Fetal hypoxia - this diagnosis is increasingly being made to expectant mothers. In essence, it is not a disease, but a state of acute lack of oxygen in a child. When fasting is in its early stages, it is quite simple to eliminate it, and it will not entail any significant consequences. If measures are not taken on time, complications will be unavoidable. The consequences of fetal hypoxia for a child are very serious.
With a severe lack of oxygen, the baby loses its vitality. It is impossible to remain in this state for a long time: either the child will become seriously ill, or hypoxia will lead to death. It is worth considering that the disease is not so difficult to recognize. If a woman listens carefully to herself and her baby, she will be able to prevent the development of this disease and change the situation. The expectant mother should experience only positive emotions.
There is no need to take care of a child to the point of paranoia, endlessly looking for signs of hypoxia in the behavior of the fetus and in your condition. To avoid this, it is enough to know the causes and risk factors for the disease. By reading the article further, you can find out all the necessary information.
Diagnosis of hypoxia
Children diagnosed with perinatal posthypoxic damage to the central nervous system are observed by a neurologist for 2 years. After this period, the diagnosis is removed or changed to a more complex one (cerebral palsy, hydrocephalus, etc.).
Methods for diagnosing post-hypoxic state:
- Ultrasound of the brain showing the anatomy of the nervous system
- electroencephalogram (EEG) characterizes neuronal function
- Dopplerography of cerebral vessels characterizes the functions of cerebral vessels, with what speed and symmetry they work and how well they deliver oxygen to the brain.
- MRI is extremely rarely performed on children in the first 2 years, as anesthesia is required for this study.
Ultrasound of the brain reveals the following post-hypoxic changes:
- Cysts (appear after 10-14 days after hypoxia).
- Deformation of the gyri and sulci of the brain.
- Periventricular leukomalacia - necrosis of brain cells around the ventricles of the brain, is an extremely unpleasant symptom in terms of prognosis, often ending in hydrocephalus and cerebral palsy.
- An increase in the size of the cerebral ventricles, interhemispheric fissure and other liquor-containing spaces.
The frequency of studies in children who have suffered hypoxia is once every 3 months to a year and once every 6 months. in the second year of life.
The Apgar score is not the only criterion for hypoxia. For example, in a fetus, in response to a lack of oxygen, the rectal sphincter opens and meconium enters the amniotic fluid, causing it to turn green. Oxygen starvation may also be indicated by the condition of the placenta (premature aging, abnormal development of blood vessels, etc.). Sometimes such children are born with a high Apgar score, but hypoxia still occurs.
The brain of children in the first 2 years of life is very plastic and gladly accepts all treatment methods, responds quickly and produces excellent results. Recently, osteopathic treatment has taken a well-deserved place in the treatment program for children who have suffered from hypoxia.
What are the consequences of hypoxia?
The consequences of oxygen starvation can be of varying degrees of complexity, it all depends on how long the baby suffered without oxygen. Doctors evaluate the health of a newborn using a special Apgar scale. If immediately after birth the baby’s health is assessed at 4-6 points, and after 10 minutes from 8 to 10, then you can expect consequences of moderate severity. If the score is lower, the consequences of the disease will be more complex.
Babies who have suffered from a lack of oxygen in the future may face such problems as:
- Developmental, mental, physical retardation
- Speech delays
- Hyperactivity
- Neurological disorders
When a developing organism lacks oxygen, the brain is the first to suffer. If the doctor nevertheless makes this unpleasant diagnosis to a newborn baby, he is immediately prescribed treatment and registered with a neurologist. Parents of such children need to know that perhaps in the future they will need the help of a speech therapist or child psychologist.
Hypoxia is not a death sentence for a child; despite all its seriousness, hypoxia does not put an end to the development of the fetus. In most cases, babies are born healthy and develop just like their peers. The only thing that may indicate hypoxia is a bluish tint to the skin of a newborn, but after a week the baby’s skin will acquire a natural color for children.
In order for your baby to be born healthy, you must monitor your health, take all prescribed medications, give up bad habits, and stay away from suspicious people who may suffer from infectious diseases. By fulfilling such simple requirements, you will reduce to a minimum the possibility of diagnosing your pathology.
Consequences of hypoxia
Previously, we looked at the causes and diagnosis of post-hypoxic conditions and agreed that children born with an Apgar score of 7 and below are considered to have suffered hypoxia. This group also includes children with an umbilical cord entanglement, premature babies, etc.
It is extremely important to regularly examine such children over time at certain age periods: 1 month, 3 months, 6 months, 9 months, 1 year. The purpose of examination and observation is to prevent and reduce chronic diseases and reduce the degree of long-term consequences. About 83% of children who have suffered hypoxia have central nervous system lesions in various manifestations and combinations.
There are 3 periods during the course of the disease:
- acute period up to 1 month.
- recovery period from 2 months. up to 2 years
- outcome of the disease - after 2 years.
The most common symptoms of central nervous system damage in the acute and recovery period. Sometimes these symptoms appear in combination with each other:
- Syndrome of increased neuro-reflex excitability.
- The child is very restless, negative to examination, sleep disturbances, muscle tone disorders, etc. are noted.
- Hypertensive-hydrocephalic syndrome.
- Due to the increase in the amount of fluid in the spaces of the brain, intracranial pressure increases. It is characterized by a rapid rate of increase in head circumference, a large fontanel, restless behavior, and frequent regurgitation.
- Vegetative-visceral syndrome.
- Dysfunction of the gastrointestinal tract, frequent regurgitation, frequent bowel movements or constipation, bloating. Dysregulation of vascular tone, which manifests itself as uneven skin coloring (marbling). Irregular breathing and heart rhythm.
- CNS depression syndrome.
- Decreased motor activity, decreased muscle tone, weakened sucking and swallowing reflexes.
- Pyramid syndrome.
It is expressed by hypertnus of the calf muscles, stiffness in the ankle joints, walking on tiptoes, delayed speech development, as well as motor development.
If you have these symptoms, you should not wait for a scheduled examination; it is better to immediately contact a neurologist and osteopath for early diagnosis and treatment.
Fetal hypoxia
When the fetus is in the mother's womb, it cannot breathe on its own. The child's lungs are still in an unexpanded state and filled with fluid, so air cannot enter them and actively circulate. But oxygen is necessary for the life of the fetus. The fetus receives all the necessary components through the mother’s blood; the most important element of this is the placenta. If the process of feeding the fetus with all the necessary substances is disrupted, then starvation occurs. If the fetus does not consume enough oxygen, hypoxia occurs. Fetal hypoxia can be caused by various reasons. Fetal hypoxia can occur during pregnancy, and can also occur directly during childbirth.
Classification of fetal hypoxia
Fetal hypoxia is divided into two degrees of severity: moderate fetal hypoxia and severe fetal hypoxia.
Depending on the causes and speed of development of the disease, acute and chronic fetal hypoxia are distinguished.
Acute hypoxia
Acute hypoxia usually develops during childbirth. In acute hypoxia, disorders of vital organs develop. The diagnosis of acute hypoxia can only be made by medical specialists based on heartbeat disturbances and recorded excessive or weakened motor activity of the baby. The diagnosis is confirmed by research using special medical equipment.
Chronic
Chronic hypoxia develops with postmaturity and infection of the fetus, with toxicosis of the woman and extragenital diseases, as well as with a conflict between the Rh factor of the blood of mother and child. Chronic hypoxia develops slowly and step by step, the child gets used to and adapts to the lack of oxygen. Doctors can diagnose chronic hypoxia by conducting research using special methods and functional tests.
In 1952, at the Congress of Anesthesiologists, a document was adopted that assessed the severity of fetal hypoxia. It describes the Virginia Apgar scale, which specifies 5 factors by which to assess the condition of the fetus. Each factor is scored from one to three points. The baby is assessed on the Virginia Apgar scale twice: as soon as he is born and five minutes after.
How does the assessment work?
The first factor is breathing activity. It is necessary to understand the nature of breathing (slow, active, normal or screaming).
The second factor is the presence of reflexes. It is necessary to check the response to the catheter in the nasal cavity (crying, coughing, sneezing, dissatisfaction, no reaction).
The third factor is the state of muscle tone. It is necessary to bend the baby’s arms and legs, find out the nature of the movement of the limbs (active, normal, weak).
The fourth factor is the condition of the skin. It is necessary to check the color of the skin of the child’s body and limbs (pink, white, bluish).
The fifth factor is heartbeat activity. It is necessary to measure the heartbeat (more than one hundred beats per minute, less than one hundred beats per minute, no heartbeat).
A healthy, active child usually receives 8-10 points. But the majority of children are rated at 7-8 points due to cyanosis of the extremities and inactive muscle tone. During the second study, after five minutes, if the child adapts well, the scores increase to 8-10. Moderate hypoxia is diagnosed at 4-7 points. And if a child has only 0-3 points on the Virginia Apgar scale, then this is severe hypoxia or asphyxia.
Complications of fetal hypoxia
If a woman ate a balanced diet, led a healthy lifestyle, was observed by a doctor and followed all recommendations, then there should be no complications from hypoxia. But in cases where fetal hypoxia is severe, this poses a danger to the further mental and physical development of the child. The consequences of fetal hypoxia can cause multiple diseases in the child. In severe forms of hypoxia, acidosis develops and redox reactions change. As a result of such complications, tissues do not accept oxygen, but only absorb carbon dioxide. With serious complications of hypoxia, the intrauterine fetus may begin to breathe, as a result of which amniotic fluid and blood enter the baby’s lungs.
Prevention of fetal hypoxia
To prevent the development of fetal hypoxia, the expectant mother should give up all bad habits long before pregnancy. Pregnant women need to spend a lot of time outdoors, eat a balanced diet and do special exercises. A pregnant woman should not be nervous, worried, tense or overworked. Particular attention should be paid to the prevention of iron deficiency anemia, because it is the main cause of oxygen deficiency disorders.
A routine examination by a qualified doctor and carrying out all the necessary diagnostic tests can prevent the disease and prevent the development of severe hypoxia. You must always remember that any emotions and sensations of a pregnant woman will certainly be passed on to the baby. A woman’s healthy lifestyle is beneficial not only to herself, but also to her future offspring.
Treatment of hypoxia
Post-hypoxic damage to the central nervous system requires staged treatment after resuscitation measures (if they were necessary), the recovery period begins, the following is applied:
- Exercise therapy
- massage
- physiotherapeutic treatment
- drug therapy (nootropic drugs, vascular drugs, vitamins)
- hydrokinesitherapy (swimming)
- methods such as bobat therapy and vojta therapy are increasingly being used, which are especially useful for children with impaired muscle tone
- osteopathy.
Causes of hypoxia in a child
The most common factor is intrauterine hypoxia of a chronic nature associated with impaired placental blood flow. In addition, the reasons are:
- premature or prolonged labor
- umbilical cord compression during childbirth
- chronic maternal disease
- multiple pregnancy
- malposition
- premature placental abruption
- mother's age is less than 16 or more than 40 years
- alcohol abuse and smoking
- previous abortions.
Osteopathic treatment of hypoxia during childbirth
Osteopathic treatment rightfully occupies one of the leading places in the rehabilitation of children who have suffered from hypoxia. Balancing the bones of the skull allows you to relieve tension from the dura mater and the cerebral hemispheres, thereby ensuring the most complete functioning of the central nervous system.
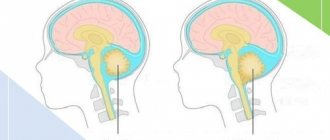
Osteopathic techniques allow for drainage of the venous sinuses, as a result of which cerebrospinal fluid resorption is improved and intracranial pressure is normalized. Freeing the cervical spine and eliminating torticollis promotes adequate blood supply to the brain.
Early osteopathic treatment in the first year of life allows children not only to keep up with their peers in development, but sometimes even to develop ahead of schedule. It is very important to carry out this treatment from the first months of life, as this will help get rid of long-term clinical pathological symptoms. Osteopathy sessions are conducted for children starting from the first month of life. Osteopathic treatment, creating optimal functioning of the central nervous system, stops the process of post-hypoxic changes in neurons, thereby somehow reprogramming the brain for full development.
There is no need to be afraid of hypoxia; you need to take the entire range of measures for rehabilitation after it. Moreover, modern medicine gives us many tools for this.
Advantages of treating the consequences of labor hypoxia in our Neonatus Sanus medical center
Our clinic of osteopathy and neurology on Vasilyevsky Island “Neonatus Sanus” - health from birth, has extensive practical experience in the prevention and treatment of newborns, infants and infants.
We know how and love to work with young children!
Our clinic employs experienced osteopathic doctors and neurologists. A lot of attention is paid to each child in order to understand the child, accurately assess his condition, give recommendations to parents and, if necessary, carry out effective osteopathic treatment.
In our center you can get the best examination, treatment and recommendations from leading specialists in St. Petersburg.
Breathing exercises
During pregnancy, the growing uterus moves upward all the organs of the abdominal cavity, including the diaphragm, which limits its movement and, consequently, the volume of inhalation. This leads to a lack of oxygen in the body, which can worsen as pregnancy progresses. This is why it is so important for a pregnant woman to practice proper breathing every day in order to prevent chronic and acute fetal hypoxia, because the need for oxygen increases significantly towards the end of pregnancy, and during childbirth an unforeseen situation may arise in which the ability to breathe correctly can play a big role in saving life and child health.
Clinical example of treatment of the consequences of hypoxia in our osteopathic center
Reviews from our patients about the treatment of hypoxia
Katyusha was born from her first pregnancy at 40 weeks. The condition after birth was severe due to asphyxia. Apgar score 1/4 point. After 3 hours, due to respiratory failure and convulsions, she was transferred to the intensive care unit. Artificial ventilation and brain hypothermia were performed. The result of severe brain hypoxia was the diagnosis: Cerebral Palsy, right-sided spastic hemiparesis. At the age of 1 year 6 months she first appeared in our center. The main complaint was delayed motor development; independent walking appeared only at 1 year and 4 months. When walking, she experienced great problems due to high muscle hypertonicity along the entire right side, strabismus and restless behavior were noted. After the treatment, the girl’s muscle tone was almost normalized, her gait was as close as possible to physiological, the girl has excellent speech development, she enjoys going to kindergarten and communicating with her peers. We thank the parents for providing the video material.
Watch the video review at the link