Classification of Wilson's disease
Soviet neurologist N.V. Konovalov, who studied the pathophysiology, pathogenesis, and clinical picture of this disease, classified the disease, identifying five of its forms:
- Abdominal: when the liver is affected, which leads to the death of the patient before symptoms appear, diagnosed in childhood, duration up to five years.
- Rigid-arrhythmohyperkinetic - a rapidly progressive form, observed in childhood, characterized by muscle rigidity, slowness of movements, the formation of contractures, convulsive laughter and crying are observed, and there is a delay in development.
- Trembling: observed in adulthood (20-30 years), progresses slowly (about 10 years), characterized by trembling. At the last stage, rigidity appears, anemia, sluggishness and monotony of speech, severe mental degradation, and epileptic seizures are observed.
- Trembling-rigid is the most common form, observed in adolescence, severe rigidity and severe trembling develop, symptoms worsen with excitement or physical muscle tension, accompanied by dysphagia and dysarthria, progressing for about six years.
- Extrapyramidal-cortical - rare, aggravated by pyramidal paresis, epileptic seizures and severe dementia due to severe softening of the cerebral hemispheres.
Etiology and pathogenesis of Wilson's disease
An excess of copper leads to severe intoxication of the body - oxidation of cell membranes, destabilization of nuclear DNA. More than two hundred modifications of the mutating gene have been identified.
The pathogenesis of Wilson-Konovalov disease is a violation of the entry of copper into the body and its excretion. Disturbances in the process of normal excretion of copper from the body are associated with a lack of P-type protein. There are also disturbances in the composition of ceruloplasmin, which is synthesized in the liver and includes copper. Toxification of the body due to an excess of copper is reflected primarily in the liver, where copper accumulates in especially large quantities, damaging the organ.
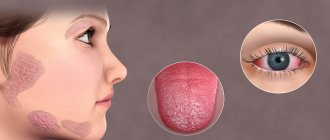
The next place where copper accumulates is the central nervous system. The basal ganglia of the brain suffer the most, causing severe neuropsychiatric disorders. Copper deposits are also visible in the cornea of the eye - the so-called Kayser-Fleischer ring. Copper also affects the heart and joints.
Hepatolenticular degeneration (Westphal-Wilson-Konovalov disease)
Diagnostic features:
Screening for Westphal-Wilson-Konovalov disease should be carried out in patients aged 3 to 40 years with an unexplained increase in aminotransferases, manifestations of FPN, HCG, liver cirrhosis, neurological changes of unknown etiology, behavioral disturbances, motor coordination, mental symptoms, corneal rings Kaiser-Fleischer, Coombs-negative hemolytic anemia, family history of Westphal-Wilson-Konovalov disease. In the diagnosis of the disease, an important place is given to the typical clinical picture in the form of damage to the liver and nervous system, identifying the familial nature of the disease, and the appearance of Kayser-Fleischer rings on the cornea. Among the laboratory data, noteworthy is the decrease or absence of ceruloplasmin activity in the blood serum, an increase in the content of copper not associated with ceruloplasmin in the blood serum (300 μg/l or more), an increase in the copper content in organs, in particular in liver tissue, an increase copper excretion in urine (more than 200 mcg/day). Therefore, the combination of such manifestations as anemia, severe jaundice and relatively low aminotransferase activity should be alarming regarding the acute course of the disease.
In morphological examination of the liver, specific changes are uncharacteristic. At the same time, in acute hepatitis, swelling of hepatocytes, isolated necrosis, and lymphocytic infiltration are more often observed. tradition. In patients with chronic hepatitis, balloon and fatty degeneration and necrosis of hepatocytes, lymphoid inflammatory infiltration, fibrosis of portal tracts, vacuolization of hepatocyte nuclei are determined in the liver. Fulminant liver failure is morphologically manifested by small-scale obesity and coagulative necrosis of hepatocytes, the presence of Mallory bodies, hypertrophy of Kupffer cells containing a large amount of pigment. As a diagnostic method, the determination of copper in liver tissue is used (the normal copper content in the liver is 15-55 μg/g of dry liver). In recent years, liver uptake of radioactive copper and genetic testing have been used for diagnosis. The ratio of liver radioactivity 24 and 2 hours after intravenous administration of a radionuclide is normally 1.4-9.0, while in Westphal-Wilson-Konovalov disease this ratio is 0.2-0.3.
Our experience in managing hepatological patients shows that many patients suffering from chronic liver diseases of a “non-Wilsonian” nature also have impaired copper metabolism. However, in contrast to hepatolenticular degeneration, in this category of patients there is an excess content of this metal in the blood serum along with an increase in the level of serum ceruloplasmin. Impaired copper metabolism in chronic liver diseases (in the absence of a genetically determined metabolic defect) is included in the multifactorial mechanism of development of hepatocyte hypoxia due to the toxic effect of copper itself, disruption of the adaptive antioxidant system, immune disorders with the development of microcirculatory sinusoidal disorders. Copper, being a blocker of sulfhydryl groups, aggravates the imbalance of the antioxidant system, which promotes the activation of enzymes involved in the metabolism and synthesis of collagen, accelerating the processes of fibrogenesis. The instability of antioxidant protection parameters in combination with impaired hepatocyte metabolism against the background of altered copper metabolism contributes to the activation of the mononuclear phagocyte system, which leads to a number of severe immune and rheological disorders that contribute to the progression of the pathological process (see color insert).
Clinical picture of Wilson's disease
Wilson-Konovalov disease is divided into two stages:
- Latent (lasts about 6 years).
- Stage of clinical manifestations.
The disease manifests itself at the age of 7-15 years. Based on the symptoms of the disease, there are three forms:
- With liver damage.
- With damage to the nervous system.
- Mixed.
In children, the disease most often manifests itself as cirrhosis of the liver; cases of Wilson's disease are diagnosed after jaundice, anorexia, fever, and renal failure.
Mental disorders in patients are observed in adolescence, and mean that the liver is already oversaturated with copper and this trace element has begun to accumulate in the central nervous system. During this period, the patient experiences disturbances in facial expressions, coordination of movements, articulation and speech apparatus.
In some cases, symptoms of a neurological and mental disorder appear. Mental disorders are associated with various phobias, aggressive behavior, but with the preservation of intellectual abilities. Some patients have hematological syndromes.
Wilson's disease affects the skin (presence of pigment spots), bones become very fragile (increased risk of injury), joints (arthritis), and the endocrine system are affected.
MRI for Wilson-Konovalov disease
Manifestations of this pathology on MRI are detected due to an increase in the MR signal in the T2 mode and a decrease in the T1 mode from the subcortical region (fence, putamen, caudate nuclei, lateral globus pallidus, external capsule), midbrain, dentate nuclei of the cerebellum and vermis.
The first to be affected are the putamen and caudate nuclei. In the pons of the brain, damage to its median and dorsal sections is recognized with preservation of the pyramidal tracts and a similar change in the MR signal from these structures.
The sequential evolution of signal changes from the dorsal part of the bridge resembles a “baby panda face” with “eyes” that are formed by a pathological signal from the central tegmental pathways.
The damage to the midbrain is diffuse, but damage to the white matter predominates with preservation of nuclear structures, including the largest red globules. In the later stages of the disease, atrophic changes in the subcortical structures are detected.
The high quality of visualization of structural changes in the brain, which is provided by MRI, is very important for the correct diagnosis.
Thus, manifestations of the disease on MRI are considered pathognomonic (i.e., certainly characteristic), which makes it possible to differentiate Wilson-Konovalov disease from other neurological pathologies. Find out why you should choose our MRI center?
Diagnosis of Wilson's disease
Diagnosis begins with a visual examination of the patient and finding out the family history of the disease:
- analysis of changes in skin color (presence of pigmentation);
- the presence of a yellow-brown ring along the edge of the cornea of the eye;
- Palpation of the liver will indicate whether there are changes in the organ’s volume.
Laboratory tests follow:
- General and biochemical blood tests. Analysis of the amount of copper in the blood (in patients more than 1.5 thousand milligrams per liter), dosage of ceruloplasmin.
- Urine analysis for copper concentration.
- Liver biopsy.
A genetic examination is also carried out, which provides the most accurate information about the patient. After this, the attending physician makes a differential diagnosis.
General principles of treatment
Therapy of hepatocerebral dystrophy is based on two main points:
- the use of drugs with the active substance penicillamine, which bind excess copper and normalize its metabolic processes;
- strict adherence to diet No. 5 (exclusion of fatty, fried, spicy foods), as well as ingredients that contain large amounts of copper (legumes, nuts, chocolate, coffee).
Long-term (lifelong) use of these components (under the supervision of a doctor) makes it possible to achieve a reverse development of clinical signs and long-term remission of hepatocerebral dystrophy.
Treatment of Wilson's disease
Treatment of this disease is aimed at limiting the intake of copper into the patient’s body and reducing accumulated reserves.
For this purpose, various treatment methods are used:
- A non-drug method is changing the patient’s lifestyle (diet, giving up alcohol and hepatotoxic medications). Products with a high level of copper (meat, seafood, dried fruits, mushrooms, chocolate, some types of groceries, fruits) are excluded from the diet.
- Drug treatment. It starts from the moment of diagnosis until the end of the patient’s life. Continuity and quality of drug treatment is the key to increasing patient survival. Cuprenil (copper chelator) is the main drug in the treatment of Wilson's disease. When the dose of cuprenyl is increased, copper is excreted in the urine. There are certain doses and specifics of taking the drug, which are established based on an analysis of the patient’s condition and the course of his illness.
- Surgical treatment (transjugular intrarenal shunting).
Diagnostics
To begin with, doctors collect anamnesis and conduct an external examination. Based on the results, the degree of damage to the body is assessed, clinical recommendations are given, and the following tests are prescribed:
- Blood and urine. In order to determine the percentage of ceruloplasmin and copper content in the body.
- A slit-lamp examination by an ophthalmologist to detect the presence of a Kayser-Fleischer ring.
- Genetic tests of the patient and his relatives.
- Ultrasound of the abdominal organs.
- MRI of the brain.
- Liver biopsy.
Reference ! The listed simple and accessible diagnostic methods allow us to exclude other diseases that have similar symptoms. In addition, the examination will help you choose the correct supportive treatment.