent the proliferation of glial cells. But multiple foci are already a pathological condition of neurological origin. Gliosis cells are not always attributed to focal origin; they often acquire a single character. This condition is most often provoked by the development of long-term arterial hypertension.
Foci of gliosis
Areas of neuroglial proliferation are a kind of scars at the site of dead neurons; they can be single, include up to 3 glial foci (few lesions) or multiple. The size of the growths can be calculated using the formula: the number of functioning neurocytes to the number of glial cells / per unit volume of tissue. Normally, this figure does not exceed 1:8/10.
With an increase in the number of gliocytes, the functioning of the central nervous system is disrupted, up to a convulsive syndrome. Neurologists believe that such a disruption of the central nervous system is often caused by subtentorial foci of gliosis of vascular origin or subcortical (subcortical) foci.
Single outbreaks
Small foci of gliosis do not cause symptomatic manifestations.
In a child, they are formed as a result of trauma received during childbirth, and the tissue of any lobe of the brain can be damaged.
But more often, single areas of glial changes are localized in the left or right parietal lobe.
In adults, the development of single foci of gliosis is caused by age-related changes or diseases of the central nervous system. Such areas practically do not change over time, therefore, in most cases, they cannot be identified without special examinations.
Multiple lesions
Multiple focal changes in brain tissue, as a rule, develop as a result of acute or chronic circulatory disorders. Forming foci of gliosis enhance the clinical picture of the disease that caused them.
Multiple foci of subtentorial gliosis of the brain appear as a result of traumatic brain injuries and hemorrhages in the tissue under the cerebellar tent. This zone is vulnerable due to the surrounding incompressible spaces filled with cerebrospinal fluid.
Multiple focal changes in the brain substance of a dystrophic nature develop with insufficient blood supply, chronic diseases of the central nervous system, and also as a result of age-related changes.
Supratentorial lesions
The supratentorial formations of the brain include the structures lying above the process of the dura mater - the tentorium of the cerebellum (from the Latin supra - above + tentorium - cerebellum).
They belong to the upper parts of the brain, in contrast to the subtentorial ones, which include the cerebellum and brain stem.
The occipital lobe, located above the tentorium, most often suffers from head bruises and birth injuries due to the fact that it is surrounded on all sides by the fluid of the cerebrospinal fluid spaces, which is incompressible upon impact. In this lobe, glial growths of vascular origin, not associated with injuries, most often occur.
According to the extent and prevalence, supratentorial gliosis is:
- Focal – localized in the form of a large single proliferation of neuroglial cells;
- Few (the term is used to reflect the presence of 2-3 lesions);
- Multiple, which is characterized by the presence of more than 3 hyperdense formations;
- Diffuse (multi-focal), affecting various parts of the brain. The number of small lesions in this case cannot be counted.
The clinical picture of the disease correlates with the number of dead neurons and the size of the lesion. A small formation of neuroglia may not make itself known.
The more extensive the process, the more vivid the clinical picture of damage to the occipital lobe becomes.
Which doctor should I contact?
If you suspect the presence of gliosis, you should consult a neurologist. After the studies have been carried out, consultation with specialists may be required to confirm the diagnosis and determine treatment tactics:
- cardiologist - if gliosis of vascular origin is suspected;
- general practitioner or family doctor - to determine chronic diseases;
- endocrinologist – for diabetes mellitus;
- neurosurgeon - if surgical treatment is necessary.
In children, a neonatologist can suspect the development of glial changes during the first month after birth. Later, developmental changes are identified by a pediatrician who will refer the child to a consultation with a pediatric neurologist.
Diagnostics
Cystic-glial changes in brain tissue can only be detected through special studies. Methods for instrumental diagnosis of gliosis include:
- EEG - severe gliosis can provoke the appearance of epileptic seizures. Therefore, if there are changes in brain activity, an electroencephalogram is performed.
- Computed tomography with contrast – using angiography, deviations in the functioning and structure of cerebral vessels are determined.
- Magnetic resonance imaging is the most accurate method for diagnosing various types of disease. Thanks to the results of MRI, it is possible to determine the presence of foci of demyelination, volume, location and cause of glial changes.
- To determine gliosis in the fetus up to 20 weeks, amniocentesis is performed.
Types of gliosis
Depending on the location of the areas of replacement of functional brain cells with glial tissue, the following forms of pathology are distinguished:
- anisomorphic;
- fibrous;
- diffuse;
- edge;
- focal;
- perivascular;
- periventricular.
Each variety has its own characteristics.
Gliosis of the brain
In the fibrous form, neuroglia predominate, differing in their fibrous structure.
The anisomorphic form of the pathology is accompanied by chaotic growth of the supporting tissues of the brain. In this case, the cellular structure of neuroglia remains predominant.
The diffuse type of gliosis is characterized by the absence of pronounced foci of replacement. Such a disorder often occurs against the background of an ischemic process.
The focal variant of gliosis is extremely common. It is characterized by the presence of replacement sites with clear boundaries. Gliosis of the white matter of the brain most often occurs in this form. Often the disorder occurs against the background of an inflammatory process.
The marginal variant of the pathology is accompanied by the appearance of small lesions on the surface of the brain.
Perivascular gliosis is characterized by the proliferation of neuroglia around blood vessels affected by sclerosis. Often such pathology occurs against the background of systemic vasculitis.
Periventricular gliosis is characterized by the proliferation of auxiliary tissue in the area of the ventricles of the brain.
Treatment
There is no specific therapy for gliosis. Treatment methods depend on the underlying disease that caused the death of neurons. Main goals of therapy:
- slow down the progression of the process;
- ensure normal trophism of central nervous system tissues;
- eliminate oxygen starvation;
- normalize metabolic processes.
Traditional medicine
To eliminate the symptoms of brain changes, the following groups of drugs are prescribed:
- Vasoactive - drugs that activate cellular metabolism and improve tissue trophism (Cavinton, Vinpocetine).
- Antiplatelet agents are drugs that slow down platelet sedimentation (all derivatives of acetylsalicylic acid).
- Agents that improve the condition of the walls of small and large arteries (Ascorutin, vitamins).
- Nootropic substances - they increase the resistance of the central nervous system to the effects of negative factors (Piracetam, Nootropil).
- Statins – have lipid-lowering properties, preventing the development of atherosclerosis (Fenofibrate, Atorvastatin).
- Painkillers and antispasmodics to relieve headache attacks.
Surgery
Surgery for gliosis is prescribed extremely rarely.
Only for single large lesions. After surgery, treatment of the underlying disease that caused the death of neurons must be continued to avoid the development of relapses.
Indications for surgical intervention for a large single lesion are:
- violation of the outflow of fluid (CSF);
- convulsive seizures caused by a large area of gliosis;
- diagnosed neoplasm;
- changes in the functioning of internal organs.
With multifocal gliosis, only constant conservative treatment has a positive effect.
Complementary and alternative methods at home
Traditional medicine methods can be used only after consultation with a neurologist. Homeopathic remedies are prescribed as concomitants against the background of conservative therapy.
Decoctions and infusions of medicinal plants and fruits improve the functioning of the cardiovascular system and stimulate metabolism.
Diet for gliosis changes
The diet for gliosis is aimed at:
- Improving brain function and relieving vascular spasms. To achieve this result, you need to eat foods rich in magnesium: buckwheat, pearl barley, corn cereals, nuts, pumpkin seeds, lentils, cabbage of all varieties, figs.
- Relieving edema, improving heart function - foods with a high potassium content are introduced into the diet: citrus fruits, green vegetables and fruits, dried fruits, mushroom and potato dishes.
- Weight loss - to control body weight, remove baked goods, canned food, carbonated sweet drinks, smoked foods, fatty meats, fast food and semi-finished products from the daily diet.
The daily diet consists of fish, lean meat, cereals, fermented milk products, hard cheese, vegetables, nuts and fruits. It is better to steam, boil or bake foods.
Complications and consequences
The presence of extensive areas of replacement of neurons with gliocytes threatens with dangerous consequences:
- persistent headaches that cannot be controlled by medications;
- mental disorders;
- permanent loss of speech, vision or hearing;
- convulsions and epileptic seizures;
- paralysis (partial or complete);
- mental disorders;
- impaired coordination of movements;
In extremely rare cases, gliosis of non-genetic origin causes death.
Symptoms and consequences
Gliosis will not cause symptoms. Signs of pathology arise due to damage to functional tissue. The development of gliosis is detected during the diagnosis of the primary disease.
Depending on the form, localization and extent of the process, patients with this pathology may experience the following complaints:
- headache;
- blood pressure changes;
- attacks of dizziness;
- weakness;
- deterioration of vision and hearing;
- increased fatigue;
- deterioration in coordination of movements.
Memory deterioration is often observed. Sclerosis gradually develops, accompanied by an inability to remember information and loss of previously acquired skills and knowledge. Possible decrease in intellectual abilities.
Prevention
In order to prevent the spread of outbreaks, you must follow a few simple rules:
- lead a healthy lifestyle with feasible physical activity;
- adhere to the diet chosen by the nutritionist;
- to refuse from bad habits;
- observe the work and rest schedule;
- follow all doctor's orders.
The replacement of dead neurons with gliocytes is a physiological compensatory process that ensures the functionality of the brain in case of non-critical damage. However, the appearance of areas of gliosis indicates the presence of other diseases that threaten the health of the central nervous system, which must be treated promptly and in full.