Are all people equally susceptible to the virus?
People are susceptible to this virus almost equally, but there are a number of provoking factors. After an illness, it is impossible to become infected with the same type a second time, but to become ill with the other two is quite possible. Cross immunity does not develop, so the danger remains.
Conditions conducive to the spread of the polio virus are:
- children's failure to comply with hygiene rules;
- unsatisfactory sanitary and hygienic conditions;
- lack of total vaccination in the region of residence;
- AIDS, tuberculosis;
- the presence of wounds after muscle injections and surgically removed adenoids/tonsils.
A factor that increases the risk of the disease is the live (containing weakened viruses) polio vaccine administered against a background of weak immunity.
Children under seven years of age are the most susceptible category; with age, the risk of infection decreases.
When is a sick child contagious?
To understand how you can become infected, you need to know exactly some time frames for the course of the disease.
A sick child becomes a source of virus release into the external environment during the entire incubation and acute period. All body fluids - feces, saliva, tears, nasopharyngeal discharge, blood, lymph, digestive juices - contain a huge amount of viable virus.
The most dangerous period for the environment is 3 weeks from the onset of clinical manifestations. This is the time when virus shedding peaks. All people who come into contact with a sick child can either become sick or become carriers. During this time, isolation is necessary; in Russia, the child is placed in an infectious diseases hospital. But even there, the strictest sanitary and hygienic measures are observed, including not only the exclusion of any contact with everyone except the medical staff, but also the complete sterilization of dishes, feces and all items used by the patient.
All children and adults who have been in contact with the sick person must be identified. They are not placed anywhere, they are simply observed every day, and, if necessary, sent to a laboratory to determine carriage. In Russia there are regulatory documents on this matter.
The routes of infection with polio are so routine that the only way to stop the infection is through universal vaccination.
How does infection occur?
The routes of infection (infection) with polio are different. The manifestation of infection begins in the oral mucosa, and less commonly in the intestines (depending on the method of infection). The virus begins to multiply in the tonsils (or intestines) and regional lymph nodes, then enters the circulatory system. The virus enters the CNS (central nervous system) hematogenously. Destruction of nerve fibers causes paralysis. Not only the central nervous system, but also the heart can be affected.
Basically, forms of the disease develop that do not lead to disability, or viral carriage occurs. The first signs are similar to those of a cold. After some time, the intestinal tract suffers, and here you need to see a doctor.
How can you become infected with polio? There are three options. They will be discussed below. Most often, the disease at the initial stage does not produce symptoms, or it is similar to relatively harmless acute respiratory infections and acute respiratory viral infections. Obvious symptoms appear differently for everyone. This takes from three days to a month (this is how long the incubation period lasts), most often it is the ninth to eleventh day. There is no cure for polio; its occurrence can only be prevented by vaccination. To alleviate the patient's condition, symptomatic therapy is used.
Vaccination against polio should not worry others if they are vaccinated, and, as a rule, this is so, because mass vaccination has been carried out in kindergartens for many decades in our country. This is also monitored by clinics, where they provide routine vaccinations to those who do not attend preschool educational institutions. Live vaccination is contagious, the possibility of infection cannot be excluded, but it is minimal and poses a danger only to those who have not been vaccinated.
Routes of transmission of the virus
Poliomyelitis has different modes of transmission. The spreader of the infection is someone who is sick or is a carrier of the virus, but insects (flies) can also become carriers. There are several ways of infection: contact, airborne droplets and oral-fecal. The last method is the most common. The most dangerous carriers are those with hidden forms of the disease. Conditions conducive to infection are the lack of hygiene skills in children, marginal living conditions, and living in places where there is no mass vaccination.
Poliovirus has different transmission mechanisms, but everyone's susceptibility to this virus is approximately the same. The most dangerous age is from six months to seven years. Three-month-old babies are almost never infected due to the immunity they receive from their mother during pregnancy. Fortunately, the paralytic variety is rare, but other forms of polio should not be considered harmless either.
The disease can only be detected using special diagnostic methods. Repeated episodes of morbidity are exceptional because immunity is developed to the transferred type of polio. Unvaccinated children contribute to the creation of an unfavorable epidemiological situation. Immunization of unvaccinated children with OPV, that is, oral polio vaccine, contributes to its normalization.
Is polio transmitted from a pregnant woman to her fetus?
Poliomyelitis is practically not transmitted from mother to fetus, but such cases are not exceptional. Predisposing factors are important here. When infected, the embryo dies in the prenatal period if the infection occurred in the first trimester. If this happens in the middle of pregnancy and in the third trimester, then the fetus almost always dies without being born; for this, artificial labor must be initiated.
In all cases, the virus causes mutations in the fetus, general intoxication, oxygen starvation, developmental delay, and various defects, primarily affecting the spinal cord and brain. Even if the fetus does not die in utero, in a quarter of cases the baby dies in the first months after birth.
Is a child contagious after polio vaccination?
Can an unvaccinated child somehow become infected from a vaccinated child? What are the chances of getting sick from contact with a vaccinated child? There is a possibility, especially if the person in contact does not have an anti-polio vaccination. If everything is in order with this, then the risk is minimal. After the polio vaccine is given, the baby releases viruses (the type that was in the vaccine) into the environment for some time. However, the number of these viruses is small, which reduces the risk of infecting others.
The immune system of vaccinated children who come into contact with a recently vaccinated child is already resistant to this infection. So the answer to the question “Is it possible to have contact with children after vaccination?” – ambiguous. It is possible, but under certain conditions.
During what period is the patient dangerous for others?
So, your child has been vaccinated against polio, is it contagious? Yes, but not for everyone. A sick person or a virus carrier poses a danger to others at any time, except for the time when he has already recovered. It is also important what type of vaccine a person was vaccinated with; this determines whether contact with him or her should be limited:
- inactivated (dead) virus (IPV) is introduced into the body by injection;
- a live, but weakened virus (OPV), the vaccine is administered orally and the child receives it in the form of baby drops.
IPV is safer, but attenuated OPV provides more durable immunization. And, although the risk of illness due to living culture is low, it cannot be excluded. A child vaccinated with the IPV (dead vaccine) method cannot act as a source of infection, but the virus introduced into the body through the OPV (live vaccine) remains viable for almost two months. Therefore, there is a possibility that a vaccinated person who has contact with an unvaccinated person can infect him. But only if he is not vaccinated. This can be both an adult and a child. It is also important to take preventive measures, which include maintaining good hygiene, increasing immunity, limiting contact with a sick person, a virus carrier or a newly vaccinated person.
The possibility of infection of a person vaccinated with a live vaccine is excluded; he develops a strong immunity to the disease, which is, in fact, why vaccination is carried out. After polio vaccination, antibiotics and other medications are undesirable because they adversely affect its effectiveness.
The virus is killed by boiling, contact with chlorine-containing substances, or exposure to UV radiation. In this case, vaccination is the only guarantee of protection against the disease. Can you get infected from a live vaccine? If there is a vaccination, then no. And if vaccination has not been carried out, then there is a risk.
Do I need to do anything after contact with a vaccinated child? As a rule, no special actions are required. When going to countries where the polio situation is not as favorable as in Russia, you must definitely get vaccinated. Those who have had contact with an infected person are quarantined for two to three weeks.
Is it possible to get polio if a child is vaccinated? The answer is clearly negative. The vaccine protects against the type of virus against which the child is vaccinated.
Until what age can you become infected with polio?
The risk of contracting this virus remains at any age, but the highest risk of getting sick is in children under seven years of age. The source of infection is the patient or the virus carrier. Children are more often infected through the fecal-oral and contact routes, that is, through objects, toys, dirty hands, and food.
Is it possible for an unvaccinated child to communicate with a vaccinated child? If a child has just been vaccinated with a “live” vaccine, then contact with him is not recommended for unvaccinated children; the danger is small, but it is there. If the vaccination was given more than two months ago, then there will be no harm from communication. You cannot take the vaccine if you have an infectious disease; you must first treat it.
How long is a child contagious after polio vaccination? Maximum – two months, and only if vaccinated with OPV vaccine (“live”). An inactivated drug contains a killed virus and provides humoral immunity, in contrast to a “live” drug, which includes a weakened virus and promotes the development of tissue immunity. OPV is recommended by WHO due to a number of advantages.
Can a vaccinated child become infected with polio? Only the variety from which it is not grafted.
Complications caused by polio
The most common complications of polio include the following: pneumonia, pulmonary atelectasis, myocarditis, acute dilatation of the stomach, intestinal bleeding.
Treatment of polio
Patients with polio are subject to emergency hospitalization for at least 40 days in special boxes.
In the preparalytic and paralytic phases, the patient needs complete rest. The bed should have a firm mattress without a pillow, the legs should be extended and the feet should be fixed with a splint in a physiological position.
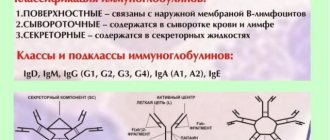
Specific treatment during the preparalytic period is the administration of immunoglobulin at the rate of 0.5 ml/kg body weight, as well as the administration of interferon and ribonuclease. For severe muscle pain, analgesics are prescribed. In case of swallowing disorders, it is necessary to insert a gastric tube; in case of respiratory disorders, artificial ventilation of the lungs is necessary.
During the recovery period, the patient should take drugs of group B, proserin, anabolic hormones, nootropic drugs, and also use physical therapy (paraffin, UHF), and use therapeutic exercises and massage to prevent contractures.
How to stop transmission of the virus
The polio virus is widespread everywhere. Poliomyelitis occurs more often in children than in adults. Cases of morbidity are reported from time to time in different parts of the world. Before prevention, which consisted of universal immunization of the population against polio, the disease systematically made itself known through epidemic outbreaks.
Poliomyelitis is seasonal (autumn-summer), like most intestinal infections, and in warm countries, episodes of infection occur throughout the year. In the fifties of the twentieth century, mass vaccination began, as a result, the incidence rate decreased significantly, and then completely disappeared. The circulation of wild strains has also stopped, and today only isolated cases of infection are recorded in the world.
Mass vaccination is the only measure to stop the transmission of the virus in society. In addition to using preventive methods, you can avoid infection if you limit contact with a child who has just been vaccinated for two to three weeks, maximum for a month and a half, by which time he will stop releasing a certain amount of pathogens into the environment. Particularly concerned parents can take a polio antibody test to check the effect of the vaccine.
There is no effective cure for polio; vaccination is the only way to avoid the disease. The vaccine is relatively safe, does not cause complications and allows the formation of collective immunity. In addition, the presence of provoking factors, such as living in unsanitary conditions, a poor diet, failure to comply with hygiene rules, and so on, should be excluded. After vaccination, you may feel slightly unwell, but not always.
Features of vaccination during an epidemic
Modern mothers often ask pediatricians whether a vaccinated child can get polio during an epidemic, and what consequences he faces. Every mother wants only health for her child.
Relatives and the state are jointly responsible for the emergence of an epidemiological situation. Doctors do not particularly conduct an explanatory policy, and parents, due to a lack of understanding of the severity of the disease, often refuse to vaccinate their children for prevention. In addition, the quality of the proposed vaccine is unknown.
Popular Infection and first symptoms of lymph node tuberculosis
If your child is not vaccinated promptly, he or she may become infected with the polio virus and also put other children at risk of infection, since the disease can often be asymptomatic. What to do if an epidemiological situation arises? Let's consider the algorithm of correct actions:
1. First of all, the child must be given an inactivated vaccine, if it has not been given previously;
2. If the child has already been vaccinated, then during the epidemic, in order not to become infected with polio again, he is given a live oral vaccine in the form of drops. Vaccination is carried out three times with an interval of one month between each;
3. If vaccination is carried out for the first time, then it is necessary to administer the inactivated vaccine to the child two times in a row (with a one-month break between them). During this time, the body will have time to develop immunity to the live polio virus. The third vaccination is droplets.
Is it possible to get sick again?
After suffering from polio, lasting lifelong immunity is acquired to the transferred variety. But only to one out of three, so the risk of re-infection remains. The only consoling fact is that the remaining types of the virus, except for the first, are low-spread. Children's immunity to this disease is weaker, so the age from six months to seven years is considered critical.
Only 1% of cases of infection result in disability; it is caused by a paralytic form of polio, but, in general, non-paralytic forms of the disease or simply virus carriage predominate. Susceptibility to the virus is universal, but it is higher in preschool children, and infants up to three months of age almost do not get sick (due to transplacental immunity). Repeated cases of the disease are recorded very rarely.
Mechanism of disease development
If infection occurs through the mouth, the pathogen first enters the intestines, then, rapidly multiplying, into local lymph nodes, from where it passes into the blood. By hematogenous route, the virus easily enters the anterior horns of the spinal cord, as well as other organs of the central nervous system.
If the pathogen enters the child’s body through airborne droplets, then, settling in the nasopharynx, it is also able to penetrate into the regional lymph nodes, and then into the blood. The pathogen spreads through the bloodstream throughout the body, having a high specificity for nervous tissue.
Treatment
To date, no specific treatment for polio has been developed.
All sick children, including those suspected of polio, should be urgently hospitalized in the infectious diseases department in separate boxes. Strict bed rest is prescribed during the acute period. It is important to limit physical activity in order to avoid the subsequent development of contractures and deformities. For severe pain, medications are prescribed: Analgin, Ibuprofen . To reduce the temperature, antipyretics are used - Paracetamol, Nurofen. If increased intracranial pressure is detected, diuretics are used. During the recovery period (from 3 to 4 weeks), drugs are used that eliminate spasms and improve blood circulation: Proserin, Dibazol, Galantamine . Physical activity is gradually introduced. In this case, a course of therapeutic physical education is prescribed. A positive effect is observed after taking vitamins B and C. Physiotherapy and massage also promote rapid recovery and minimize the amount of residual effects.
Forecast
Atypical and non-paralytic forms of the disease have a favorable outcome, in the absence of infection and the development of complications. The paralytic form has a more serious prognosis and depends on the level and depth of the lesion. Mild paresis passes without a trace, and deep lesions often form residual effects. The course of the disease with damage to the facial nerve (pontine form) has a good prognosis for life, however, paresis or paralysis of the affected nerve may persist. The bulbar form, especially when the respiratory and vasomotor centers are involved in the pathological process, has a poorer prognosis, which can be fatal.