Introduction
Fainting —also known as syncope —is the medical term for temporary loss of consciousness. Any episode of syncope is important for at least two reasons. First , fainting can cause injury, so it's important to try to prevent it from happening again. And secondly , fainting can sometimes be a sign of a serious medical problem. Although there are different types of syncope and the causes that lead to it, the most common type of syncope is vasovagal syncope.
What is vasovagal syncope?
Vasovagal syncope (also called neurocardiogenic syncope) is a temporary loss of consciousness caused by a neurological reflex that causes either a sudden dilation of the blood vessels in the legs, a very slow heart rate (bradycardia), or both.
Vasovagal syncope accounts for more than half of all syncope. While doctors often call it "simple syncope," the mechanism of vasovagal syncope is actually not that simple. And misunderstandings about how vasovagal syncope works can lead to problems making the correct diagnosis or choosing appropriate treatment.
Symptoms associated with loss of consciousness
Vasovagal syncope develops in two stages. The initial one is characterized by complex symptoms with a gradual loss of sensitivity.
Symptoms of fainting...
First stage:
- Intense pallor.
- Profuse cold sweating.
- Fatigue and loss of strength, which begins in the hands, then spreads to the whole body.
- Dizziness.
- Noise in ears.
- Gastrointestinal disorders.
- Pain in the chest, in the sternum area.
- Feeling of rapid heartbeat.
- Changes in field of view. Tunnel vision - only objects in front are visible.
- Abnormal perception of hot and/or cold.
This complex symptomatology is usually accompanied by loss of consciousness . However, in some cases, the described clinical picture occurs without fainting. Currently, this condition is commonly called presyncope.
Causes and triggers of vasovagal syncope
Vasovagal syncope occurs when something triggers the vasovagal reflex, causing the blood vessels to suddenly dilate. The dilation of blood vessels causes a significant portion of the blood volume to accumulate in the legs.
This association is often accompanied by a slowing of the heart rate. As a result, blood pressure suddenly drops. If the drop in pressure is enough to deprive the brain of oxygen, fainting occurs.
In most people with vasovagal syncope, dilation of the blood vessels is the predominant factor causing loss of consciousness. However, in some people, slowing the heart rate plays an important role.
Common triggers for vasovagal syncope include:
- sudden, severe pain;
- blood donation;
- traumatic event;
- extremely difficulty urinating or defecating;
- attack of prolonged and severe cough;
- hyperventilation;
- standing still for a long time (for example, if you sit for a long time);
- overwork in hot weather;
- excessive use of alcohol or substances (such as pills).
If an episode of syncope follows any of these events, vasovagal syncope is almost certainly occurring.
Symptoms and signs
Although the loss of consciousness in vasovagal syncope can be quite sudden, it is more typical that it is preceded by several seconds or several minutes of warning symptoms. These symptoms are sometimes called the “prodrome” (precursor) of fainting. Those that occur after you wake up from blacking out are called “postdromal.”
Prodromal symptoms
Prodromal symptoms of syncope often include:
- dizziness;
- buzzing or ringing in the ears;
- visual disturbances such as flickering or tunnel vision;
- sudden sweating;
- sudden nausea.
These prodromal symptoms are accompanied by a feeling of "weakness" and then, finally, loss of consciousness. The time between the onset of prodromal symptoms and actual syncope may be several minutes or one or two seconds.
If you feel yourself fainting, you can break the episode by lying with your legs elevated or sitting in a chair with your head between your knees. Wait until you feel better before you try to stand up.
Features of fainting
Fainting itself also has several characteristic features:
- Vasovagal syncope almost always occurs when the victim is standing or sitting upright (when blood may pool in the legs), and almost never occurs while lying down.
- People who experience vasovagal syncope usually regain consciousness within seconds of falling to the ground. This is because once on the ground, gravity no longer causes blood to pool in the legs and blood pressure improves almost instantly.
- On the other hand, if the victim is held upright by a benevolent bystander, the unconscious state can become very prolonged. This is a potentially dangerous situation because while the victim is upright and unconscious, the brain is not sufficiently perfused with blood.
If you see someone weak, place them on their back and raise their legs about 12 inches above their heart. Loosen any belt, collar or constricting clothing. Seek help if the condition lasts longer than a few seconds.
Postdromal symptoms
After an episode of vasovagal syncope, many people feel terrible for a few hours or even for the next few days or even longer. During this "postdrome" period, people typically experience extreme fatigue, nausea, dizziness, and loss of appetite.
Prevention measures
In order to prevent vasovagal fainting, first of all, it is necessary to avoid psycho-emotional stress. In particular, these include both conflict situations that can cause stress and prolonged stay in an upright position. At the same time, active outdoor activities are used as preventive measures to prevent loss of consciousness: walking, running, and so on.
You can also prevent the onset of another fainting spell:
- hardening or contrast shower (strengthens blood vessels);
- adherence to daily routine;
- duration is at least 8 hours;
- Regular consumption of herbal tea, red wine or coffee to restore blood pressure;
- drinking chamomile, lemon balm or St. John's wort tea, which has a positive effect on the nervous system.
Vasovagal syncope is not a dangerous phenomenon, which, however, may indicate serious pathologies: cardiovascular diseases, tumors. You can cope with such phenomena if you change your lifestyle.
Diagnostics
Doctors who know how to correctly diagnose vasovagal syncope understand that this condition is almost always situational. Vasovagal syncope is especially likely after a viral illness, after exercise, after a warm shower, or early in the morning—in other words, relative dehydration can occur at any time.
Given these characteristic features and the situational nature of this condition, doctors should be able to make a correct diagnosis simply by looking at symptoms, medical history, family history, and the sequence of events leading to syncope.
Physical examination of people with vasovagal syncope is usually completely normal. However, testing (such as an ECG) is very useful in diagnosing the similar conditions of orthostatic hypotension or postural orthostatic tachycardia syndrome (POTS) and can be very helpful in screening for likely candidates.
Causes
Vasovagal syncope occurs for the following reasons:
- Disruption of the autonomic nervous system, leading to improper regulation of vascular contractility, is the cause of neurogenic fainting (accounting for more than 50% of all fainting);
- Heart pathology is the cause of cardiogenic diseases (account for 25% of all);
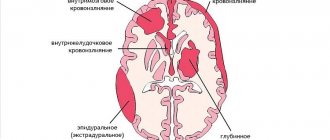
- Vascular disorders (significant atherosclerotic deposits in the vessels of the head and neck, transient ischemic attacks, strokes);
- Sudden increase in intracranial pressure (tumor, hydrocephalus, hemorrhage);
- Decrease in the content of oxygen, sugar, electrolytes in the blood (hypoxia, anemia, hypoglycemia, renal and liver failure);
- Decreased circulating blood volume (bleeding, excessive urination, diarrhea);
- Poisoning (carbon monoxide, alcohol, etc.);
- Mental disorders (hyperventilation syndrome, hysterical neurosis).
After physical activity
- There are situations where vasovagal syncope occurs after exercise. In this case, the provoking factors are: a tight collar, a sharp turn of the head, strong compression of the chest, pressure on the area of the carotid sinus.
- Vasovagal syncope occurs in athletes in this way: a sudden reflex expansion of peripheral vessels occurs, as a result of which cardiac output sharply decreases and cerebral hypoxia develops; There is a sudden reflex suppression of cardiac activity by the vagus nerve until the heart stops completely.
- In the first case, ordinary fainting occurs, and in the second, blood circulation suddenly stops, which requires immediate medical attention.
Causes during pregnancy
During pregnancy, a woman’s general condition is often characterized by increased weakness and general malaise. This is caused by processes and stress on the body. But sometimes expectant mothers experience dizziness followed by fainting. As a result, the pregnant woman begins to worry a lot.
It is necessary to understand the reasons for this phenomenon, and most often they are associated with:
- a sharp change in blood circulation;
- low sugar levels in the body;
- sudden movements;
- frequent and long periods of lying on your back;
- stuffiness and heat;
- toxicosis.
Treatment of vasovagal syncope
People who have had a single episode of vasovagal syncope do not need any medical treatment at all.
But if there have been recurring episodes, there will likely be more episodes if the person is not treated. And, as anyone with vasovagal syncope knows, these episodes of fainting often come at the most inconvenient or impractical times and can be very life-disrupting. Fortunately, treatment is usually quite helpful.
There are several main types of treatment for vasovagal syncope: medications, exercise, and a pacemaker.
Medications
In some people, vasovagal syncope occurs with alarming frequency, even when all appropriate precautions are taken. For these people, drug therapy is often helpful.
In the past, the drugs most commonly used for vasovagal syncope were beta blockers, but some studies have not shown any benefit and these drugs are not currently recommended.
Drugs that have been shown to have some effectiveness include:
- Midodrine, a vasoconstrictor that dilates blood vessels;
- Disopyramide, an antiarrhythmic drug;
- Serotonin reuptake inhibitors;
- Theophylline, commonly used to treat asthma.
Therapeutic measures
The treatment regimen for vasovagal syncope is determined based on the severity of the underlying disease. Therapeutic intervention is mainly used for patients who often experience short-term loss of consciousness.
In cases where the problem under consideration arises due to mental pathologies, the treatment regimen is determined depending on the status of the underlying disease.
Therapy for vasovagal syncope consists of several approaches.
Drug treatment
The patient is prescribed the following medications:
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
- Alpha adrenergic agonists. They contribute to the narrowing of blood vessels.
- Beta blockers. Such drugs block specific receptors in the body that are activated under the influence of stress hormones (adrenaline and norepinephrine).
- M-anticholinergics. Prescribed for the treatment of bradycardia.
Surgical intervention
Used in the presence of heart diseases and tumors. Surgical intervention, during which, if appropriate indications are available, a pacemaker is introduced, is carried out subject to the following conditions:
- age exceeds 40 years;
- vasovagal syncope occurs with regular frequency;
- absence of initial symptoms indicating imminent loss of consciousness;
- arrest was recorded .
Lifestyle change
You can prevent another loss of consciousness by following these recommendations:
- drink at least two liters of liquid per day;
- exclude heavy physical activity;
- avoid emotional stress;
- sleep at least eight hours a day;
- stop wearing tight underwear, replacing them with compression ones;
- regularly perform exercises aimed at strengthening your mental state.
Special isometric exercises are also used, through which you can increase blood pressure for a short period of time:
- Holding the ball in your hand, you need to squeeze your palm. The action promotes the outflow of venous blood.
- Hands clasp together and then forcefully pull in opposite directions.
- In a standing position, the legs are crossed, after which they must be tensed.
In case of sudden loss of consciousness, the person must be placed on his back with his legs raised above his head. This pose increases blood flow to the brain.
Vasovagal syncope is not dangerous to humans. It causes only two types of complications:
- injuries resulting from a fall;
- deterioration in quality of life in cases where fainting occurs frequently.
Preventive measures can help prevent another loss of consciousness.