A cerebral hemorrhage is the release of blood into the brain substance due to a ruptured vessel or through a highly permeable vascular wall. In the modern high-tech world, babies weighing even less than 0.5 kg are cared for, but this is a lot of work and these children may not always be like others. Cerebral hemorrhage can have an unfavorable outcome, leading to disability and death of the child - damage to the central nervous system ranks second in the structure of mortality of newborn children.
Brain hemorrhage often occurs in premature babies due to underdeveloped blood vessels and their fragility.
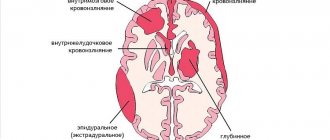
The following intracranial hemorrhages are distinguished:
- subdural;
- epidural;
- subarachnoid;
- peri- and intraventricular (near- and intraventricular);
- parenchymal;
- cerebellar.
In premature infants, subarachnoid, intra- and periventricular hemorrhages in the brain are more common.
Statistics
The exact frequency of occurrence of this pathology has not been established - in premature infants the clinical picture is nonspecific, making a diagnosis is difficult due to the low-symptomatic or even asymptomatic clinical picture. The doctors' limited clinical experience leaves its mark. Approximately: 80% of cases are children born at 32 weeks of development and earlier with a weight of less than 1500 g; but babies born at 34–35 weeks of intrauterine development occupy less than 2%. The incidence of cerebral hemorrhage in children weighing less than 1000 g is almost 50%. Boys are more susceptible to this pathology.
The lower the body weight of a premature newborn, the higher the risk of cerebral hemorrhage
The risk of vascular rupture decreases on the 4th day after birth and becomes insignificant after a week.
Diagnosis, treatment
Emergency doctors will inject the patient with a special drug that eliminates cerebral edema, try to block the hemorrhage so that the vessel stops bleeding, restore blood pressure and take him to intensive care. When dealing with a cerebral hemorrhage, it is very important that healthcare providers are experienced professionals.
Diagnostics
When the patient is taken to a medical facility, doctors will conduct a thorough diagnosis to accurately determine the location of the hemorrhage and its intensity. In this case, the patient remains in the intensive care unit even after taking all necessary measures, because... In the first weeks, observation is important to exclude complications and sudden deterioration in health with subsequent death.
The ICD code for intracranial hemorrhage is I61.
Doctors use several diagnostic methods in turn, trying to get the fastest possible research results. The following methods are used:
- Computed and magnetic resonance imaging (CT, MRI) - help determine the location of hemorrhage and the size of the hematoma, penetration of blood into the ventricles, displacement of parts of the brain, and the presence of vascular malformations;
- Echoencephalography - allows you to detect a blood clot and a displacement of the midline structures of the brain to the side distant from the hemorrhage;
- Angiography – shows the presence of aneurysm, vasculitis, neoplasms, and also displays areas without the presence of blood vessels;
- Lumbar puncture - helps determine the presence of blood cells in the cerebrospinal fluid;
- Ophthalmoscopy - determines the presence of signs of damage to the retina, the presence of blood in it, narrowing or displacement of veins.
After conducting all the necessary studies, the attending physician decides on further actions.
If a victim is brought to the hospital with complaints of mild symptoms reminiscent of an approaching or already occurring hemorrhage, the doctor should conduct a survey, check reflexes and prescribe an immediate ECG and other diagnostic methods. After this, a diagnosis is made.
It is important to carry out all checks within the first 6 hours after hemorrhage, otherwise the chance of saving life is significantly reduced.
Treatment
Immediately after receiving the research results, the doctor becomes clear exactly how to proceed. It all depends on the degree of hemorrhage and the presence of any complications. In special cases, emergency surgery may be prescribed.
Surgical intervention
Surgical intervention is required in cases where the patient has large hemispheric hematomas, blood has entered the ventricles of the brain, or an aneurysm has ruptured due to increased intracranial pressure. The operation must be performed within three days. The sooner this happens, the better for the patient's condition. Therefore, most often it is carried out almost immediately.
With careful actions by surgeons, the patient’s chances of recovery will be quite high. But after this, long-term treatment and constant care will be required.
Classic treatment
Regardless of whether the operation was performed, the patient is prescribed urgent therapy. It is recommended to start it in the first 3 hours after the problem is detected. The patient is prescribed a wide range of medications from different pharmacological groups. They reduce the risk of complications and improve your overall condition.
The doctor chooses therapy aimed at maintaining vital functions:
- Stimulation of the respiratory system. Oxygen therapy is used, the mucus present in the respiratory tract is removed, the trachea is intubated, and a ventilator is connected. Additionally, for pulmonary edema, oxygen inhalation with the addition of ethyl alcohol vapor may be prescribed.
- Decreased body temperature. This requires taking antipyretic medications. Magnesium sulfate or Paracetamol are most often prescribed.
- Normalization of water-electrolyte and salt balance along with biochemical balance, as well as blood osmolarity in those who are in a coma. Infusion therapy (drip) and diuretics are prescribed.
- Reducing cerebral edema, maintaining its normal state. Corticosteroids, osmotic diuretics, and sedatives are used. The most popular: Mannitol and Albumin solution. Drainage of cerebrospinal fluid is also often required.
- Stabilization of pressure, correction of heart function. The patient is taking beta-blockers, calcium channel blockers, ACE inhibitors, diuretics, corticosteroids, and cardiotonic drugs. Infusion therapy with Labetalol, Enalapril (for hypertensive patients) or Dopamine (for hypotensive patients) is almost always prescribed.
- Strengthening the walls of blood vessels. Medications are prescribed individually and have a strong effect on the entire vascular system.
- Elimination of infectious contamination. Prevention involves taking uroseptics and antibiotics. Assigned individually if necessary.
- Symptomatic therapy. Drugs whose action is directed against nausea, vomiting, convulsions, and excessive agitation. The most commonly used are Thiopental, Diazepam, Cerucal, Fentanyl.
- Piracetam. Selected by the attending physician.
- Antioxidant effect. Emoxipin, Mildronate and other medications are prescribed, as well as vitamin E.
The patient has been in the hospital for about a month. This is followed by a long recovery period.
Development mechanisms
Intraventricular hemorrhage in the brain in immature children is usually located in the region of the caudate nucleus and thalamus, since the germinal matrix is located in this area. The blood supply to this area has some peculiarities - a well-developed network of vessels with a fragile wall. As a result, even a temporary increase in arterial or intracerebral pressure leads to overflow of the veins in this area, and then rupture of blood vessels - intraventricular or periventricular hemorrhage.
On the other hand, with low blood pressure, which is the result of a pronounced decrease in oxygen in the blood, ischemia of brain tissue develops, which can provoke hemorrhagic impregnation.
There is no evidence of which mechanism is more common, but it is clear that the main problem is fragile vessels that are very sensitive to pressure changes. And the less mature the child, the more vulnerable his blood vessels are.
Symptoms
The clinical picture of hemorrhages does not always appear immediately after the birth of the baby; the problem may not manifest itself in the first days of life. In this case, the signs depend on the location and degree of vascular damage.
In the general picture, the symptoms will be as follows:
- the baby's hyperexcitability abruptly changes to depression;
- tense and swollen fontanel;
- crying and screaming intensifies in the newborn;
- rapid pulse;
- frequent regurgitation;
- lack of appetite;
- increased gas formation;
- stopping breathing movements;
- shortness of breath, suffocation;
- anemia;
- increased content of ketone bodies in the blood and bilirubin, which provokes intoxication of the body;
- muscle weakness;
- moderate tilting of the head;
- one or two-sided paralysis of the extraocular muscles;
- the beginning of the development of renal and cardiovascular failure;
- the addition of a secondary infection, resulting in the appearance of sepsis, pneumonia or meningitis.
In some cases, the clinical picture will vary; it depends on the form of hemorrhage and the degree of spread. An accurate diagnosis can only be made after neurosonography.
Clinical picture of various forms of intracranial hemorrhage:
- VZhK. In grades 1 and 2, symptoms may not appear, and the situation may not be aggravated by neurological disorders. If IVH of the 3rd or 4th degree is diagnosed, there are clear signs of swelling of the fontanelle, convulsions, impaired respiratory function, and disruptions of the cardiovascular system. As the problem develops (due to an increase in fluid volume and compression of the nerve centers), lethargy appears, reflex function is suppressed, and the size of the head increases. The breakthrough of blood from the walls of the ventricles into the brain tissue leads to parenchymal hemorrhage.
- Subdural and epidural hemorrhage. Blood accumulates between the bone tissue of the skull and the dura mater, forming a bag with accumulated fluid, which subsequently turns into a hematoma. The problem occurs due to mechanical compression of the head during delivery. Symptoms have 2 phases. At the first stage, convulsions appear, reflex ability decreases, and fainting is possible. In the second phase, imaginary enlightenment appears.
- Subarachnoid hemorrhage. The clinical picture is wavy. In the first 2-3 days the child has no visible signs. Then depression or excitement appears. The resulting convulsions can be replaced by imaginary well-being. The prognosis for life depends on the degree of damage and timely treatment.
When making a diagnosis and prescribing treatment, the doctor is guided by the results of CT, MRI, ultrasound, x-ray and neurosonography. Only after this can we talk about further forecasts.
Causes
List of factors that increase the risk of cerebral hemorrhage:
- The main cause of cerebral hemorrhage in a premature baby is oxygen deficiency that occurs during pregnancy or childbirth.
- Very low birth weight - less than 1500 g.
- High or low blood pressure.
- Respiratory distress syndrome, pneumothorax.
- Electrolyte blood disorders.
- Heart failure.
- Pathological acidosis.
- Reduced body temperature.
- In premature babies who have suffered oxygen deficiency due to asphyxia, the brain is not able to automatically regulate blood circulation, as happens in adults and full-term babies.
- Affected walls of brain vessels as a result of intrauterine viral or mycoplasma infection.
- Irrational care and medical manipulations: strict regime of artificial respiration;
- a large number of hyperosmolar drugs;
- high doses of administered oxygen;
- carrying out painful procedures without anesthesia;
- simultaneous administration of many drugs that affect the platelet component of blood coagulation;
- birth injury.
The likelihood of birth trauma during premature pregnancy increases due to the fact that the birth canal is not prepared for the birth of the child, the situation is complicated by rapid or, on the contrary, long-term labor, the application of a vacuum and forceps during childbirth.
When the mother regularly smokes, the fetus experiences a chronic deficiency of nutrients and oxygen.
Severe consequences for a premature baby can be expected if his mother suffers from alcoholism, drug addiction, smokes, has a large number of previous pregnancies, if the birth was not in a maternity hospital and the baby had to be transported to the hospital.
Cerebral hemorrhage in children born before the end of the normal pregnancy period is observed with a combination of 3 or more risk factors.
Types and degrees
Pathology in an infant is characterized in relation to accepted parameters. WHO has established 3 degrees of violations, in Russia it is customary to differentiate 4 degrees. In the first case, the ventricles of the brain are not injured, the hemorrhage is localized in the walls. In the second, blood penetrates into the cavities; in the third, it spreads from the ventricles to the surrounding tissues. In the fourth degree, all ventricles and medulla are affected.
Important information: What to do if a newborn’s navel is bleeding (bleeding) and why a little blood is released from the baby’s umbilical wound
Epidural
This type of pathology is caused by rapid labor, post-term pregnancy with anticipation of spontaneous labor, and underdevelopment of the skull bones in the prenatal period. The vessels are damaged between the dura mater of the brain and the skull. Signs begin within 72 hours of birth.
Subdural
In 95% of cases, they appear during spontaneous childbirth if the baby’s head does not correspond to the size of the mother’s pelvis. They are detected immediately by the absence of the necessary reflexes or the appearance of convulsions. With such brain damage in newborns, blood accumulates between the soft and hard membranes of the brain.
Subarachnoid
The likelihood of occurrence increases with the application of obstetric instruments or personnel error. Blood accumulates in the tissues, membranes and under the membranes of the brain.
Parenchymal and intraventricular
Appears during pathological pregnancy, intrauterine infection, and prematurity. Blood can accumulate in both ventricles at the same time or in only one, as well as in the connective tissue.
Varieties
There are 3 degrees of severity:
- Mild degree - the brain does not have serious disorders. But mild degrees of severity can smoothly flow into more severe ones.
- The average degree is complicated by stupor, muscle hypotonia, and hydrocephalus.
- Severe degree is considered severe hemorrhage with all possible consequences.
Stages of the disease:
- Acute period - 1st week.
- Subacute or early recovery – the first 3–6 months.
- Late recovery period - can last from 4 months to 2 years.
Consequences
After suffering a cerebral hemorrhage, the consequences can be very different and vary depending on the complexity of the disease. The most severe consequences occur in patients who have been in a coma for a long time.
Previously, we have already considered the issue of the consequences and treatment of a stroke on the right side.
Consequences:
- In the first year, there is a high probability of repeated hemorrhage, so you need to be extremely careful and follow the doctor’s recommendations.
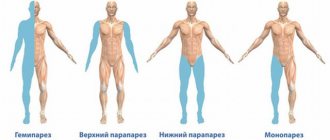
- Paralysis of the muscles of the face and tongue.
- Loss of sensation in half the body.
- Loss of half of the visual field.
- Speech apparatus disorders.
- Mental disorders.
The first year after illness is important; the favorable prognosis depends on this period of recovery. 3 years after the hemorrhage, irreversible processes of extinction of unrestored body functions occur.
Internal cerebral hemorrhage is a serious diagnosis that requires rapid response and comprehensive treatment.
Despite the long rehabilitation period, the overall prognosis for life after hemorrhage is positive. 09.14.2016
Signs of the disease
Premature newborn on a ventilator
In premature babies, it is sometimes difficult to identify the disease, because the nervous system is still immature, and the general symptoms of the premature body come to the fore: respiratory disorders, intrauterine infections, metabolic disorders. Symptoms and their combinations can vary significantly depending on the age of the child, the volume and location of the source of circulatory disorders.
Main symptoms of the acute period:
- Signs of respiratory disorders and lack of spontaneous breathing come to the fore.
- Signs of general suppression of the functions of the most important organs and systems: muscle hypotonicity; due to muscle weakness, the child moves little or does not move at all; decreased reflexes; the baby's cry is weak or absent; there are no sucking and swallowing reflexes; there is a tendency to low body temperature, regurgitation, vomiting, attacks of respiratory arrest and slow heart rate.
- Increased excitability: muscles are hypertonic or dystonic; revitalization of reflexes may be observed; rapid and rhythmic trembling of the limbs and body; slow tonic spasms of the face, limbs, body.
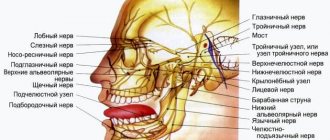
- Symptoms of focal lesions: gross convergent strabismus; involuntary oscillatory eye movements; "setting sun" symptom.
- Symptoms of hydrocephalus and intracranial hypertension - fontanelles swell, skull bones diverge.
Symptoms and signs
Pathology can be detected immediately after birth, within a few hours or even days. The diagnosis is made by characteristic symptoms in children, laboratory and hardware examinations.
Signs of cerebral hemorrhages depend on the type of hemorrhage:
- With an epidural, breathing is heavy, the pulse is rare, the pupil on the injured side is dilated.
- Subdural causes muscle weakness, unconditioned reflexes are absent, and infants experience convulsions that are repeated cyclically. It is difficult to stop without the use of pharmaceuticals.
- Subarachnoid is accompanied by hyperactivity, increased excitability, difficulty falling asleep, and frequent monotonous crying. Possible squint.
- Ventricular and interventricular can lead to apnea - cessation of breathing.
Common symptoms that may indicate the presence of pathology in infants are frequent regurgitation, weakness or hyperexcitability, developmental delays, headaches, which are indicated by moaning on one note and attempts to reach the forehead with hands. One should be alert to periodic holding of breath, numbness with increasing pallor of the skin, a sharp drop in temperature, absence of a sucking reflex, and loss of appetite. Accumulation of blood in the brain tissue is indicated by paresis of the limbs and stiffness of the neck muscles.
Important information: Side effects after taking Escapel and does bleeding rule out pregnancy?
Diagnosis of a newborn is carried out in the maternity hospital. To assess the condition, general and specific blood tests are done - necessarily a coagulogram, puncture - to analyze the cerebrospinal fluid and cerebral fluid for the presence of blood fragments. X-rays of the skull, neurosonography, MRI or CT may be required. If the pathology is detected later, it is indicated by changes in behavior, in which case outpatient examinations are possible.
Complications
Intracranial hematomas in some cases can become a further cause of the development of cerebral palsy
If the hematoma has not been diagnosed, then the child may experience increased cerebral edema, dislocation of brain structures, which will lead to the death of the patient. Severe long-term complications may include multiple hemispheric cysts that communicate with the ventricles, ventricular enlargement, hydrocephalus, severe neurological deficit, and cerebral palsy.
All of these complications are serious, because they can further negatively affect the neuropsychic and physical development of the child and lead to severe disability.
Diagnostics
If a brain injury is suspected, all newborns in the maternity hospital undergo neurosonography - an ultrasound examination of the brain and spinal cord. A CT scan of the brain is possible.
Carrying out neurosonography
Treatment
The basis of treatment is supportive symptomatic therapy. Children should be in a protective mode, reminiscent of that in adults during a stroke: sharp sounds and intense light should be eliminated, examinations of babies should be gentle, the remainder of the umbilical cord should be processed and diapers should be changed very gently and gently in order to disturb the baby as little as possible. The child must be in a special heated cuvette; during this period, neither hypothermia nor overheating is acceptable.
A very important condition is that the child should not starve.
For this, babies are given a tube, even if the baby is almost full-term and could feed himself, bottle feeding is recommended; sucking milk from the breast is a heavy burden for such a baby. Additionally, droppers with parenteral nutrition can be connected.
The child must be under constant control of the most important vital functions: blood pressure, pulse, breathing, temperature, urination, body weight, and arterial blood counts are monitored.
Symptomatic treatment of intracranial hematoma
Medicines are prescribed sequentially, depending on the main symptoms, severity of the disease, and the nature of concomitant disorders:
- If there is increased bleeding or a tendency to hemorrhage, Etamzilat, Dicynon, Vikasol (Vit. K, Menadione) are prescribed.
- To eliminate seizures - Diazepam, Phenobarbital, Sibazon.
- For cerebral edema and increased intracranial pressure - Lasix, Diacarb, Mannitol, Furosemide, Dexon.
- To restore intestinal flora, preparations based on lacto- and bifidobacteria - Bifidumbacterin, Lactobacterin.
- For respiratory problems - Ambroxol, a surfactant (Curosurf) is injected into the trachea.
- Piracetam can be prescribed to stimulate brain function.
- Antibiotics are used to treat bacterial inflammation.
Symptoms of cerebral hemorrhage
Recognizing a cerebral hemorrhage is quite difficult due to the extensive pattern of symptoms. But it is very important to diagnose the disease as quickly as possible; the life of the victim and its further usefulness completely depend on this.
The first 6 hours are decisive; if during this time the patient is transported to a medical facility and measures are taken, then the prognosis is favorable.
Signs:
- Sudden numbness of the face or limb (for no apparent reason).
- Disorientation. The person does not understand where he is and speaks poorly.
- Double image in the eyes.
- Vomiting, nausea.
- Cramps.
- Eye paresis, mydriasis (pupil dilation), smoothness of facial muscles, drooping corner of the mouth.
- A person cannot smile if asked to do so.
- The patient cannot lift both limbs up.
- The tongue is twisted. When trying to say a sentence, the speech is slurred.
The clinical picture depends on the area and area of brain damage. In most cases, the departments responsible for speech and movement are affected. If at least one of the listed signs is present, a person must be referred to a medical facility to confirm the diagnosis and treatment.
Symptoms differ in different periods of the onset of the lesion:
- Acute period. The presence of cerebral signs, increased intracranial pressure. Necrosis and swelling of the brain are possible - which inevitably leads to death.
- Recovery period. 2-4 weeks after the rupture of blood vessels, the processes of removing blood and restoring the structure begin. The duration of this period varies from person to person - several months.
- Period of residual effects. This is a conditional name, because the body recovers throughout its life. With proper treatment and a gentle lifestyle, it is possible to rehabilitate vital functions and even performance.