Multiple sclerosis (MS) is a serious chronic disease characterized by damage to the myelin sheath of nerves, which explains the appearance of symptoms. Every patient who is diagnosed is diagnosed with one of four types of MS. The symptoms of multiple sclerosis and the characteristics of its course depend on this. But this is not a static value, since as the disease progresses, the nature of the course changes.
A little about the features of the disease
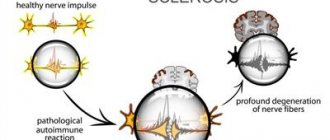
Multiple sclerosis is an autoimmune disease, i.e. at some point the body begins to produce antibodies to the proteins of the myelin sheath of its own nerves, forming sclerotic plaques of connective tissue. The word “scattered” means that many connective tissue plaques are randomly located along the nerve fiber. Plaques are distributed throughout the white matter of the brain and spinal cord. Their sizes vary - from one millimeter to several centimeters. Sometimes plaques can merge. New plaques alternate with old ones, on the periphery of which the myelin sheath has again begun to form. Different parts of the nervous system are affected simultaneously, which makes diagnosis very difficult.
The typical age of onset of multiple sclerosis is from 14 to 40 years, but there are cases of onset at 8-10 and 50-60 years. Up to 50 years of age, women get sick more often; at older ages, the frequency levels off. In Russia, per 100 thousand in different regions, from 30 to 70 people get sick. People get sick more often in cities - the larger the city, the higher the frequency of diseases in it.
The further north people live, the more often they suffer from multiple sclerosis.
Doctors have long noticed a connection between the frequency of the disease and distance from the equator. In hot countries, people practically do not suffer from multiple sclerosis, and the less light there is and the further north, the more patients there are. The maximum prevalence is noted in Sweden and Norway, but in Korea, China and Japan it is practically not found.
The frequency of cases also depends on skin color. White Europeans are susceptible to the disease, but people with dark or yellow skin tones are practically not affected.
Multiple sclerosis was first described by the famous French physician Charcot in the second half of the 19th century; since then, the study of this disease has not stopped. There are international scales for assessing the state of functional systems and assessing disability. These scales make it possible to bring the assessment of a sick person’s condition to a single denominator in different countries.
Additional evidence
Antiviral therapy for multiple sclerosis is being pursued by the Swiss-French company GeNeuro with its experimental temelimab. According to one hypothesis, some viruses can give impetus to the development of multiple sclerosis.
Thus, multiple sclerosis-associated retrovirus (MSRV), which belongs to the pathogenic W family of human endogenous viruses (pHERV-W), can be transactivated by external factors, for example, human herpes virus type 6 (HHV-6) or Epstein-Barr virus. The result is the generation of the pathogenic envelope protein MSRV-Env, which, by overactivating the endogenous toll-like receptor 4 (TLR4), triggers a pro-inflammatory cascade and suppression of remyelination.
Temelimab (GNbAC1) is a recombinant humanized monoclonal antibody that selectively targets the extracellular domain of MSRV-Env for its neutralization.
Types of flow
According to the international classification, the following types of multiple sclerosis are distinguished:
- relapsing – remitting;
- secondary - progressive;
- primary - progressive;
- progressive - recurrent.
The course can be benign and malignant. A benign course is considered to be one in which, after 15 years from the onset, the person has not become disabled. With a malignant course, there are practically no remissions.
Special types include rare diseases: Devic's neuromyelitis optica, Schilder's disease or diffuse cerebral sclerosis, Ballot's concentric sclerosis.
The remitting course is the most common, recorded in 90% of primary cases.
Graphically, the flow types look like this:
Types of multiple sclerosis
With the remitting type, exacerbations alternate with remissions, the overall decrease in quality of life increases gradually or remains at the same level. With each subsequent exacerbation, a new symptom may appear or an old one may recur. At least 30 days pass between exacerbations. The prognosis for this type of course is favorable; patients can remain functional for years or decades.
Prevention
Since the pathology is not fully understood, there are no specific preventive recommendations. Doctors recommend a correct and healthy lifestyle without strong emotional outbursts. To reduce the frequency of exacerbations in multiple sclerosis, you need to adhere to the following simple recommendations:
- regular feasible loads;
- minimum stress and mental strain;
- rejection of bad habits;
- weight loss, if necessary;
- strict compliance with all medical instructions during acute periods;
- proper nutrition with limited fatty foods.
Find out what vitamins you need to take for this disease here.
The insidiousness of the disease
Modern neuroimaging methods make it possible to detect foci of demyelination in the early stages. The standard examinations in this case are magnetic resonance imaging and, less common in our country, positron emission or radionuclide studies. However, no one goes for examination for no apparent reason. The insidiousness of multiple sclerosis is that clinical manifestations begin when at least 40% of neurons are affected; until this stage, the course is asymptomatic. Many newly identified cases have been described in which more than 50% of the nerve fibers were affected. It is clear that with such massive damage, the possibilities of healing are extremely limited. Detection of foci of demyelination in the early stages is an accidental finding, and it is not possible to change this in the near future.
In recent years, people have started talking about clinically isolated symptoms that cause medical caution. This may include numbness, weakness of a small muscle group, urinary retention, and blurred vision. Only one symptom appears, but it also “passes” without treatment within 2-3 days. During this time, almost no one gets to the doctor. It is possible to understand that this was the debut of a formidable disease only in retrospect, when a clear clinical picture unfolds several years later.
If you have unclear symptoms, it is always better to undergo an MRI.
Principles of treatment
There is no etiotropic treatment for relapsing-remitting sclerosis, so pathogenetic therapy is used. When the disease worsens, the patient is prescribed glucocorticosteroids:
- Methylprednisolone.
- Prednisolone.
To suppress the activity of the immune system, the patient is shown cytostatics:
- Cyclosporine.
- Cyclophosphamide.
- Azathioprine.
As for relatively new treatment methods, Betaferon or Rebif are prescribed. In some cases, the following are prescribed:
Copaxone.- Mitoxantrone.
- Natalizumab.
Symptomatic treatment involves the use of the following medications:
- to relieve muscle tone - Mydocalm ;
- for problems with urination - Proserin ;
- for tremor - Phenazepam ;
- for depression - Paroxetine ;
- for seizures - Finlepsin ;
- to improve the functioning of the nervous system - Nootropil or Cerebrolysin .
Traditional medicine can be used as additional therapy. In this case the following is used:
- Wheat sprouts. Pour the washed grains with water and wait until sprouts appear up to 2 mm. Scroll the raw materials through a meat grinder, pour in milk and mix everything well. Take the resulting remedy on an empty stomach for a month, then take a break for two weeks and repeat the course.
- Propolis. Mix 10 grams of propolis with 90 grams of butter, take half a teaspoon several times a day, you can add honey.
Damage to the nerve fiber
Determined by the stage of development of the sclerotic plaque. Some nerves behave as if in simple inflammation - the myelin sheath swells, is destroyed and immediately begins to be synthesized again. The speed of nerve impulse conduction drops sharply. True, the rate of remyelination or reverse development is low, so the symptoms last a long time. The longer the duration of the disease, the lower the rate of remyelination.
If a lot of myelin is destroyed, then the exposed axial cylinders also begin to collapse. This is much worse, because they are practically irreparable. Following the axial cylinders, the nerve cells completely die. Finally, the last to disappear are the oligodendrocytes, or the cells that form axons and myelin. One oligodendrocyte “serves” several mature neurons, and after its death the entire zone dies out.
At this time, on MRI it is already possible to see foci of atrophy of the substance of the brain and spinal cord. These lesions are most often located around natural voids or ventricles through which cerebrospinal fluid or cerebrospinal fluid circulates. The death of neurons causes expansion of the ventricles and disturbances in liquorodynamics.
In the same patient, fresh plaques, areas of demyelination and recovery, and foci of irreversible sclerosis can be detected. Their location determines the symptoms of the disease and its course.
Nerve fiber loss can range from 10% at the onset of the disease to 80% in the final stages.
Symptoms of Multiple Sclerosis
Traditionally, they are divided into classic or typical and rare, based on the frequency of occurrence.
Classic symptoms include:
- damage to the pyramidal tract or voluntary movements;
- coordination problems;
- lesions of the optic and oculomotor group of cranial nerves;
- damage to the facial, cochleovestibular and trigeminal nerves;
- sensitivity disorders;
- dysfunction of the pelvic organs;
- mental disorders.
Rare symptoms include:
- paroxysmal states;
- epileptiform seizures;
- acute psychoses;
- transverse myelitis;
- afferent or sensory paresis in one hand;
- autonomic disorders;
- polyneuropathy;
- various pains.
Classic symptoms
The first place in frequency is occupied by lesions of the pyramidal tract or conductive structures that regulate voluntary movements. These are various paralysis and paresis, decreased muscle strength and high fatigue with little physical activity. The lower extremities are affected more often. Upon examination, a sharp increase in tendon reflexes is revealed.
An experienced doctor can detect all the symptoms of multiple sclerosis “on the hammer”.
There is also spasticity, a different decrease in muscle strength on the same limbs, clonus or rapid rhythmic contractions of individual muscle groups, most often in the feet and hands, contractures or limitation of passive movements in the joint. The course of movement disorders is individual.
Coordination disorders are manifested by imbalance of the body, overshooting, trembling of the limbs when approaching the target, chanted speech. Dizziness occurs, handwriting changes, and unsteadiness appears when walking.
Oculomotor and visual disturbances are manifested by double vision, strabismus, chaotic movements of the eyeballs, drooping eyelids, changes in the reaction of the pupil to light, decreased visual acuity, narrowing of its fields, and blanching of the optic nerve head.
Lesions of other cranial nerves may manifest as smoothing of the nasolabial folds, drooping of the corner of the mouth, sensory disturbances in the face, drooling, hearing loss, difficulty swallowing, and a nasal tone in the voice.
Pelvic disorders in men are manifested by the classic triad described by Sheinberg. These are urinary incontinence, impotence and constipation. Fortunately, these violations occur only in 5% of cases.
Mental disorders include decreased memory and attention, pathological changes in mood, anxiety and obsessions. In some unfavorable cases, intellectual decline reaches the level of dementia.