The mood of patients with schizophrenia largely depends on the nature of productive symptoms and affective symptoms (decrease or increase in mood).
A person with schizophrenia may experience mood disorders in the form of depressive or manioform symptoms. In a depressive state, characteristic depressive symptoms are observed with low mood, depression, and lack of desire to do the usual work or have fun and joy. Only here, in addition to possible depressive psychotic symptoms with ideas of self-abasement and self-blame, there must be characteristic symptoms of the schizophrenic process (hallucinations, delusions of relationships, influence, persecution, etc.).
Manioform symptoms are manifested by a picture of the opposite pole with elevated mood, accelerated tempo of thinking, verbosity, and increased motor activity. And in this state, in addition to possible psychotic symptoms characteristic of pure mania, which manifests itself in the form of delusional ideas of grandeur and overestimation of one’s own capabilities, there must also be specific symptoms characteristic of schizophrenia (hallucinations, delusional ideas of relationship, influence, persecution, etc.).
With a continuous form of schizophrenia, the mood may depend on the nature of the productive (hallucinatory-paranoid) symptoms and is normalized as it is reduced (weakened) during the treatment of the patient.
In the episodic remitting course of schizophrenia (paroxysmal, recurrent, circular, periodic schizophrenia according to various classifications) in the structure of psychosis (exacerbation) predominantly mood disorders (depressive or manioform symptoms) are observed, and to a much lesser extent - hallucinatory-paranoid symptoms and another - dissociative ( characteristic of the schizophrenic process).
In the episodic course of schizophrenia with progressive development of the defect (fur coat-like, paroxysmal-progressive schizophrenia according to various classifications), mood disturbances and characteristic schizophrenic symptoms are observed in approximately half.
Mood disorders (depressive or manioform symptoms) with episodic remitting course and episodic course of schizophrenia with progressive development of the defect require specific treatment with antidepressants, as in the corresponding phases of bipolar affective disorder or endogenous depression.
It should be taken into account that the more pronounced affective changes in a patient, the better his prognosis and the less a specific schizophrenic defect develops (flattening of affect, development of indifference, apathy, difficulties in communication), which is an unfavorable sign of the course of this mental illness.
The state of indifference, low mood and lack of desire to do the usual work, which is observed with depression in patients with schizophrenia, differs from the apathetic manifestations that are characteristic of emotional burnout (an increase in the schizophrenic defect).
Disorders of the emotional sphere in schizophrenia: the formation of apathy - a personality defect
A decrease in the amplitude of emotions during apathy is a manifestation of a schizophrenic defect. Patients with a mental illness such as schizophrenia lose the ability to respond adequately to bad news or, conversely, to enjoy something. It seems that they are indifferent to everything, nothing evokes an emotional response in them. And how sad it is, but this is actually so... Over time, you can notice that such patients stop taking care of themselves and their loved ones. They cannot empathize with them, they lose their sense of empathy (sensitivity, empathy and responsiveness). This has a negative effect on the person’s environment and leads to misunderstanding by others.
Diagnosis of disorders
For subsequent therapy of disorders and its effectiveness, timely diagnosis of the child’s emotional development and its disorders is very important. There are many special methods and tests that assess the development and psychological state of a child, taking into account his age characteristics.
Diagnosis of preschool children includes:
- Diagnosis of anxiety level and its assessment;
- Study of psycho-emotional state;
- Luscher color test;
- Studying the child’s self-esteem and personality traits;
- Study of the development of volitional qualities.
Seeking psychological help is necessary if a child experiences certain difficulties in learning, communicating with peers, behavior, or has certain phobias.
Parents should also pay attention if the child experiences any emotional experiences, feelings, and also if his condition is characterized as depressed.
Emotional state disturbances in schizophrenia: stages of apathy formation
- First stage: there is a decrease in the amplitude and severity of emotions. This happens while all emotions remain adequate.
- The second stage is a narrowing of the range of emotions, when there is a loss of strong, expressed, higher, both positive and negative emotions:
- the mother or child falls ill, and the patient does not sympathize and does not react as before,
- there is no profession, it’s the same as if I’m sitting at home and not earning money, etc. Emotions remain at the average everyday level - wash, cook, make a bicycle, etc.
- , distorted emotions appear false ones - parathymia : ridiculous laughter, causeless anger, aggression towards a person one likes, etc. At the same time, some minor events lead to sharp emotional outbursts that look clearly paradoxical, contrary to the order of things or moral standards For example, a patient with schizophrenia may be indifferent to the serious illness of his mother, but the death of a house plant will lead him to deep feelings. Patients cannot explain why they do this, and sometimes they can even be critical of parathymia.
- Subsequently, a loss of emotions is observed, when for a short time (5 minutes or 1 - 2 hours) there is a complete absence of emotions in the patient (both positive and negative). One can bring up such a tragic example from medical practice, when a son with schizophrenia gouged out his father’s eyes so that he would not eat his cucumbers (“so that the father would not see the cucumbers”). And when the loss of emotions passed, the patient developed psychogenic depression over what he had done.
- The final stage of development of apathy is the absence of emotions and complete indifference to the environment. Only primitive drives are preserved - sex, hunger, pain.
Emotional decline in schizophrenia - the formation of apathy - can be compared to the breakdown of a piano.
First, the sound becomes dimmer, then high and low tones stop sounding, then false sounds appear, then some keys stop playing - they fall out, and the last extreme - the piano stops sounding at all.
You can notice how the development of the disease leads to the fact that a patient with schizophrenia becomes more and more emotionally cold, he no longer likes his former interests, he breaks off contacts with friends and relatives, quits his job, his favorite activity and moves into the world of painful experiences. He may spend months or years in his room (or even in bed), detached from everyone, not paying attention to what is happening.
The energy and initiative of patients decreases. It is difficult to force them to do something, even if it concerns professional activities. The daily routine also changes: a person can be active at night and sleep during the day. Or wake up early in the morning, at three or four o'clock.
Over time, apathetic changes reach such a degree that hygiene skills are lost. The patient stops taking care of himself, changing clothes, and his appearance stops bothering him.
Main problems
Depending on the degree of disturbance of the emotional-volitional sphere, the child becomes irritable, lethargic or generative. Parents should notice their child's problems as soon as they appear. Any disease, before settling in the body, manifests itself in symptoms. At this stage, it is necessary to determine the extent of the child’s problems and prescribe treatment. What is the classification of persons with disorders of the emotional-volitional sphere?
- Aggressiveness. Persons behave inappropriately, bully others and take pleasure in tears and humiliation of a weaker opponent. Even children who behave aggressively will never bully someone who is stronger than them. They will logically reason that a harmless creature will not be able to fight back, and therefore can be humiliated.
- Slow reaction. Children cannot immediately understand what the problem is. For example, they may feel hungry, but will not make any effort to ask for food or to get food themselves.
- Disinhibited reaction. The second point in the classification of persons with disorders of the emotional-volitional sphere are people who cannot control their emotions. If they cry, they cry too loudly; if they laugh, they do so for an unnaturally long time.
- Excessive anxiety. Downtrodden children of overactive parents become quiet. They are afraid to talk about their desires and problems. They fail to attract attention due to their weakness of character.
Help for emotional disturbances (apathy) in schizophrenia
That is why one of the main conditions for the patient’s rehabilitation in everyday life and society in the early stages (when you can still help!) is support among loved ones. A person with schizophrenia should be involved in housework, even if the help is minimal. Wash the dishes, make the bed, clean up after yourself, brush your teeth - these seemingly banal things are simply necessary. It is also very important to help him get a job (after the exacerbation ends), first with at least a part-time schedule, and also to encourage him in every possible way to communicate with old friends and acquaintances, and to help him find new ones. After all, if you distance yourself from a patient with schizophrenia or do everything for him, the defect will only worsen.
The main thing with these actions is not to provoke the patient into aggression. It is important here to grasp the fine line between total control and friendly support. So try your best and be patient! The patient can be brought back to life!
We constantly detect plagiarism on our materials without providing a clickable follow link to them. In this case, without warning, we turn to Google DMCA , which leads to pessimization of the plagiarist. On the contrary, we welcome the popularization of our materials, but with the obligatory active follow link to this page psyhosoma.com/emocionalnye-narusheniya-pri-shizofrenii/ .
External manifestation
Disturbances in the development of the emotional-volitional sphere of a child can be determined by the child’s behavior.
- Strong dependence on parents. A child who, at five years old, cannot trust the people around him causes a strange reaction. The baby hides behind his mother’s skirt all the time and tries to close himself off from the world. Normal childhood embarrassment is one thing. And something completely different – distrust, unsociability and intractability.
- Lack of communication. A child who is neglected in the family will feel lonely. The child will not be able to form relationships normally, since the parents will convince the child that he is stupid, crooked and unworthy of love. The loneliness that such a child will exude will be strongly felt.
- Aggression. Children who lack attention or who want to relieve tension may not withdraw into themselves, but, on the contrary, behave too relaxed. Such children will not restrain their emotions and will try with all their might to attract attention to their person.
Gestalt therapy
Such therapy allows the child to expand his feelings, or rather develop them. The specialist’s task is to transform the child’s inadequate reactions into ones that will be acceptable to society. How does the transformation process work? The specialist identifies a problem, such as excessive aggression, which the child expresses by beating his opponent. The doctor should tell the child that his way of solving the problem is ineffective, and in return offer more civilized methods of expressing emotions. For example, a verbal form of expressing your dissatisfaction. Then you need to play out the situation with the child. After your child loses his temper, you should remind him of the recent conversation and ask him to express his feelings in words.
The child's anger should decrease over time as the task will seem too difficult at first. Over time, the baby should get used to the new strategy for expressing aggression. And in order for the learned material to be better understood, the child needs to be constantly reminded of the lesson completed. And it is desirable that the child sees similar methods of emotional reaction in adults. For example, when mom and dad quarrel, they should not shout at each other, but calmly and measuredly express dissatisfaction with one or another offense of their spouse.
Behavioral therapy
This type of therapy takes place in the form of a game. The child is offered a simulated situation, and he must show how he will behave in it. The game is aimed at developing in the baby those feelings that any normal individual should experience in a given situation. After conducting a game situation to reinforce the material, the presenter must once again explain what exactly was being modeled and how the patient should behave in such a situation. You should definitely get feedback from your child. The child must explain the material he has learned. Moreover, you need to get the child not only to tell you how to behave in a situation, but also to explain why such behavior will be considered acceptable.
Such therapies should be carried out once a week. And for the remaining 7 days, the child must consolidate the material received in class. Since the child will have little interest in his own development, parents should monitor the child’s behavior. And if the child does something differently from the training, mom or dad must repeat the recently completed lesson with their child.
Cognitive behavioral psychotherapy
Persons with emotional-volitional disorders who have reached adulthood also need help, just like children. But it will be difficult to change a teenager with the help of a game. Therefore, cognitive behavioral therapy should be used. What is its essence?
A person is given a situation and several ways to develop it. The teenager must tell what awaits the person who has gone through each of the fictional paths. In this way, the person will better master the situation and understand the essence of the consequences of this or that behavior. In a similar way, you can instill responsibility in teenagers and explain the price with your promise. The formation of new behavioral habits will not happen immediately. It’s one thing to theoretically lose a situation, and quite another to change your character.
The older a person is, the less chance he has of making internal changes. Therefore, the specialist who conducts classes with a teenager must positively reinforce the patient’s successes and focus on any positive changes. People who suffer from a disorder of the emotional-volitional sphere are subject to self-criticism and it is very important for them to hear approving words from adults and respected people.
Non-psychotic mental disorders are observed in almost all children and adolescents suffering from resistant forms of epilepsy. They are not only a factor indicating the progression of the epileptic process, but also one of the main reasons for social maladaptation and subsequent disability of patients. As a rule, these are persistent personality changes, manifested in disorders of the intellectual-mnestic sphere (30-70%) [2, 6, 8, 11] and affective disorders [2, 5, 9, 10]. The share of epileptic psychoses in the structure of epilepsy in adolescence is small [1].
The formation of non-psychotic epileptic personality changes in children and adolescents suffering from forms of epilepsy resistant to drug therapy is associated both with the impact of the epileptic process itself and with the nature and severity of organic changes in the brain that accompany the disease. Many authors [6, 7, 13] attribute one or another role in the occurrence of mental changes in epilepsy to long-term use of antiepileptic drugs (AEDs) and even associate epileptic personality changes almost exclusively with the influence of constantly taken medications, in particular barbiturates. The development of mental disorders in patients with epilepsy requires additional prescription of psychotropic and nootropic drugs along with anticonvulsants, which in turn increases the “load” on internal organs (liver, kidneys, gastrointestinal tract, cardiovascular system) and worsens the compliance of patients.
In the last decade, anticonvulsants with not only normothimic (carbamazepine, valproic acid) but also nootropic effects (lamotrigine, topiramate, levetiracetam) have become widely used in the treatment of epilepsy. The use of these drugs, unlike the previous generation of anticonvulsants (barbiturates, hydantoins, benzodiazepines), improves the cognitive functions of patients suffering from epilepsy, as well as stabilizes their mood and emotions even in the absence of complete clinical-encephalographic remission, without additional inclusion of nootropics and mood stabilizers in therapy [ 3, 4, 12].
The purpose of this study is to study the dynamics of cognitive and emotional-volitional disorders in children and adolescents suffering from resistant forms of epilepsy during treatment with levetiracetam.
Material and methods
We examined 76 children and adolescents, 45 (59.2%) boys and 31 (40.8%) girls, aged from 6 to 17 years, treated in the department for the treatment of mental disorders in young people of the St. Petersburg Research Psychoneurological Institute them. V.M. Bekhterev, suffering from focal and generalized forms of epilepsy with concomitant non-psychotic mental disorders resistant to drug therapy. The average age of children and adolescents was 14.31±0.3 years, the duration of epilepsy was 9.17±0.45 years.
There were no restrictions on the inclusion of patients in the study.
All children were examined over time before starting levetiracetam therapy and after 1 year of using the drug. All children received various anticonvulsant therapy before coming to the institute. Levetiracetam was prescribed at a daily dose of 20 mg/kg body weight, divided into 2 doses (10 mg/kg 2 times a day), with a dose increase of 20 mg/kg every 2 weeks until the recommended daily dose was reached - 60 mg/kg body weight body (30 mg/kg body weight 2 times a day), in combinations (for all forms) with both the second and third drug, with lamotrigine at a dose of 3-5 mg/kg - 15 (19.7%) patients, with carbamazepine at a dose of 10-30 mg/kg - 12 (15.2%) children, with valproate at a dose of 30-50 mg/kg - 21 (27.6%) patients, with topiramate at a dose of 3-5 mg/kg - 26 (34.2%) patients, with valproate and topiramate (in the same doses) - 2 (2.6%) patients. When adding levetiracetam to other drugs, the principle of titration was maintained.
When examining patients, psychopathological and experimental psychological methods were used. Using the clinical-psychopathological method, the form of epilepsy and the characteristics of attacks were studied in detail in the clinical picture of the disease.
The majority of the study sample - 57 (75%) people - were patients with focal forms of epilepsy; according to the etiology of the disease, among focal epilepsies, symptomatic forms were predominantly distinguished (46.1%), among generalized epilepsies - cryptogenic (15.8%). There were no patients with idiopathic forms of epilepsy among those examined. Complex partial seizures were observed in 45 (78.9%) of 57 patients with focal forms, complex (simple and complex) - in 12 (21.1%). Secondary generalized seizures were observed in 49 (85.9%) patients suffering from focal drug-resistant forms of epilepsy. According to the localization of the epileptic focus, patients with focal forms were distributed as follows: 11 (19.3%) - with localization of the epileptic focus in the frontal region, 5 (8.8%) - in the temporal region, 39 (68.4%) - in the frontal region. temporal and 2 (3.5%) - in other areas (occipital, parietal). According to the nature of the attacks, children suffering from a generalized form of epilepsy were divided as follows: atypical absence seizures were observed in 8 (42.1%) of 19 children, myoclonus - in 6 (31.6%), astatic seizures - in 5 (26.3%) ). The presence of grand mal seizures was noted in 13 (69.2%) children suffering from generalized drug-resistant forms of epilepsy.
Using the clinical-psychopathological method, disorders in the intellectual-mnestic and emotional-volitional spheres of patients were also studied in detail. A decrease in cognitive functions was recorded in all 76 (100%) patients, mnestic-aphasic disorders - in 36 (47.4%), personality changes in the form of bradypsychia, bradykinesia - in 29 (38.2%), dysphoric states - in 31 ( 40.8%), manifestations of depression - in 14 (18.4%), anxiety was observed in 23 (30.3%) patients. Manifestations of cerebrasthenic syndrome were observed in 56 (73.7%) patients. Hysteroform neurosis-like disorders were identified in 6 (7.9%) subjects. At the same time, various psychopathological manifestations concomitant with epilepsy could occur in the same patient.
For the convenience of clinical assessment of the severity of psychopathological symptoms, a visual analog scale was used - Comprehensive Psychopathological Rating Scale (CPRS). The assessment was carried out in points from 1 to 3 for each cluster, where 3 points is a description of the extreme severity of the symptom; 2 points - description of subjective experience or behavior that should always be considered pathological in certain circumstances; 1 point - a description that can be applied to pathological deviations from the individual norm, but can also relate to a variant of the norm in a certain group of people; 0 points – absence of a specific symptom. For all clusters included in the scale, subscale levels 0, 1, 2 and 3 are operationally defined. The severity of the disease was assessed using the Clinical Global Impression (CGI) scale in the range from 1 to 7 points, with an increase in score according to the increase in the severity of the disease.
The intellectual level of children was assessed using the Wechsler method (children's version). Intellectual development corresponded to the norm in 24 (31.6%) children, a decrease in intelligence to a borderline level was observed in 44 (57.9%), a gross decrease in intelligence (to the level of retardation and imbecility) was recorded in 8 (10.5%) children.
The results obtained during the study were processed using SPSS statistical packages using standard methods of mathematical and statistical analysis (comparison of means using Student's t-test).
Results and discussion
When using levetiracetam for 1 year, 59 (77.8%) patients experienced a reduction in attacks, which is presented in Table. 1
.
During treatment with levetiracetam, 62 (81.6%) patients with epilepsy showed marked improvements in the intellectual-mnestic sphere, which is presented in Table. 2
.
During 1 year of levetiracetam therapy, 48 (63.2%) patients also experienced changes in the emotional-volitional sphere, presented in Table. 3
.
From the table 2 and 3
It follows that after 1 year of therapy with levetiracetam in children and adolescents with resistant forms of epilepsy, even in the absence of clinical remission of attacks, there was a significant improvement in attention, memory, speech and motor activity, as well as a decrease in tension. There was a tendency to improve mood, which contributed to social adaptation and improved quality of life of patients, and also improved patient compliance. However, it should be noted that at the level of trends, manifestations of verbal and physical aggression also persisted, and at times intensified; patients became capricious, excitable, and sometimes uncontrollable in behavior. This behavior was typical for 7 patients receiving levetiracetam in combination with valproate for focal forms of epilepsy, and 2 patients with a generalized form receiving levetiracetam in combination with carbamazepine. The changes in behavior were so pronounced that they required a revision of therapy. In a number of similar cases, replacing valproates with first-choice drugs in the treatment of focal forms (carbamazepine, topiramate, lamotrigine) led to a complete reduction of disorders in the emotional-volitional sphere. Thus, the results of this study confirm the existing literature data on the high effectiveness of levetiracetam not only as an anticonvulsant drug, but also as a drug with a good nootropic effect. Levetiracetam also has an effect on the emotional-volitional sphere of children and adolescents, reducing stress levels and improving mood, but sometimes the activating effect of the drug entails increased manifestations of aggression and affective instability.
The study revealed changes in the overall severity of the disease after 1 year of levetiracetam therapy, which is presented in Table. 4
.
It shows that when assessed using the scales used, the overall severity of the condition associated with the underlying disease significantly decreased.
The dynamics of changes in cognitive functions and affective disorders in a patient with a resistant form of epilepsy who received levetiracetam for 1 year is most clearly presented in the example of one of the patients.
Patient A
., 14 years old. Upon admission, the patient complained of daily nightly complex partial attacks of a tonic nature with vocalization, rolling of the eyes, loss of consciousness, lasting up to 1 minute, with a frequency of 2-3 times per night at different times, speech impairment after the attack; episodes of aggressive behavior, emotional lability, mental retardation.
Heredity is not burdened with neuropsychiatric diseases. Born from the first pregnancy, which occurred against the background of emotional stress and anemia in the mother, the first urgent labor with stimulation. Birth weight 3.5 kg, height 52 cm, Apgar score 7/8 points, cried immediately, discharged on time. Early development by age. Diseases suffered include acute respiratory infections (ARI), iron deficiency anemia, and bilateral sinusitis.
At the age of 3 years, febrile convulsions appeared for the first time against the background of acute respiratory infections; no AED treatment was performed. A repeated attack of febrile seizures at the age of 6 years, after which, without connection with high temperature, generalized tonic-clonic seizures began to occur lasting 3-5 minutes up to 18 times a day, with wetting and falling asleep after the attack. Since 2005, attacks have been observed only at night, lasting up to 2 minutes, 2-3 times per night. Against the background of the attacks, regression of previously acquired skills was noted. From the age of 7, as the disease progressed, there was a deterioration in memory, attention, slowness of activity, motor clumsiness, and a subsequent decrease in intellectual abilities.
Mental status: consciousness is not clouded. Correctly oriented in the environment and time according to age and intelligence. Available to contact, but somewhat closed. Answers questions selectively, monosyllabically, with a delay. Smiles when talking. Emotionally labile, there are episodes of aggression and irritability (according to the mother). There are no deceptions of perception, delusional ideas or suicidal thoughts. Intellectual-mnestic function is reduced.
Neurologically: the face is symmetrical, the pupils are D=S, the reaction to light is preserved. Hypotonia of the shoulder girdle muscles with tension in the neck muscles. Muscle strength is 4-5 points, tendon reflexes are symmetrical, somewhat animated.
Somatically: without pathology.
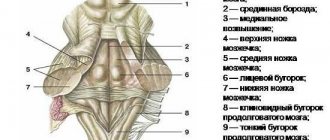
On MRI: a picture of minor arachnoid changes of a liquorocystic nature. Moderate decrease in blood flow in the intracranial segment of the right vertebral artery. Option for the development of the circle of Willis. Transcranial Dopplerography: vascular angiodystonia. Dynamic EEG without visible changes - significantly pronounced diffuse changes in the bioelectrical activity of the brain in the form of high irritation of the entire surface of the cortex with signs of organic changes at both the cortical and subcortical levels, predominantly of a residual nature, with a predominance in leads from the left hemisphere. A focus of paroxysmal activity in the deep parts of the left frontotemporal region with a tendency to generalization. Video-EEG sleep monitoring: generalized bilaterally synchronous discharges of acute-slow wave complexes throughout almost the entire recording. Psychologist's conclusion: the structure of intelligence is uneven, HI=74, VI=79, NI=72. Signs of organic brain damage.
Diagnosis: focal cryptogenic epilepsy with decreased cognitive abilities, resistance to drug therapy (ICD-10 category F 02.8*2).
Considering the features of therapy in this case, it can be noted that the patient had previously received finlepsin, depakine, convulex, suxilep in various combinations with a short-term effect. After the diagnosis of cryptogenic frontal lobe epilepsy in June 2003, Depakine was prescribed at a dose of 1800 mg per day, Lamictal 100 mg, ⅔ tablets 2 times a day, subsequently the dose of Depakine was increased to 2700 mg per day. During this therapy, myoclonic seizures lasting up to several seconds appeared, and daily generalized tonic-clonic seizures persisted. Subsequently, radedorm was added to the treatment regimen, which stopped nocturnal attacks, but provoked behavioral disorders in the form of irritability, emotional lability, and affective instability. The drug was discontinued. Clonazepam was prescribed, the attacks were absent for 2 weeks, then they recurred. The introduction of lamotrigine into therapy led to a reduction in daytime astatic attacks and myoclonus. But nocturnal complex partial seizures persisted, sometimes with secondary generalization. When benzonal, diphenine, and relanium are added to therapy, severe intoxication and development of status epilepticus are observed, which can only be stopped with the help of resuscitation measures. The introduction of topiramate up to 200 mg per day into therapy has no effect. The introduction of convalis led to the resumption of generalized tonic-clonic seizures. With increasing doses of topiramate and valproate, attacks become more severe and more frequent. Reducing the dosage of lamotrigine or valproate provoked an increase in seizures until the development of complex partial seizure status. When Keppra was added to therapy with Convulex (900 mg per day) and Lamictal (100 mg per day), the patient showed positive dynamics: first, the duration and then the frequency of attacks decreased; after 1 month of therapy (Keppra dose 1500 mg per day), short attacks of tonic tension without loss of consciousness once every 7-10 days. Subsequent dose increases did not increase the effectiveness of therapy. After 1 year of therapy with Keppra at the same dosage, short (several seconds) simple partial nocturnal seizures persist, and paroxysmal activity in the form of generalized acute-slow wave complexes remains on the EEG, with an emphasis over the frontotemporal regions of the left hemisphere. Despite this, the patient’s behavior improved, he began to attend classes at school, communicate with peers, his memory improved, he became more focused, he was less tired, and he mastered the correctional school program.
Thus, levetiracetam, an anticonvulsant with a complex mechanism of action, is a highly effective drug in the treatment of both focal and generalized resistant forms of epilepsy and concomitant mental disorders. Even with incomplete clinical remission of attacks, levetiracetam causes significantly positive changes in the intellectual-mnestic sphere, improving performance, attention processes, memory, and effectively affects speech pathology, which allows you to avoid additional use of nootropics, which often intensify and/or provoke the development of convulsive attacks. In the case of manifestations of aggression or increased affective instability, even with clinical remission of attacks, adjustment of drug therapy is required taking into account the form of epilepsy. Levetiracetam, when taken for a long time, causes positive changes in the cognitive and emotional-volitional spheres, improves the social adaptation of children and adolescents suffering from epilepsy, increases the compliance of patients and contributes to a better implementation of rehabilitation measures.
Methods
Emotional-volitional disturbances in the personality sphere can be subject to correction. What methods do specialists resort to to correct what parents have wrongly instilled in their child?
- Game therapy. With the help of the game, the rules of adequate behavior in the group are explained to the child. The child develops new neural connections that help transform what he sees in the game and transfer examples to life situations.
- Art therapy. With the help of a drawing you can learn a lot about a child’s personality. A creative work will show the specialist how the baby feels in the garden, in the family and in this world. Drawing helps you relax and feel confident. Other types of art work the same way: modeling, embroidery, design.
- Psychoanalysis. An experienced psychotherapist can help a child reconsider his views on familiar things. The doctor will tell the baby what is good and what is bad. The specialist will act in two ways: suggestion and persuasion.
- Trainings. This method of influence involves working with a group of children who have a common problem. The guys will jointly review their habits and form new ones based on old ones.