Intracranial pressure (ICP or hypertension syndrome) is a common phenomenon in pediatrics. Therefore, this diagnosis can be given to any baby. Short-term hypertension is even more common - for example, during infectious diseases or during unfavorable weather conditions. What reasons provoke increased intracranial pressure and what symptoms indicate the presence of pathology? How can I measure intracranial pressure in a child and what treatment methods are available? What consequences can result from prolonged neglect of the disease and what preventive measures will help prevent hypertension?
A child has intracranial pressure - what is it?
Intracranial pressure is an increase or decrease in the volume of cerebrospinal fluid (cerebrospinal fluid, which is located in the subdural space between the membranes of the brain) inside the skull. But ICP in children is not an independent disease, but only a symptom of some pathology in the body.
If increased ICP is permanent and there are disturbances in the physical or mental development of the child, it is necessary to contact a therapist or pediatric neurologist and not let the disease take its course.
Diagnostic methods
How to determine that a child’s ICP has changed? First of all, you need to consult a neurologist. After a thorough questioning and examination, the doctor will prescribe instrumental studies and consultations with related specialists as necessary.
The following diagnostic techniques can be used:
- Neurosonography is an ultrasound examination of the child’s brain, which is carried out through an open fontanel. This technique is informative only until the fontanelle closes.
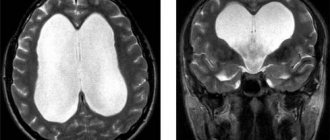
- Magnetic resonance and computed tomography - which will allow you to assess the presence and level of changes in the structures of brain tissue, determine the presence of neoplasms, and identify changes in the lumen of the pathways through which cerebrospinal fluid is excreted.
- X-ray examination - determines structural anomalies of the skull bones.
- Dopplerography is a study of the condition of the blood vessels of the brain.
- Lumbar puncture is a technique for examining cerebrospinal fluid that allows you to accurately determine changes in ICP. But before checking the indicators of this study, a full range of other procedures are prescribed, and only if they prove unsuccessful is a puncture prescribed.
- Method of direct measurement of pressure inside the skull - how ICP is measured using this method: a needle with a pressure gauge must be inserted into the baby’s head, which will allow you to obtain accurate pressure values and compare them with normal ones.
In some cases, intracranial pressure is determined in a child after a visit to an ophthalmologist, since a prolonged increase in ICP causes changes in the fundus of the eye - dilation of the lumen of the veins and narrowing of the arteries, swelling of the eye disc appears.
Causes of intracranial pressure in children
The causes of increased intracranial pressure in children can be very different, ranging from infections to head injuries and tumors. Thus, the level of ICP is influenced by the following factors:
- Injuries or hematomas of the head received during difficult childbirth.
- Hydrocephalus (water on the brain).
- Inflammatory diseases of the brain (meningitis, encephalitis).
- Adhesions between the membranes of the brain formed after surgery.
- Problems with blood clotting.
- Swelling of the brain as a result of severe intoxication (for example, drug poisoning).
- Neoplasms of benign and malignant nature.
- Hemorrhages and head injuries received in early childhood (falling from a height, etc.).
- Early overgrowth of the fontanelle (up to a year).
- Intrauterine infections.
- Acute hypoxia (for example, during fetal development).
- Congenital anomalies in the structure of brain structures.
The causes of intracranial pressure in older children are explained by cardiovascular disorders and pathologies of the muscular system.
A temporary increase in ICP can occur when:
- Severe stress accompanied by crying.
- Physical fatigue.
- Sudden change of weather.
Hypertension sometimes occurs during viral infections, but the symptoms of ICP resolve when the underlying pathology is eliminated.
Complications of high ICP
If high intracranial pressure is not treated, serious consequences may develop, including:
- Violation of the child's mental state.
- Development of epilepsy.
- Deterioration of vision.
- The occurrence of ischemic or hemorrhagic strokes.
- If there is infringement of the cerebellum, then the baby’s breathing is impaired, weakness in the limbs develops, and a disorder of consciousness is possible.
- Delay in physical and mental development.
Hypertension is most often associated with adulthood. However, intracranial hypertension, or increased pressure in the brain, often affects very young children. If such a diagnosis was made to a newborn baby during a routine ultrasound of the brain, do not panic. There may only be physiological reasons for this, for example, prolonged crying during examination.
However, you shouldn’t delay consulting a pediatric neurologist either. He will determine the exact cause of the deviation and, if necessary, prescribe treatment. Pathological intracranial pressure is a serious disorder that requires constant monitoring and treatment.
Unlike adults, intracranial pressure in children is more difficult to notice and diagnose in time.
Why do children have increased intracranial pressure?
>
Intracranial pressure is more a symptom of another disease than an independent disorder. Anatomically, its cause lies in the level of cerebrospinal fluid (CSF) and its effect on parts of the brain. Liquor is constantly produced by the blood vessels of the brain and then absorbed into the blood. When this ratio is violated, then this pathology occurs.
It can appear in the womb or during childbirth:
- abnormalities of brain development, cerebrospinal fluid outflow tracts;
- intrauterine infections;
- early closure of the fontanel (normally it closes at 12-18 months);
- hydrocephalus;
- birth trauma, hematoma resulting from severe childbirth;
- acute hypoxia causing cerebral edema.
In such cases, pathology is detected during pregnancy or immediately after birth. If a disorder is detected in time, it can be corrected and gives the child the opportunity to fully grow and develop.
Pressure disorders in the brain may appear later in life due to:
- head injuries of varying severity, hemorrhage;
- tumors of any nature;
- inflammation in the brain (encephalitis, meningitis);
- bleeding disorders;
- severe intoxication causing cerebral edema (alcohol, drug, drug poisoning);
- consequences of brain surgery in the form of adhesions.
Sometimes it occurs as a temporary phenomenon in children under 2 years of age. Intracranial pressure decreases and increases within normal limits. It is caused by changes in cerebral vascular tone when:
- severe stress, prolonged crying;
- weather change;
- excessive physical activity.
Symptoms of pathology One of the main symptoms of intracranial pressure in a child is causeless crying
Symptoms in children vary depending on age. Signs of intracranial pressure in a child under 2 years of age:
- irritability, aggression, crying for no reason (especially at night), the child often screams;
- excessive drowsiness, lethargy, muscle hypotonicity;
- abnormal head proportions;
- accelerated head growth that does not meet age criteria;
- pronounced veins on the head;
- bulging of the fontanel (more details in the article: when should the fontanel close in a newborn?);
- trembling;
- Graefe's symptom (the eyes are always drooping and there is a white stripe between the upper eyelid and the pupil), which the child cannot control;
- retardation in mental and physical development;
- nausea and regurgitation after eating;
- poor weight gain due to refusal of breast or formula, because when sucking, cranial pressure normally increases, and such children begin to have severe headaches.
An older child with intracranial pressure will often complain of headaches
Older children (3-10 years old) are concerned about:
- nausea and vomiting regardless of meals;
- hormonal imbalances due to endocrine diseases, poor physical development;
- delay in speech development, aphasia (absence or impairment of speech in a child who can speak);
- large forehead;
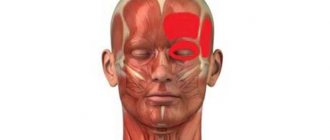
- frequent severe headaches radiating to the eyes, mainly at night;
- vision problems, double vision, when closing the eyes the child sees flashes;
- poor motor coordination;
- fatigue, inattention, irritability, apathy, drowsiness;
- Children 3-4 years of age often walk on tiptoes and suffer from attention deficit disorder.
These signs indicate that the child has problems with cranial pressure. If there is a sharp jump, then the baby experiences severe vomiting, convulsions and fainting.
This condition requires emergency medical intervention, as it can even be fatal.
Methods for diagnosing the disease
Many experts believe that in our country we have a problem of overdiagnosis of increased intracranial pressure in children. It is attributed to many benign symptoms: chin trembling, frequent crying, poor weight gain, anxiety, etc. Such phenomena can be caused by completely different reasons, for example, a lack of breast milk or colic. A pediatric neurologist, but not a pediatrician, identifies such a disorder and makes a diagnosis.
The diagnosis of true cranial hypertension depends on the age of the child, the severity of the disease and its suspected cause:
- Measuring the head circumference of a newborn. At the clinic, the pediatrician does this for children in their first year of life at every appointment. A deviation from the norm may give the first suspicion of disorders in the brain area.
- Ophthalmoscopy is an examination of the fundus of the eye by an ophthalmologist. Intracranial hypertension manifests itself by the presence of dilated veins, spasmed vessels or swelling of the optic nerve.
- Neurosonography - ultrasound of the brain. It is used in diagnostics of newborn babies (for all children it is carried out at the age of 1, 3, 6 months). For older children whose fontanelle has already closed, abnormalities can be checked using magnetic resonance imaging or computed tomography.
Ultrasound examination of the brain in an infant
- Dopplerography. Allows you to evaluate blood flow in the vessels of the brain and the presence of blockages.
- The most reliable way is a spinal puncture. It is used rarely, in particularly severe cases. A needle is inserted into the ventricles of the brain or the spinal canal, and the presence of increased intracranial pressure is determined by the way the cerebrospinal fluid flows out. The study is carried out only in a hospital setting.
- If a child is hospitalized, his intracranial pressure can be measured with a special catheter, which provides readings on a monitor. This procedure is performed only in intensive care units and intensive care units.
- In newborns, intracranial pressure disturbance is determined by the pulsation of the fontanelle on the crown of the head using a Ladd monitor.
- Additionally, an x-ray of the skull bones is prescribed. An enhanced vascular pattern, divergence of interosseous sutures, etc. may be noticeable on it.
In childhood, it is important to carry out the required diagnostics on time and constantly. This will not allow you to miss the development of complications and disorders, especially during puberty.
Methods for treating increased intracranial pressure
Treatment methods and the choice of drugs will be decided by a neurologist or neurosurgeon depending on the diagnosis, the severity of the disorder, its cause and the age of the baby. Therapy is aimed at curing the underlying disease - the root cause of the pathology.
In some cases, the child is only taken under observation and registered if intracranial pressure does not interfere with his normal life and growth. Sometimes serious drug therapy or even surgery is required. Such cases are treated only in special medical centers.
Medicines
To normalize intracranial pressure, the following groups of drugs are used:
- Diuretics - Triampur, Furosemide, Acetazolamide. Remove excess fluid from the body, including cerebrospinal fluid.
- Nootropic drugs - Piracetam, Cavinton, Pantogam, Nicotinic acid (instructions for using Pantogam tablets for children). Improves blood supply and nutrition of brain cells.
- Neuroprotectors - Glycine, Nevrohel (how to give “Glycine” to newborns: Komarovsky’s advice). Increases the performance of brain cells and calms the nervous system.
- Antibiotics - Penicillin, Ceftriaxone. If the cause of the pathology is identified, narrow-spectrum drugs are prescribed; if not, broad-spectrum drugs are prescribed. They eliminate neuroinfection.
- Sedatives to normalize the baby’s mental state and improve the functions of the nervous system.
Traditional medicine
Traditional medicine can be used with the permission of the attending physician and only as an accompanying treatment. For intracranial hypertension it is advised:
- take orally an infusion of mulberry, hawthorn, valerian, mint or lingonberry leaves;
- drink birch sap;
- make head compresses with peppermint;
- rub lavender essential oil into temples;
- wash your hair with camphor oil;
- take baths with string, birch or bay leaves, clover or linden blossom.
Baths with string and other sedative herbs have a positive effect on intracranial pressure. Other methods
In addition to drug treatment, the doctor will prescribe:
- Exercise therapy with adequate load;
- massage of the collar area;
- physiotherapy (electrophoresis, magnetotherapy);
- following a special diet with limited salt, fried, smoked, fatty foods;
- some sports, such as swimming;
- acupuncture;
- homeopathy;
- visiting an osteopath (after his manipulations, fluids, including cerebrospinal fluid, circulate well in the patient’s body);
- manual therapy;
- microcurrent reflexology is a new way to treat increased intracranial pressure, in which the brain is exposed to electrical impulses;
- Spa treatment.
On the recommendation of a doctor, the child may be prescribed massage treatments for the collar area.
In serious cases, they resort to shunting, that is, draining excess cerebrospinal fluid (for example, with hydrocephalus). Tumors and some brain injuries require surgery.
Consequences for a child with high ICP
A constant increase in intracranial pressure leads to damage to the blood vessels of the brain and disruption of its blood supply. A positive prognosis is possible with timely diagnosis and adequate drug therapy. Such children are subsequently successfully treated and do not lag behind their peers in development either in physical or mental indicators.
Advanced, severe cases lead to such serious complications as:
- stroke;
- mental disorders;
- hydrocephalus (how is hydrocephalus of the brain treated in a child?);
- epilepsy;
- paralysis, paresis;
- coordination disorders;
- visual impairment, sometimes blindness;
- speech disorder (aphasia);
- retardation in physical and mental development;
- weakness in arms and legs;
- breathing disorder.
Lack of proper treatment is fraught with disorders of physical and mental development
The list of complications is impressive. If increased intracranial pressure is not diagnosed in time, it can lead to disability in the child. In some cases, there is even death.
Lifestyle recommendations
It is very important for a child with intracranial pressure to properly organize their lifestyle to prevent deterioration of the condition:
- observe the drinking regime, do not drink more than allowed by the doctor;
- provide adequate nutrition, intake of vitamins (Alphabet, Complivit);
- physical activity will be useful, but in moderation;
- hardening procedures;
- avoid strong psycho-emotional shocks and high mental stress at school;
- create a favorable, trusting, calm environment at home;
- provide access to fresh air - ventilate the room often, walk more;
- Spend as little time as possible at the computer or watching TV;
- for aphasia and other speech disorders, regularly visit a speech therapist;
- ensure a full night's sleep (at least 8 hours), add daytime sleep.
Increased intracranial pressure in a child is a pathology quite common in the practice of any pediatrician. Unfortunately, in almost 50% of cases, the diagnosis is made without taking into account the real severity of the manifestations and the possible danger to the baby’s health.
In some cases, the cause of a short-term change in intracranial pressure (ICP) may be a banal infection or a change in weather conditions - this condition is not dangerous and does not require specific therapy.
The reasons why intracranial pressure in a child increases or decreases significantly over a long period of time are very serious and may require constant medical supervision and even surgical intervention.
Symptoms
Symptoms of ICP may vary slightly in children of different ages. Thus, intracranial pressure in a child under 2 years of age is characterized by the following signs:
- The baby often cries for no apparent reason (especially at night).
- The child suffers from excessive sleepiness and lethargy, and sometimes seems irritable and aggressive.
- There is accelerated growth of the head, causing it to acquire abnormal proportions (it appears large compared to the body).
- Pronounced veins appear on the head.
- The child periodically trembles and has convulsions.
- The baby is lagging behind in physical or mental development.
- The child often feels sick after eating.
- There is poor weight gain (because the baby often refuses food).
- You may notice protrusion of the fontanelle.
- There is increased sensitivity to pain.
- The baby may have strabismus and other defects on the face and head.
In children over 3 years of age, ICP can be recognized by the following symptoms:
- Large forehead, uncharacteristic for a child of this age category.
- Periodic attacks of nausea and vomiting (regardless of meals).
- The presence of endocrine diseases and, as a result, hormonal imbalance.
- Delay in physical and speech development (for example, the child pronounces words poorly or may have no speech at all).
- The child often complains of severe headaches.
- Problems with vision are observed (including double vision).
- Attention deficit disorder, as well as fatigue, drowsiness and irritability.
When there is a sharp jump in cranial pressure, the child experiences convulsions, severe vomiting, and sometimes it ends in fainting. In such cases, emergency medical attention is required.
Symptoms in children over 3 years of age
Intracranial pressure in a child whose fontanelle has already closed has other symptoms. In preschoolers and children of primary school age, its manifestation can be considered inattention, retardation in mental and physical development, and difficulty remembering new information. Such children, as a rule, have poor and uneven handwriting.
The main symptoms of ICP in a child of this age:
- Big forehead.
- Poorly developed speech.
- Visual impairment, double vision, spots or flashes before the eyes, pain in the eye area.
- Closed eyes.
- Increased fatigue.
A detailed story about the pathology will be given to you by a wonderful specialist - a pediatrician, candidate of medical sciences, author of popular books and television programs dedicated to children's health, Evgeniy Olegovich Komarovsky:
- Frequent whims.
- Frequent headaches, which mainly occur closer to the night.
- General weakness.
- Poor coordination of movements.
- Frequent vomiting. After another vomiting, no relief is observed. This type of vomiting differs from that which appears after food poisoning.
At the same time, the baby’s well-being worsens in the evening.
How to measure intracranial pressure in children?
You can measure intracranial pressure in a child through a spinal puncture in a hospital setting (this cannot be done at home, since there are no devices that can measure intracranial pressure as simply as, for example, with a tonometer in the case of blood pressure). A spinal puncture to measure ICP is performed extremely rarely, since the procedure is fraught with serious complications. To do this, special equipment is inserted into the child’s lumbar spinal canal and the necessary measurements are taken.
There are other complex methods for measuring ICP that require craniotomy. But they are carried out only in cases where the question of life and death arises.
Treatment of ICP in infants
Treatment of intracranial pressure in infants can be aimed both at eliminating excess or replenishing the lack of cerebrospinal fluid in the cranium, and at eliminating the causes that provoke this problem.
The choice of one direction or another will depend on the cause of ICP in the child.
For example, if the problem is caused by a malignant tumor or anatomical disorders, then there is a reason to correct not the consequence, but the cause of the metabolic disorder (often, surgically).
But if, for example, the baby is suffering as a result of hypoxia, then it is enough to take measures that will ease the discomfort and promote normal circulation of the cerebrospinal fluid.
More details about treatment methods:
- surgical intervention: used in the most severe cases, when there is certain interference in the skull for the normal flow of cerebrospinal fluid;
- drugs that lower ICP (diuretics are usually prescribed: asparkam, diacarb, triamur);
- vitamins that help improve cerebral circulation;
- sedatives;
- massage;
- physiotherapy (a swimming pool is often prescribed);
- homeopathy;
- Doctors also strongly recommend frequent emotional contact with the baby, regular walks in the fresh air, breastfeeding, and maintaining a sleep schedule.
Advice: do not be afraid of drug treatment. The sooner you start it, the faster you will relieve your child of pain, and the lower the risk of possible developmental complications. Drugs are prescribed only those that are approved for this age category.
The course of treatment is selected by the doctor. Do not try to independently treat your baby or simply choose traditional medicine. You may harm your child.
Treatment of intracranial pressure with medications
To normalize intracranial pressure, the following groups of medications are used:
- Nootropic drugs - stimulate mental activity and normalize blood circulation. These include Pantogam, Piracetam, Cavinton and other drugs.
- Diuretics - remove excess fluid from the body (including cerebrospinal fluid). These include Furosemide, Triampur, Diakarb, Veroshpiron, etc.
- Antibiotics - used to fight infectious diseases caused by bacteria, viruses, fungi and protozoa. These include Ceftriaxone, Penicillin, Azithromycin, Amoxiclav, etc.
- Neuroprotectors - calm the nervous system, protect brain cells from various damages, prevent their death and improve their functioning. Among them, the most effective are Glycine, Nervohel, etc.
- Sedatives - normalize the child’s mental state, restore the functions of the nervous system (Persen, Afobazol, etc.).
Giving a child any medications without the consent of the attending physician is strictly not recommended (since the drug can aggravate the baby’s condition). The doctor will select the required dosage and prescribe a course of therapy.
Diagnostics
Methods for examining the cranial cavity if pathology is suspected are:
- Ultrasound of the brain - neurosonography. Using this method, the macrostructure of the substance of the nervous system organ, liquor spaces are examined, and echogenicity is measured.
- Doppler studies reveal abnormalities in the blood supply to the blood vessels, as well as the presence of blockages.
- Axial computed tomography is a picture of the brain from different angles. For this method, thin beams of rays are used. CT scan reveals pathological dilatations in the ventricles.
- Resonance tomography is a method of studying the cranium using magnetic fields and radio waves. This method does not use radiation ions. When using MRI, pathologies are detected in brain tissue, the volume and stage of expansion of the cerebrospinal fluid space, as well as areas of tissue compaction are determined.
- Lumbar puncture. A needle is used to penetrate between the vertebrae and into the spinal cord. A sample of cerebrospinal fluid is taken for examination.
- X-ray of the skull. Determines defects in the structure of bone structures, as well as suture dehiscence.
- To examine the fundus, ophthalmoscopy is used, which reveals congestion of discs in the orbits.
Treatment with folk remedies
In addition to drug therapy or as independent treatment, you can use time-tested folk remedies. Here are some effective recipes:
- Lavender decoction - 1 tbsp. l. dried herb, pour 2 cups of boiling water, let it brew for an hour, strain and give the child 1 tbsp. l. 1 time per day before meals. Course of treatment: 30 days.
- Compresses with camphor oil - medical alcohol is mixed with camphor oil (1:1). A cotton swab is moistened with the resulting mixture and lubricated with gentle gentle movements, the child’s scalp is wrapped in polyethylene and a warm cap is put on top. The procedure is recommended to be done at night for three weeks.
- Birch sap - to normalize increased intracranial pressure, the baby should be given 1-2 glasses of sap per day (depending on age). Therapy is carried out for 4 months. To improve the taste, you can add 1 tsp to birch sap. flower honey.
If a child experiences an allergic reaction to any product (skin rash, itching, etc.), treatment should be stopped and a doctor should be consulted.
What is blood pressure, types
Blood pressure is the process of compression of the walls of capillaries, arteries, veins, which appears during the movement of blood fluid.
Depends on:
- Age characteristics of a person. Ideal values for adults are considered to be 130-110/70-80 mmHg. In young children, this indicator is not constant and varies in relation to the age of the children.
- Paula. For men and women, the medical characteristics are almost the same. In the period from 6 to 17 years of age, girls have higher blood pressure values than boys.
- The presence of stressful situations. These processes are characterized by strong heartbeat, rapid pulse, and fever. Blood pressure automatically rises. Constant exposure to critical moments may result in persistent hypertension.
- Chronic pathologies of the endocrine, cardiovascular, nervous systems, kidneys.
- Having excess body weight. Obesity is often accompanied by severe hypertension.
- Time of day. In the morning, blood pressure is lower than before going to bed.
- Carrying out physiological exercises.
Blood pressure in children.
The norm depends on the age and condition of the child. Blood pressure is characterized by two components:
- upper (systolic) – shows the blood pressure at the greatest compression of the heart muscle;
- lower (diastolic) - reports the movement of blood fluid when the heart is most relaxed.
Possible complications
If you ignore the symptoms of the disease, complications may arise such as:
- Mental and physical abnormalities.
- Stroke.
- Epilepsy.
- Problems with vision (up to complete loss).
- Muscle weakness.
- Respiratory system disorders.
- Vegetovascular dystonia.
If the disease is controlled (visit a doctor regularly, undergo treatment, etc.), complications can be avoided, keeping the child’s health normal.
Methods for measuring blood pressure
Digital data is measured:
- Direct (invasive) method - performed in a hospital setting if constant monitoring of blood circulation and the patient’s condition is necessary. Consists of inserting a catheter needle into the lumen of the radial artery. The cord of the device is connected to a pressure gauge that records the data.
- Indirect (non-invasive) methods : Auditory - the most common. Pressure is measured with a hand-held tonometer with a cuff filled with air. When the valve opens, oxygen leaves the device, making it possible to listen to heart beats at specific dial readings.
- Oscillometric - measuring blood pressure using a mechanical device. Does not require manual air supply. The indicators are displayed on an electronic display.
Rules for measuring blood pressure:
- It is carried out in a lying or sitting position, with the patient completely relaxed, in complete silence.
- One hour before measurements, you should avoid eating food.
- It is carried out on both hands. The upper limb should be placed next to the heart with the palm facing up.
- Oxygen is pumped into the cuff smoothly, without sudden movements.
- The sleeves of clothing should not squeeze the arm and arteries.