Our clinic specializes in the treatment of autoimmune diseases. Pregnancy with multiple sclerosis (MS) poses some risks, but these can be minimized. Our most positive experience to date is our patient, who carried and gave birth to three healthy children without increasing neurological deficit. If you are determined to plan or maintain an existing pregnancy, we will be happy to help you.
Pregnancy management programs.
- Preparing for pregnancy with multiple sclerosis
- Management of pregnancy in multiple sclerosis
- If pregnancy with multiple sclerosis occurs without preparation
- Management of the postpartum period
How can multiple sclerosis be treated safely for a child ? Usually, as a basic drug, we use immunoglobulins for intravenous administration. It is possible to use other safe agents of biological origin (peptides, etc.).
Preparing for pregnancy, if you have time for it. The use of medications during pregnancy is limited. Therefore, our task is to solve all problems as much as possible before pregnancy. First of all, we are talking about the treatment of infections, correction of intestinal flora, normalization of night sleep, i.e. about preventing everything that can provoke an exacerbation.
Our clinic employs obstetricians and gynecologists with experience in managing pregnancy with autoimmune diseases. If necessary, a neurologist-immunologist comes to the rescue. Our task is to minimize the risk, and if it worsens, to immediately stop the exacerbation.
If you decide to plan or maintain an existing pregnancy, we will be happy to help you. Who to contact in our clinic:
- You can choose and purchase a pregnancy management program.
- In addition to the pregnancy management program, we recommend consulting a neurologist or neurologist-immunologist. At this consultation, the doctor will outline a plan of action and joint (obstetrician-gynecologist + neurologist) management of pregnancy.
Is it possible to get pregnant with MS?
Doctors say that, like other autoimmune pathologies, bearing a child has a beneficial effect on the course of the disease. During the gestational period, natural immunosuppression occurs. This results in a decrease or complete absence of symptoms of multiple sclerosis throughout pregnancy.
It turns out that bearing a child is not a contraindication for a sick woman. On the contrary, at this time an exacerbation of multiple sclerosis is observed only in 5-10% of expectant mothers.
Doctors say that the disease is easier and less likely to lead to disability in women who have given birth. If you have multiple sclerosis, you cannot get pregnant and give birth only if the disease is severe . With it, the patient is unable to move independently and is practically bedridden.
Is IVF allowed?
In patients with multiple sclerosis, in vitro fertilization increases the risk of exacerbation of the disease:
- by 70% over the next two months;
- by 60% – three months.
This is due to the use of synthetic gonadotropin during the procedure . This drug stimulates superovulation (maturation of several follicles).
It is noted that women who underwent IVF in the remission stage of MS, but the attempt ended in failure, are at risk of relapse.
According to the observations of French scientists, 49 out of 70 in vitro fertilization cycles were unsuccessful.
Symptoms
Manifestations of multiple sclerosis are associated with damage to various parts of the brain and spinal cord. Areas of demyelination of nerve fibers can occur in a variety of places. Depending on the location of the pathological process, one or more symptoms may develop:
- inconsistency of movement of different muscle groups;
- tremor;
- strengthening reflexes;
- muscle weakness (usually lower extremities);
- paralysis and paresis;
- slurred speech;
- dizziness;
- strabismus;
- nystagmus;
- decreased sensitivity of the skin;
- numbness, tingling or burning of fingers and toes;
- difficulty swallowing;
- spontaneous urination and defecation, stool and urine retention;
- decreased intelligence;
- behavior change.
With multiple sclerosis, neurosis-like conditions often develop. Some women experience asthenovegetative syndrome (weakness, apathy, fatigue). Depression or euphoria may develop. Hysterical states associated both with organic changes in the brain and with the individual mental reaction to the diagnosis are very typical. 80% of all women experience sudden mood swings throughout the day.
There are several variants of the course of the disease:
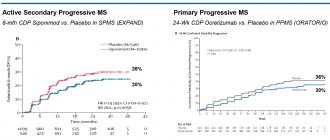
- Remitting-relapsing . The most common clinical variant. Periods of exacerbation are followed by moments of complete remission with the absence of any symptoms. The woman’s condition does not worsen from attack to attack.
- Primary progressive . From the first days of the disease, there is a continuous increase in neurological symptoms and a deterioration in the woman’s condition. Periods of remission are not typical.
- Secondary progressive . Occurs 5-10 years after the onset of the disease. Periods of remission disappear, the disease passes into a progressive form with a gradual deterioration of the general condition and an increase in negative symptoms.
The course of the disease is individual for each woman. No two patients are alike, with identical symptoms or the same rate of disease progression. It is almost impossible to predict in advance the rate of development of multiple sclerosis.
What steps should you take when planning?
To accurately determine whether a woman can give birth, she should consult a neurologist. The doctor will refer the patient for a consultation with an ophthalmologist and prescribe a number of additional examinations.
Survey results:
- The ophthalmologist will check your vision and look at the condition of the fundus.
With multiple sclerosis, one eye is usually affected. Symptoms of retrobulbar neuritis appear. In addition, the doctor performs perimetry with various shades. With the disease, the patient suffers from a narrowing of her visual fields and impaired color perception. - MRI is the most effective diagnostic method for identifying lesions in the brain and spinal cord in MS.
In the image, the doctor reveals multiple small lesions that look like areas of clearing. Magnetic resonance imaging is a safe and informative method. It does not harm the health of the expectant mother.
If a woman's health condition allows her to become pregnant, her doctor may stop certain medications because they may harm the developing fetus . Usually, the doctor advises you to stop taking DMTRS 3 months before the planned gestation.
If the patient experiences an exacerbation of multiple sclerosis for the first time, she will have to refrain from conceiving for some time. With a progressive course, pregnancy is undesirable, since treatment is necessary.
Multiple sclerosis, pregnancy and childbirth
Multiple sclerosis (MS) is a fairly widespread dysimmune disease of the central nervous system, which affects mainly young people and almost inevitably leads, at a certain stage of its development, to disability. This disease is chronic, in most cases progressive, unpredictable in course and currently incurable. In recent years, there has been an increase in MS incidence rates, which is associated not only with improvements in diagnostic methods, but also with an absolute increase in the number of cases. The age range of this disease is also expanding (usually 20–40, but cases of onset of the disease at the age of 10 to 55 years have been described). The exclusion of a large number of able-bodied people from active life due to disability, high costs for diagnosis, treatment, rehabilitation and social assistance make the problem of MS socially and economically significant.
The significant and uneven prevalence of the disease on Earth is noteworthy. High-risk areas for MS incidence (more than 100 patients per 100,000 inhabitants) are the Scandinavian countries and Central European countries, Canada. In Russia, southern European countries, Australia and the USA, this disease occurs with a frequency of 30 to 100 cases per 100,000 inhabitants. Women get sick more often than men, representatives of the white race more often than blacks.
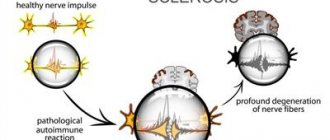
The study of MS dates back more than 100 years, and although significant strides have been made in understanding the disease in recent years, many unresolved questions remain. In recent years, the understanding of the very essence of MS has changed as a disease that affects only the myelin sheaths of the conductors of the brain and spinal cord, in which periods of exacerbations are replaced by periods of complete or almost complete clinical well-being. It is now known that already in the early stages of the disease there is damage to the axons themselves, leading to brain atrophy, and therefore it is proposed to consider MS as an autoimmune neurodegenerative, and not just a demyelinating disease. It has been reliably proven that even in the phase of complete clinical remission, the activity of the disease remains, and this is confirmed by the appearance of new foci of demyelination (according to magnetic resonance imaging) and ongoing disorders in the immune system. Thus, MS is not in the full sense of the word a “remitting” disease.
Until recently, the timing of establishing the correct diagnosis of MS in the development of neurological symptoms was not particularly important, since the doctor could not influence the development of the disease to any extent. Treatment of patients consisted only of stopping exacerbations and providing symptomatic therapy. In recent years, the situation has changed radically due to the advent of so-called preventive, or modifying, therapy. These drugs, although they are not able to cure the patient, significantly change the course of MS in many patients, preventing the development of exacerbations and slowing down the development of disability. The activity of research devoted to the morphology, etiology and pathogenesis of MS, and, as a consequence, the development of new therapeutic approaches to its treatment, gives reason to believe that in the not too distant future it will be possible to find methods for secondary clinical prevention and pathogenetic radical treatment of MS.
Multiple sclerosis and pregnancy:
It has long been well known that pregnancy has a beneficial effect on the course of MS—during it, exacerbations of the disease become less frequent.
The reason for this is considered to be hormonal changes during pregnancy, which is accompanied by immunosuppression. However, in the first 3 months. after childbirth, on the contrary, the disease may take on a more aggressive course - exacerbations become more frequent and more severe. This is why women with MS were previously strongly discouraged from having children. Recently, this view has been revised. Long-term observation over a number of years of a large number of sick women before pregnancy and after childbirth turned out that, although in the first months after childbirth the frequency of exacerbations does increase somewhat (the risk of exacerbation in the first 3–6 months after childbirth is 20– 40%), balancing their decrease in the prenatal period, the birth of a child does not affect the long-term prognosis of the disease. Moreover, one study over a 25-year period showed that women who had children during this period later experienced secondary disease progression (compared to nulliparous patients) and were less disabled.
Thus, it was found that pregnancy and childbirth are not a risk factor for exacerbations of MS, and it is even possible that pregnancy has a beneficial effect on the course of the disease. Exacerbations that occur in the first months after childbirth are probably provoked not by hormonal changes, as previously thought, but by the stress of childbirth and significantly increased physical activity after the birth of a child. Women should not be scared of pregnancy. A more significant activation of the disease than childbirth is caused by termination of pregnancy (both artificial and spontaneous) and hysterectomy.
During pregnancy, drug treatment should be avoided if possible. The use of adrenocorticotropic hormone and its synthetic analogs is contraindicated, since these drugs suppress the adrenal glands of the fetus. In case of severe exacerbation in the second and third trimester of pregnancy, the use of prednisolone is allowed.
There are descriptions of the use, even in the early stages of pregnancy, of hormonal “pulse therapy” with methylprednisolone, plasmapheresis and intravenous immunoglobulin to relieve severe exacerbations, with the subsequent birth of healthy children.
During pregnancy and breastfeeding, you should not take drugs that can pass through the placenta or through mother's milk into the baby's body. Such drugs, often used for MS, include: diphenine, carbamazepine, baclofen, azathioprine, cyclophosphamide.
If pregnancy occurs in a patient with MS receiving preventive therapy with beta-interferons or Copaxone, such treatment should be discontinued until the baby is born and breastfeeding is complete. However, there are isolated observations that describe cases of continued treatment with preventive therapy drugs during pregnancy. In all cases, healthy children were born, and monitoring them until the age of 3 did not reveal any deviations from the norm. And yet, during pregnancy and lactation, treatment with modifying drugs should not be continued. After completing the breastfeeding period, it is advisable to start or resume preventive therapy as soon as possible in order to avoid a possible exacerbation. If the patient received mitoxantrone, then a break of 6 months is desirable. before pregnancy (although there is evidence of the birth of healthy children in women who received mitoxantrone at the time of conception).
During pregnancy, a woman should not take benzodiazepines, as they act on the fetus, leading to the development of “floppy baby” syndrome.
The recommended drug for the development of urinary infection during pregnancy is ampicillin. For those patients who have already had episodes of urinary tract infections, its prophylactic use is indicated, since the development of pyelonephritis is very likely.
Methods of delivery for multiple sclerosis:
Depending on the duration of the disease and the existing neurological disorders, childbirth in MS is carried out either naturally or surgically. In general, pregnant women with MS undergo operative delivery approximately 1.5 times more often than other pregnant women.
Childbirth anesthesia in pregnant women with MS:
In standard situations, a cesarean section is performed under one of the types of neuraxial anesthesia (spinal or epidural anesthesia). Previously, it was believed that multiple sclerosis is a contraindication to surgery under neuraxial anesthesia, since it involves the administration of drugs (local anesthetics) directly into the spinal cord, which is part of the nervous system. However, studies in recent years have shown that patients with multiple sclerosis tolerate all types of anesthesia and anesthesia equally well. It has been proven that patients with multiple sclerosis have the same risk of anesthesia complications as relatively healthy people.
When it comes to vaginal birth, research clearly demonstrates that epidural pain relief for labor does not increase the risk of an MS attack in the postpartum period. That is, in pregnant women with multiple sclerosis, epidural anesthesia can quite reasonably be used to relieve pain during natural childbirth, especially since severe pain, which is a constant companion to childbirth, is a proven risk factor for exacerbation of the disease.
In standard situations, a cesarean section is performed under one of the types of neuraxial anesthesia (spinal or epidural anesthesia). Previously, it was believed that MS is a contraindication to surgery under neuraxial anesthesia, since its implementation involves the administration of drugs (local anesthetics) directly into the spinal cord, which is part of the nervous system. However, studies in recent years have shown that patients with MS tolerate all types of anesthesia and anesthesia equally well. It has been proven that patients with MS have the same risk of anesthesia complications as relatively healthy people.
Thus, depending on their health status, pregnant women with MS can equally safely give birth either independently or through a caesarean section. Vaginal childbirth in patients with multiple sclerosis is best performed under epidural anesthesia. The choice of anesthesia for caesarean section is based on generally accepted principles and does not have any fundamental features.
Protective effect of breastfeeding in MS:
Researchers from Stanford University, led by Dr. Annst Langer-Gould, found that breastfeeding delays the exacerbation of MS after pregnancy. Typically, women with MS go into remission during pregnancy, but suffer an unusually high rate of disease exacerbations for 3–4 months. after childbirth.
In the group of women studied, 48% breastfed only for at least 2 months, and 52% did not breastfeed at all or breastfed and began supplementing in the first 2 months. after childbirth. Among women who mixed breastfeeding, the percentage of exacerbations of MS was 87%, while among women who exclusively breastfed for 2 months. exacerbation occurred in only 36%. Interestingly, 60% of women with MS chose not to breastfeed or mixed feed before starting MS medications. It was in this group that started taking medications in the first 2 months. after childbirth, there was the highest % of exacerbations. Researchers suggest that exclusive breastfeeding delays the resumption of ovulation. Lactational amenorrhea can have an anti-inflammatory effect on the body.
Literature:
- T. E. Schmidt, N. N. Yakhno “Multiple sclerosis” // Moscow “Medicine”, 2003, pp. 7–8, 79,138–139;
- A. S. Nikiforov, E. I. Gusev “Private neurology” // Moscow “GEOTAR-Media”, 2008, P. 245;-
- Maurice Victor, Allan H. Ropper, seventh edition of the “Manual of Neurology” // MIA, 2006, P 413;
- Science Daily, 2009, research;
- Article “The whole truth about anesthesia”, 2015.
Exacerbation of the disease in the first trimester
It is noted that in 3–10% of cases, relapse of multiple sclerosis is mild and short-lived. When remission occurs, the condition is completely restored to its original state.
The risk of exacerbations directly depends on the frequency of outbreaks of the disease before pregnancy. If they were frequent, the threat of relapse increases.
Causes
During the gestational period, the hormonal background of the expectant mother undergoes changes . This entails a decrease in the activity of autoimmune reactions.
For a pregnant woman, the fetus is an allogeneic transplant (foreign), since it carries paternal antigens.
Despite the fact that during pregnancy, T1-type immunity is suppressed, T2-type reactions are activated. They are necessary for the passive transport of antibodies from mother to fetus.
Danger and consequences
According to the observations of specialists, the risk of spontaneous miscarriage and non-developing pregnancy is the same as in healthy women.
Many expectant mothers worry that the disease will be passed on to their children. However, this occurs only in 5% of cases. In 10% of cases, the disease is inherited when both parents have multiple sclerosis.
What treatment is prescribed?
If pregnancy is planned, then 3 months before it and during the entire gestational period, immunomodulators, Bac-lofen, Sirdalut, Finlepsin are discontinued.
They have a teratogenic effect and can lead to impaired fetal development.
During exacerbations, the doctor may prescribe short courses of glucocorticoids - Methylprednisolone. Its use is safe in the 2nd and 3rd trimesters. In the early stages, the medicine is used only for health reasons, since during this period it can disrupt the intrauterine development of the child.
The doctor prescribes pulse therapy because it is not accompanied by the appearance of intrauterine defects in the fetus. It is believed that immunoglobulin therapy is safe at any stage of gestation.
What you need to know about multiple sclerosis:
- how the disease begins, what are the early symptoms and signs;
- what are the causes and possible consequences of the disease;
- what diseases are similar to MS;
- what types and forms of the disease exist.
Breastfeeding
Multiple sclerosis and pregnancy are an opportunity to forget about exacerbations for a while, since during pregnancy the immune system suppresses the manifestations of the disease. However, after childbirth, the risk of exacerbations not only returns, but also increases slightly. This is associated with the occurrence of chronic stress: the expectant mother does not get enough sleep, worries about the child and tries to breastfeed the child for some time, which is a contraindication to taking medications. Prolactin continues to be produced during breastfeeding, but doctors still recommend switching to artificial formula when the baby is two to three months old. After this, the expectant mother can resume taking medications.
Is it worth giving birth with this diagnosis?
Spontaneous delivery is not considered a contraindication for multiple sclerosis . Doctors say that it occurs in expectant mothers without serious complications.
During childbirth, an expectant mother with MS is more tired than a healthy woman. That's why doctors should help her give birth faster. The patient must push correctly and not miss a single contraction during pushing.
Caesarean section is prescribed for patients with MS for medical reasons (for irreversible changes in the nerve fibers responsible for expulsion of the fetus from the uterus). It takes place under epidural anesthesia, which is absolutely safe for the baby.
Possible complications after childbirth
Doctors say that exacerbations of multiple sclerosis occur soon after the birth of a child . Most often they occur in the first 3 months after birth.
At this time, hormonal levels return to their original levels. The immune system is activated. The myelin sheath of nerve fibers is severely damaged. Attacks become more severe than before the gestational period.
Treatment of the disease if the child is on breastfeeding
For patients with multiple sclerosis, lactation is recommended for up to 3 months, less often up to six months . In order not to provoke new attacks, mothers are prescribed PMTRS, and the baby is transferred to artificial feeding.
Women with MS should remember that prolonged breastfeeding does not prevent relapse rates. This is why it is necessary to include medications.
Modern doctors do not prohibit patients with multiple sclerosis from becoming pregnant and giving birth . On the contrary, they advise them to conceive a child so that their body can rest during the gestational period. During pregnancy, the disease stops. If there are no medical indications, childbirth takes place naturally.
MS Treatment Methods
At the moment, there are no drugs that can completely cure multiple sclerosis. But the disease is progressive. Periods of exacerbation constantly alternate with periods of remission. Only adequate treatment can significantly prolong remission. Therapy is aimed at reducing inflammation and relieving symptoms.
Patients are recommended to have a healthy lifestyle. Regular physical activity is very important, aerobic exercise is especially beneficial. It is necessary to maintain optimal levels of vitamins and minerals, avoid overexertion (nervous tension is especially dangerous) and take proper rest, control body temperature, practice relaxing practices (meditation, yoga) and physiotherapeutic procedures (swimming, massages).
How is childbirth?
When a girl is pregnant, with multiple sclerosis, childbirth takes place only in a hospital under the supervision of specialists, since complications with such diagnoses are not included in the list of possible exceptions. The woman in labor will have to warn the obstetricians about her illness.
The procedure of epidural anesthesia during childbirth is becoming increasingly popular. Is this dangerous? An unambiguous answer will be difficult, since in all examples the decision is made by a specialist.
Epidural anesthesia is considered an alternative to spinal anesthesia; it differs in its mechanism of action. The anesthesia administered in this way affects the roots of the spinal cord and bypasses its trunk. The likelihood of exposure to toxins is reduced.
When there is a loss of sensation, the woman in labor will have to miss contractions, in which case labor will be induced artificially. Cesarean section is often a common delivery option for multiple sclerosis , since natural childbirth can be dangerous.
General information about RS
The development of multiple sclerosis in the human body can be viewed by comparing it to an electrical wiring system. Nerve endings have “insulation” similar to electrical wires. Wire insulation is a combination of plastic and rubber. Nerve insulation is myelin, which separates nerve fibers from each other and facilitates the smooth passage of impulses to a specific target. A compromised immune system simply begins to “devour” myelin, leaving nerve endings without insulation. This leads to the fact that the signal transmitted along the nerve endings weakens or simply does not reach the target.
Multiple sclerosis most often occurs in young people aged 15 to 25 years, less often from 25 to 45 years, very rarely after fifty. There are three times more women suffering from it than men.
Statistics show that in each individual country, per hundred thousand people, the number of patients will be different: in Russia - 40, in Holland - 128, and in Norway - 180.
A person suffering from multiple sclerosis experiences symptoms that interfere with normal life. These are various vision problems, impaired coordination of movements, memory and speech disorders. The patient feels constant fatigue and weakness throughout the body and, first of all, in the limbs. In the early stages of the disease, the symptoms are mild - this makes it difficult to diagnose the body and, accordingly, make a diagnosis. If you do not pay attention to minor symptoms, a person can live for several years with the disease without even knowing that he is sick.
Possible complications of pregnancy
Doctors do not recommend artificial termination of pregnancy due to hormonal stress, which can significantly accelerate the activation of the disease compared to the situation when pregnancy ends naturally - childbirth. Possible complications:
- Spontaneous termination of pregnancy.
- Insufficient body weight of the newborn.
- Congenital malformations in a newborn.
Complications occur with a frequency characteristic of the general population of pregnant women. Clinical practice confirms that the diagnosis of MS is not a provoking factor for premature birth. There is also no direct connection between a parental diagnosis of MS and child mortality or congenital malformations.