History of disease diagnosis
The symptoms of anorexia nervosa were first described in 1684 by Richard Morton under the name “mental passion.”
The doctor described an amazing picture - an extreme degree of exhaustion with amenorrhea in a young girl. At the same time, she continued to maintain a high level of activity, walked a lot, read, and even took notes on what she read (which was uncharacteristic of other types of exhaustion, for example, with tuberculosis). The doctor assumed some serious unexplored illness behind such a clinical picture. He proposed treatment methods available at that time - “bitter pills” and “antihysterical water” containing castor oil and ammonia. After a slight improvement, the patient refused treatment, deciding to “leave everything to nature.” The doctor agreed, which he later bitterly regretted: after 3 months, the girl’s condition worsened sharply, fainting resumed, after which she died. Morton later describes a similar clinic with another patient with whom he worked more successfully. This first example of diagnosis and treatment, which looks naive by modern standards, shows the main difficulties of working with anorexia nervosa. It demonstrates a low willingness of patients to contact a doctor, as well as a severe course, including death. Later, the diagnosis of anorexia nervosa was described in more detail in the 19th century by W. Gull (1868) and Ch. Laseque (1873), who almost simultaneously and independently published works on this disease. It was Gull who coined the term Anorexia Nervosa, which later became established as a diagnosis.
Prevalence of anorexia
Cultural and technological progress had a huge impact on the spread and pathomorphosis (change over time) of anorexia. So, in the 60s of the 20th century, the singer and supermodel Lesly Hornby, nicknamed Twiggy (from the English Twig - reed), was popular, who, with a height of 169 cm, weighed 40 kg. Her image became a reference for many girls of that time. It contributed to the rise of anorexia as a social disorder.
Currently, anorexia belongs to the group of mental eating disorders, code F50.0 in the International Classification of Diseases, 10th revision (ICD-10).
The prevalence of anorexia, according to various sources, ranges from 0.016% to 1.2% in different populations in women, and much less in men - up to 0.29%. However, over the past decades there has been a clear upward trend in the rate of anorexia in both women and men.
Refusal to eat
It is impossible to reduce the idea of the symptoms of anorexia only to the fact of conscious refusal to eat. The disease can occur for a short time, against the background of some somatic pathology, or be long-term or chronic in nature, due to the presence of a mental disorder, or the use of certain psychotropic medications. Thus, depending on the true causes of the development of the disease, “specific” signs of anorexia can be identified that have different motivations for refusing to eat.
Somatic pathology
Malignant tumors, pathology of the endocrine system or some neurological diseases may be accompanied by signs of anorexia - lack of hunger and, accordingly, refusal to eat, not with the goal of getting rid of excess weight, or adjusting the figure in ways that are dangerous to life and health.
Mental disorders and pharmacotherapy
Symptoms of anorexia (lack of appetite, refusal to eat and weight loss) can appear against the background of various mental disorders (for example, against the background of depression, bipolar affective disorder, mania), as well as due to the use of mood correctors that have the property of suppressing appetite.
Psychogenic factor
The most well-known signs of anorexia, which the disease is associated with in everyday life, include conscious refusal to eat and adherence to strict diets. It is the psychopathological aspect of deliberate weight loss that allows us to classify this type of eating disorder as anorexia nervosa (F50.0 according to ICD-10), excluding the causes of underweight given above.
Differential diagnosis allows you to establish the exact cause of refusal to eat and make the correct diagnosis. The importance of differential diagnosis cannot be underestimated, since the appropriateness of the prescribed treatment for anorexia directly depends on the correct diagnosis.
Course of the disease
The typical course of this disorder begins at the age of 14-16 years in girls; much less often, the onset occurs in adulthood. As a rule, the basis of anorexia is a girl or boy’s dissatisfaction with his own body against the backdrop of excessive concentration on his own appearance. Most teenagers are characterized by fixating attention on appearance and compliance with certain social stereotypes, but in this case this process takes on a comprehensive, overvalued character. This is why social stereotypes have such a big impact.
Another psychological feature of patients with this disorder is impaired body image and dysmorphophobia (an unreasonable fear of one's own ugliness). Such people, although objectively of normal or underweight, still feel full and begin to take steps to lose weight. From this moment on, the flywheel of anorexia begins to spin.
In behavior, anorexia nervosa is characterized by a sharp restriction of food intake, sometimes with fanciful features: patients, for example, can eat only one food and exclude all others from food. In addition, they use so-called purging behavior (inducing vomiting, laxatives and diuretics without a doctor’s prescription), and severe (sometimes grueling) physical activity. Among the behavioral characteristics, the patients’ desire to put on many layers of clothing (hiding their own body), fear of eating, especially in public places, constant talk that the person has “put on weight” against the background of ongoing weight loss, decreased mood, etc. also attract attention. loss of interest in previous activities.
Psychosomatic nature of anorexia
Not only social role models, but also family may play a special role in the relationships of such patients, as well as in the development of the disorder. Most often, patients with anorexia have difficult relationships with family members, especially with their mother. Usually these are tough, rigid, controlling relationships on the part of the mother and rebellious, protest relationships on the part of the patients. Patients with anorexia usually find it difficult to build sincere, trusting relationships with anyone, including psychologists or psychotherapists. If this can be done, then the trust that has arisen can be used to alleviate symptoms.
Another option for the onset of anorexia is the transformation of bulimia. In this case, the onset of the disorder is accompanied by episodes of uncontrolled overeating, which after several months or years turn into food refusal with weight loss.
Causes of anorexia
The main cause of anorexia is mental disorders, something that happens in a person’s head that makes him behave this way.
The author of this article adheres to the point of view according to which isolating anorexia into an independent nosological unit is not advisable (many will not agree with this - maybe I’m wrong, write comments, let’s discuss).
If we consider anorexia not in isolation, but within the framework of chronic psychopathology (personality disorder, schizophrenia, “schizo-like” - schizotypal, schizoaffective disorders, etc.), then its etiology should be studied from two positions. The first is the etiology of chronic mental illness. We will not talk about this in detail here. The second is the reasons that led to the development of this particular syndrome and not another in the patient (usually the patient). Let's talk about this.
To begin with, let's say that there are studies showing the connection of anorexia with genetic factors (heredity), as well as with the level of various hormones in the body. These studies, however, again treat anorexia as a separate phenomenon. Without excluding the influence of these factors, in most cases the obsessive desire to lose weight is associated with a fixation on ideas of inferiority of one’s appearance. A girl or woman thinks that she is fat, that she can get fat, that despite her overall thinness, in some places there are still cosmetic defects associated with “fatness,” excessive fat deposition, etc. Sometimes a woman realizes that she is not fat, but on the contrary, but still refuses food, because it seems to her that if she starts eating, she will get fat. At some stage, the idea of refusing food can take on a separate life of its own; a woman will refuse to eat because as soon as she eats or thinks about food, she experiences mental or even physical discomfort. At the same time, sometimes a woman, contrary to common sense, may be convinced that it is excessive thinness that makes her attractive. Or she herself may not consider herself attractive in this way, but have the belief that this is how she looks attractive to men. In short, there can be many cockroaches in the head associated with anorexia, and they can be different. A specialist - a psychiatrist or psychotherapist - can deal with them.
The “cultural factor” plays a huge role in the etiology of anorexia - the spread in society of ideas and stereotypes that associate beauty with exhaustion. The influence of such ideas is especially dangerous in adolescence, when personality in general and sexual preferences in particular are being formed. The spread of these ideas is facilitated by the fashion industry, which instills standards of beauty associated with excessive thinness. As well as coverage in a positive context of the lifestyle, views and behavior of some “stars”, famous personalities suffering from anorexia. There is no doubt that in reality such an idea of beauty is unnatural and not physiological (a woman with a narrow pelvis is less likely to be able to give birth to a child normally, a woman prone to excessive thinness will have problems with bearing it and even with the possibility of conceiving, exhaustion contributes to the development of various diseases and so on.). This allows some to argue that the idea of exhaustion, excessive thinness, as a sign of beauty, is part of a depopulation program (reduction or limitation of population growth, birth rate), beneficial to certain circles (we will not dwell on the discussion of this point of view here).
As is the case with almost any mental illness, provoking factors for anorexia are stress, nervous tension, alcohol and substance use, and disturbances in sleep and wakefulness.
Repeated attempts to identify certain types of relationships in the family or character traits that correlate with the likelihood of anorexia, oddly enough, have not yielded clear results. Or, more precisely, they gave, but the most general: low self-esteem correlates with the risk of anorexia, psychopathologically burdened heredity correlates. It would seem logical to assume that if a girl is constantly reproached for being fat, she is more likely to become anorexic. But no, even at this level it doesn’t work - some will fall into depression, some won’t, some will give up on it and stop taking care of themselves, some will “out of spite” begin to gain weight even more, etc. There are probably some premorbid features (theoretically), but the question is much more complicated than it seems at first glance.
Anorexia in men
Male anorexia is much less common than female anorexia. The course of anorexia in men has its own characteristics. As a rule, such boys and men are extremely focused on maintaining muscle mass and muscle definition, which is considered the main sign of masculinity. Therefore, anorexia in men is often accompanied not so much by vomiting or eating disorders, but rather by excessive physical exertion, which becomes the dominant factor in behavior to the detriment of relationships, work, and other values. Even injuries and illnesses cannot stop such men from going to the gym and grueling sports.
In any case, anorexia is accompanied by decreased mood, depressive episodes, loss of initiative, difficulties in relationships with peers and family members, sometimes emotional instability, but always by an excessive fixation on the image of one’s own body, accompanied by a distorted vision.
Symptoms and signs of anorexia in adults
Entering adulthood can be a strong stress factor for a person who has prerequisites for an eating disorder with developed addictive behavior. By this time, a person’s weight can decrease by 20–50% of normal, and therefore the symptoms of anorexia in adults become obvious, almost completely developing the picture of the disease.
Symptoms of anorexia in adults include:
- fast fatiguability;
- dizziness, fainting;
- decreased heart rate;
- low blood pressure;
- damage to blood vessels on the face;
- puffiness of the cheeks;
- hair loss;
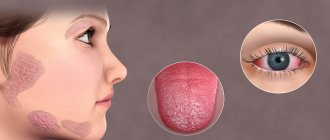
- dry skin;
- body hair growth;
- cessation of menstruation;
- lack of sexual desire;
- gastrointestinal disorders.
Symptoms of anorexia in adults at the final stage include irreversible degeneration of internal organs, protein-free edema, lack of subcutaneous fat, trophic changes in the skin and muscles, and myocardial dystrophy. Serious failures appear on the part of internal organs and systems. However, against the backdrop of extreme exhaustion, such people continue to refuse food, considering themselves fat.
Anorexia in children and adolescents
In children of preschool and primary school age, anorexia nervosa can develop due to stress and an overly critical assessment of their body. In girls, this condition is observed more often than in boys, since girls begin the process of puberty and socialization as an adult earlier. Childhood anorexia is a fairly rare phenomenon. In each case, psychologists work with the entire family.
In adolescents, this disease is much more common. Its manifestations are associated with the fact that the teenager’s body undergoes changes that can be perceived negatively. At the same time, there is a need to please peers, to be ideal. Teenagers look at photos of celebrities and want to look the same.
In adolescence, the risk of anorexia does not decrease. Young boys and girls with problems with self-esteem become independent, parental control weakens, so the symptoms of the disease may not be noticed immediately.
Symptoms
From the point of view of the somatic course of the disease, a sharp loss of body weight, including muscles, attracts attention. Girls often lose their periods (usually when they weigh less than 45-47 kg). Patients often experience problems with the functioning of the gastrointestinal tract, constipation, various laboratory test abnormalities (deviations from the norm of hormones, microelements, hemoglobin, etc.), dizziness and fainting, swelling of the salivary glands, weakness, dental problems, brittle hair and nails, a constant feeling of cold due to a lack of adipose tissue.
Stages of development
The course of the disorder can be divided into 3 stages:
- Body dysmorphomania: characterized by impaired perception of one’s own body with a feeling of imaginary fullness, decreased mood, anxiety, and the search for the “ideal diet”
- Anorectic. During this period of time, there is a total refusal of food, a sharp (20-30%) loss of body weight, and somatic manifestations of the disease manifest themselves. On an emotional level, during this period, patients often feel uplifted with an increase in mood, as they feel imaginary success in solving their weight loss task.
- Cachectic: body weight deficiency can reach 50% of predicted. At this phase, systematic disturbances in the functioning of internal organs (heart, adrenal glands, gastrointestinal tract) begin, so-called oncotic edema begins due to protein deficiency. In the absence of proper treatment, this clinical picture ends in death.
Diagnostics
Due to the fact that anorexic men do not consider themselves sick, the percentage of self-seeking professional help is low. Most often, the alarm is sounded by relatives and close friends who have begun to notice the manifestation of certain symptoms of a psychological disorder. After the patient ends up in a specialized medical institution, the doctor’s task is not only to make a correct diagnosis, but also to conduct a comprehensive diagnosis of the whole organism.
Currently, the diagnosis of anorexic condition is carried out according to the following criteria:
- prolonged causeless lack of appetite;
- change in body weight by 25% or more compared to usual values;
- obsession with losing weight;
- inadequate assessment of one’s appearance and condition:
- critical drop in hemoglobin level in the blood;
- gagging after eating, etc.
The doctor talks with the patient, performs a set of laboratory tests, conducts ultrasound diagnostics and other studies if necessary. After the diagnosis is confirmed, the patient is admitted to a hospital, where the long road to recovery begins.
Treatment
As a rule, the treatment of anorexia is associated with significant difficulties. This disease disrupts all levels of human functioning – psychological, biological and social. It is believed that within 10 years the mortality rate from anorexia is one of the highest among all mental disorders - according to various estimates, from 5% to 30% of the total number of patients. The causes of death are increasing multiple organ failure of internal organs, additional infections as a result of weak immunity, as well as suicide attempts with parallel ongoing depression. Anorexia therapy should be carried out at all levels.
In the treatment of this disorder, it is first necessary to ensure that the patient’s life is not in danger. If there is a threat to life, the patient must be treated inpatiently - therapeutic or psychiatric, depending on the nature of the clinical picture. In stationary conditions, a comprehensive examination is carried out, the necessary therapeutic measures are taken, including parenteral nutrition. However, it is necessary to understand that in a hospital you can relieve the severity of the condition, remove the threat to life, but not cure anorexia. The main emphasis in patient treatment is long-term outpatient treatment, but especially psychotherapy.
Treating patients with anorexia and underweight is much more difficult than treating overweight patients. Unfortunately, there are no medications specifically targeted against anorexia. Antidepressants, mild tranquilizers or antipsychotics may be used according to indications, but their effectiveness is difficult to predict. The main emphasis in treatment should be on psychotherapy.
Often, psychological changes in anorexia are rigid and comprehensive, so the first phase of psychotherapy is building a trusting relationship with the patient. Then it is necessary to develop in him an awareness and acceptance of the symptoms of his own disorder, since some such patients come to a psychotherapist not to work with anorexia, but in order to continue to lose weight even more effectively! Psychotherapists working with overweight people need to be constantly vigilant and diagnose patients with anorexia in a timely manner, especially if the work is carried out in a group and remotely.
The main goal of treating anorexia is to gain weight to at least minimal normal values. This often requires special nutrition and the use of dietary supplements, the composition of which is determined based on the results of blood tests and assessment of the clinical condition. The main problem is that patients and doctors usually differ in treatment goals: patients, influenced by their distorted self-perception, want to lose further weight, and doctors try to help them gain weight back to normal values. Therefore, an important link is the use of psychotherapeutic methods.
One of the most proven methods of working with such patients is cognitive behavioral psychotherapy. It is a set of specially developed techniques with patient management protocols aimed at changing the patient’s thinking, his rigid dysfunctional beliefs, normalizing his own body image and teaching rational nutrition. For example, among modern approaches, dialectical behavior therapy stands out, in which special approaches have been developed specifically for patients with anorexia nervosa.
Non-directive hypnosis can also be used as an auxiliary approach, which allows you to reduce emotional stress and create a more positive image of your own body. An important stage in working with such patients is family therapy, that is, working with loved ones. Often their behavior influences the patient’s condition and behavior, and sometimes they themselves need the help of a psychotherapist to cope with their own anxiety or depression.
In this regard, the method of systemic family therapy developed at the Maudsley Clinic in London deserves special attention. This method is used on an outpatient basis, only at the initial stage (if necessary) implying inpatient treatment. The therapy process is divided into 3 phases:
- Body weight normalization phase: involves primarily improving the patient’s somatic condition, correcting nutrition in order to eliminate the risk to life and health. The role of psychotherapy here is to identify the characteristics of family communication and family patterns of eating behavior. The task of the psychotherapist is to help parents acquire special skills that can provide assistance to the child during recovery.
- The phase of regaining control over nutrition: criteria for readiness to move to this phase - a steady, albeit minimal at first, increase in body weight, the patient’s acceptance of the parents’ requirements regarding nutrition and positive changes in the psychological climate of the family. The task of parents and therapist at this phase is to help the child regain control over his eating behavior, with minimal psychological pressure.
- Restoration of the patient’s identity: the criterion for the beginning of this phase is normalization of weight at a level of at least 95% of normal values, removal of inadequate dietary restrictions. The main goal of psychotherapy is to return the patient’s own identity, maintain healthy relationships acquired at earlier stages, and also discuss with parents the changes that will happen to the child after he gains full autonomy.
In general, therapy for eating disorders requires complex lifestyle changes - changing beliefs, correcting body image, improving emotional regulation and interpersonal skills, learning to eat rationally, and some other actions. At the same time, each patient remains unique, inimitable, each case requires the development of its own approach. Unfortunately, it is almost impossible to create a single psychotherapy template that can be used to achieve a guaranteed result in anorexia.
Moreover, like many other mental disorders, anorexics are sometimes prone to relapse. The reason for the return of symptoms may be some external stress factor, exacerbation of depression, pregnancy, as well as many other reasons. It is good if by this point the patient has already formed a trusting relationship with his doctor, whom he can contact again if symptoms reappear.
Causes
Each type of disease develops as a result of different reasons. Mental anorexia is a consequence of a mental illness such as schizophrenia, paranoia or depression. The causes of the development of other forms of the disease may be physiological and psychological factors. Physiological factors are mainly responsible for the development of symptomatic and drug-induced anorexia. Physiological causes of anorexia include:
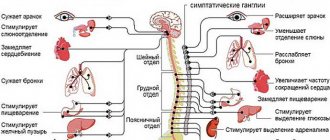
- disruption of brain hormone levels (decreased serotonin, norepinephrine and increased cortisol);
- development of somatic diseases of organs;
- drug abuse, mainly antidepressants.
The psychological causes of the disease anorexia give rise to its most common form - nervous. These include:
- desire to control your life;
- the desire to meet the demands of the surrounding world;
- perfectionism;
- an inferiority complex instilled at an early age as a result of improper upbringing;
- psychological trauma;
- physical or sexual violence.
Anorexia appears under the influence of both the patient’s own desire for ideals and the provocation of this desire by others.