One third of the total mass of the human cerebral hemispheres is in the frontal lobes. If blood circulation is disrupted in this particular part of the brain, then, first of all, all cognitive (cognitive) processes suffer.
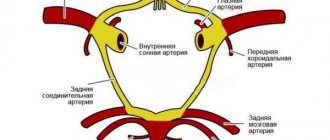
The main causes of impaired blood flow in the vessels of the frontal lobes of the brain are exacerbations of hypertension, atherosclerosis, some congenital pathological diseases of blood vessels, poor blood clotting, and a tendency to thrombus formation. All this leads to a stroke. Depending on its mechanism of action, a stroke can be ischemic or hemorrhagic. Further, in turn, the stroke leads to the development of frontal syndrome. It is important to note that stroke is not the only cause of this disease. However, symptoms may
Symptoms of frontal stroke
Frontal stroke most often manifests itself in the form of general cerebral symptoms:
- A person experiences acute pain in the front of the head, nausea and vomiting.
- Dizziness leads to loss of consciousness.
- A high body temperature may rise.
Specific symptoms of frontal stroke:
- Rudimentary reflexes appear: sucking, grasping, searching (in the case of extensive damage to the frontal lobes);
- A person loses the ability to control his own actions;
- The sense of self-awareness is lost;
- There are motor and speech disorders;
- The ability for abstract thinking and planning is lost;
- The functions of memory, attention and will of a person are impaired;
- The victim is unable to focus on anything, cannot solve complex problems, make logical connections, form concepts, etc.
Symptoms may also vary depending on the location of the damage. In case of a stroke on the left side of the frontal part of the brain, a person's verbal behavior is impaired. He is unable to quickly remember and name familiar objects, and cannot speak at a fast pace. If the damage occurs on the right side of the frontal part of the brain, then nonverbal fluency is impaired.
It is believed that lesions in the prefrontal region of the brain lead to disruption of a person’s executive functions. A person who has suffered a stroke of the frontal lobes may retain some motor functions, intelligence and perception, but at the same time the behavior and the very personality of the victim are distorted. Often such consequences are unnoticeable while the patient is still being treated in a medical facility. But over time, these deviations will become more and more apparent. The doctor’s task is to collect a complete history of the onset and course of the disease in order to subsequently correctly prescribe the necessary therapy.
Summary based on gender and age
Medical statistics show that older people and females are most susceptible to stroke.
Among women
More often, hemorrhagic stroke develops, as well as micro-strokes, which often go unnoticed. As a rule, women have a harder time surviving a stroke and are more susceptible to the consequences. As a result of a stroke, women are much more likely to develop:
- memory loss;
- decreased intelligence;
- lack of speech.
In men
As a consequence of a stroke, men often:
- paralysis of the limbs and facial asymmetry occurs;
- coordination of movements is impaired;
- hearing loss;
- convulsions appear.
In older people
Stroke and its consequences are much more severe in older people. More often it occurs:
- cerebral edema;
- complete paralysis;
- lack of breathing.
In young people
Micro-strokes are typical for this category of patients. The consequences usually take the form of:
- nervous system disorders;
- depression;
- acute course of hypertension;
- in some cases, speech and memory disorders.
In children and adolescents
A stroke is fraught with consequences such as:
- speech problems;
- paralysis of one side of the body;
- developmental delay;
- epilepsy attacks.
In newborns
In addition to the above, the child has a high probability of developing cerebral palsy.
Consequences of frontal stroke
The consequences of a frontal stroke can be expressed in the form of frontal syndrome. There are two types of this disease: abulic and disinhibited.
The abulic type leads to the loss of a person’s ability to think creatively, initiative, and curiosity. Often there is a disturbance in the emotional background, manifested in the form of apathy and indifference.
The disinhibited type of frontal syndrome is directly opposite to the abulic type - impulsive behavior occurs, a person loses common sense in their actions, and is unable to foresee the consequences of their actions. Memory and thinking are completely preserved. Thus, a person is able to characterize his actions in possible situations, but in practice he will act completely inadequately and unpredictably.
An acute loss of nutrition to an area of brain tissue due to spasm or blockage of an artery is called an ischemic stroke. It accounts for approximately 80% of all vascular lesions of the brain and is often the cause of death and disability in patients. Focal and cerebral manifestations persist for a long time, and treatment and rehabilitation continue for more than a year.
Read in this article
Extensive stroke and its features
Signs of destruction of brain tissue over a large area are the following:
- long period of loss of consciousness;
- cerebral coma with complete lack of response to stimuli;
- loss of vision;
- intense headache and dazedness;
- convulsions;
- fever, chills and hot flashes;
- nausea and severe vomiting;
- persistent disturbances of movement in the limbs and sensitivity;
- pronounced changes in tendon reflexes;
- memory loss.
Extensive hemispheric ischemic stroke
Causes and risk factors for ischemic stroke
The main pathological conditions in which the risk of acute cerebral ischemia increases include:
- transient disturbances of cerebral blood flow due to narrowing of the lumen of the carotid artery;
- hypertension and symptomatic hypertension;
- smoking;
- high levels of cholesterol, triglycerides, homocysteine in the blood;
- age over 60 years;
- atrial fibrillation;
- diabetes;
- atherosclerosis of the coronary arteries with myocardial ischemia;
- chronic alcoholism and drug addiction;
- previous stroke;
- obesity;
- low physical activity;
- taking hormonal contraceptives;
- migraine attacks;
- burdened heredity;
- acute and chronic stress.
Less commonly, strokes occur against the background of vasculitis, antiphospholipid syndrome, meningitis, Moya moya disease, blood diseases, compression of the vertebral artery in the cervical spine, and congenital vascular anomalies.
Read more about drug treatment for stroke here.
Disability
Do they give it to everyone?
Despite the fact that mainly older people are susceptible to such a complex disease as stroke , recently young people have also been affected (read about the consequences of a stroke for older people here).
The current legislation of the Russian Federation does not establish any limitation in which cases disability is granted, whether it is applicable to everyone who has suffered a stroke or not, while a citizen applying for such status must have appropriate medical indications and be able to confirm them with documents.
Can they refuse to receive it?
The answer to this question is simple - they can. Even if the patient has serious medical conditions, but his condition is not critical and does not correspond to the least degree of disability, then experts may refuse to obtain disability.
The right to receive this status is available to patients who cannot live fully and carry out work activities due to incomplete restoration of impaired brain functions.
How soon can I apply?
Many are also interested in how long it takes to apply for disability and when it is granted. The status of “disabled” and disability group are assigned to a citizen only after passing the medical examination , which can only be referred to by the attending physician.
In this case, the patient can declare a desire to register a disability both while being treated in a hospital and after being discharged from a medical institution (read about how long people stay in the hospital and intensive care unit with a stroke here).
Stages and order of registration
In any case - while in the hospital or after discharge - registration of disability will take some time, as well as additional examinations.
A citizen who has suffered a stroke must go through several stages:
- Contact your attending neurologist while in hospital or after discharge to a medical institution at the registration mass. At the appointment, you should inform about health problems that appeared after the disease, and about the desire to receive a disability group. If the patient is bedridden, then his relative will have to agree on inpatient examinations.
The doctor must make an appropriate entry in the medical record, as well as give directions for tests and consultations with specialized specialists, which must subsequently be entered into the patient’s medical record.You will need the results of tests such as: general blood and urine analysis, biochemical blood test, REG of brain vessels, ECG, EEG, CT/MRI of the brain, X-ray of the skull (in some cases of the cervical spine), Doppler ultrasound, ultrasound of blood vessels and others . The opinions of the following highly specialized doctors are also required - psychiatrist, ophthalmologist, ENT specialist, surgeon, endocrinologist, cardiologist.
- When all the examinations have been completed and the results have been received, the attending physician must write a prescribed form for a referral to the ITU commission.
- The patient then fills out an application asking to set a date and time for the examination. On the appointed day, the citizen comes with the necessary package of documents and makes a decision on the assignment or refusal to assign a disability.
- If the patient does not agree with the decision, he can appeal it first to the main ITU bureau, and then, if necessary, in court.
Who is eligible for which group?
In accordance with the consequences of a person who has suffered a cerebral stroke - how much they limit his ability to work and quality of life, ITU members assign him one of the existing disability groups.
- I – As a result of a stroke, there are severe disorders of the musculoskeletal system. The patient cannot lead a normal life and has lost the ability to care for himself independently - he needs constant care.
- II – The person has persistent dysfunctions of the body. At the same time, he is disabled, but can take care of himself.
- III – Functional disorders in the body are persistent, but moderate and can recover over time. The person is able to work, but is prohibited from certain types of work (you can see the list of recommendations and prohibitions here).
If the patient is a minor, then he will be assigned the status of “disabled child.”
How to get a?
To obtain a disability, the patient needs to know how it is formalized and follow the rules established by the legislation of the Russian Federation, which regulate the list of necessary documents, the rules for conducting medical examination for various patients and the amount of payments.
Required documents
A citizen applying for disability will have to prepare and submit the following documents to the ITU::
- Issued referral to ITU.
- Personal application for examination.
- Civil passport (original and copy).
- The patient’s medical record with all available certificates, conclusions, and test results. Moreover, if a person received something from a private institution, then they also need to be provided to the commission.
- A copy of the work record book, a certificate of income and a reference from the place of work, if the person is working.
- Open sick leave, certificate of occupational diseases or occupational injuries, if available.
Medical and social examination
On the appointed day, the patient comes to the office with a prepared package of documents and provides them to the members of the commission .
Their number is usually three people. But in some cases, if the presence of highly specialized specialists is necessary, their number can be increased. They carefully study all documents, analyze social, labor and living conditions, if necessary, conduct inspections and assess its compliance with the following criteria:
- self-service option;
- ability to navigate in space and coordination;
- the degree of his dependence on others;
- ability to adequately communicate and control behavior.
Also, during the examination, a record of the protocol is required.
After all this, the commission voices either a positive or negative decision, which is formalized in the form of an act. If a citizen receives the status of “disabled,” he is given a certificate indicating the disability group and an individual rehabilitation program.
With this certificate, you must contact the social security authorities, where they will arrange the appropriate benefits, and the pension fund, where they will determine the amount of the pension benefit.
For pensioners
The specifics of registering disability for pensioners who have suffered a stroke are slightly different, but only at the stage when the medical examination has already been completed and the necessary certificate has been received.
It is with this that a citizen of retirement age must first contact the Pension Fund of the Russian Federation. After reviewing it, you will need to obtain a certificate and apply for a small pension supplement. At the same time , the pensioner can continue working if his state of health allows , because This does not affect the amount of the benefit.
Pension amount
A citizen who has received a certificate from the ITU and has completed documents with the Pension Fund can count on help from the state.
- Social pension, which is paid to non-working disabled people and disabled children permanently residing in the country who provide a passport, a certificate from the ITU and an application. According to Art. 18 Federal Law No. 166 and indexation from 2021 by 4%, payments are (in rubles):
- I – 12577;
- II – 5240;
- III – 4454.
- A labor (insurance) pension is paid to working disabled citizens who provide a work record book, an ITU certificate and an application. Its size directly depends on the salary: I – 100%, II – 90%, III – 50% and in 2021 increased by 4.1%.
- Monthly social payments, according to Art. 28.1 Federal Law No. 181, also indexed in 2021 by 5.5% are (in rubles):
- I – 3552;
- II – 2667;
- III – 2133.
For bedridden patients
Patients who have suffered a stroke and have lost the ability to move independently can also apply for disability . But first they need to draw up and notarize a power of attorney for their representative, who will prepare all the necessary documentation.
Also, to undergo an examination, a bedridden patient may be temporarily hospitalized or the commission may be invited to his home.
For children
Disability is also different for children who have had this disease . Everything is formalized in the medical institution where the treatment and rehabilitation took place, and there is no need to collect additional certificates and conclusions, and there is no need to undergo an examination by a commission.
Such children are assigned the status of “disabled since childhood” and do not need to undergo re-examination.
On our Internet portal you will find useful information about the symptoms and consequences of a stroke on the left and right side of the brain, with cerebral hemorrhage, find out why the patient sleeps a lot or suffers from insomnia, the causes and degree of coma, why the brain and limbs swell, legs hurt and convulsions.
For how long is it issued?
Many citizens are wondering: for how long will disability be issued? The answer will be as follows - the status of “disabled” in each specific case has its own period.
- Indefinite – does not require re-examination.
- Not unlimited - requires re-examination depending on the group: I - 2 times a year, II and III - 1 time a year.
- Women over 55 and men over 60 do not undergo re-examination.
Permanent disability is also issued if, after 5 years, disabled people of groups I and II have not experienced any improvement in health.
Symptoms of cerebrovascular accident
The development of acute cerebral ischemia occurs suddenly. The symptoms persist for more than a day. All signs can be divided into focal and cerebral. The first include:
- limb weakness (paresis);
- speech and vision impairment;
- facial distortion;
- difficulty swallowing;
- decreased sensitivity.
In the presence of a focus of critical ischemia in the right hemisphere, patients develop the following clinical signs:
- left-sided paralysis;
- the assessment of the size and number of parts of one’s body and surrounding objects is impaired;
- current memory is lost, but the past is clearly remembered;
- the left field of vision is absent;
- the patient does not recognize the severity of his condition;
- difficulty concentrating;
- depressive reactions alternating with goofy behavior;
- loss of behavioral inhibitions.
This disease is characterized by a variety of symptoms, an unfavorable course and a long rehabilitation period.
Patients are conscious or stunned; with severe cerebral edema, cerebral coma may develop. Impaired movement, sensitivity and a drop in muscle tone are noted on the right side of the body, speech and logical thinking suffer, and depression is characteristic. In addition, depending on the location of the blockage of the vessels that supply the brain cells, patients experience the following abnormalities:
- weakness of the tongue and facial muscles on the right;
- loss of the right field of vision, a decrease in the ability to recognize objects, up to complete blindness;
- difficulties in writing, reading, counting;
- impaired urine output;
- weakening of memory;
- decreased criticism and abnormal behavior.
Signs of cerebral infarction with damage to the anterior cerebral artery
Ischemic stroke in the territory of the anterior cerebral artery on the left is manifested by right-sided paresis of the lower limb on the right or hemiparesis with more pronounced damage to the lower limb on the right.
When the paracentral branch of the anterior cerebral artery is blocked, monoparesis of the foot on the right develops, resembling peripheral paresis. Possible manifestations include urinary retention or incontinence with reflexes of oral automatism and grasping phenomena. With left-sided localization of ischemic stroke, the left hand is affected with the formation of its apraxia.
Also characteristic are changes in the mental state with damage to the left frontal lobe in the form of a decrease in criticism and memory with the development of unmotivated behavior. All these changes are expressed during the formation of bilateral foci of cerebral infarction in the anterior cerebral artery basin.
Classification
Depending on the underlying disease, ischemic strokes are cardioembolic and atherothrombotic; according to the extent of the process, lacunar and minor strokes are divided into separate forms. The group of others includes rare and unclear causes of pathology.
If a blood clot has formed in the cavity of the left atrium or left ventricle, then with the movement of blood it can enter the bloodstream of the brain and lead to complete blockage of the artery. Patients at high risk of embolism include those with:
Occurs due to the development of atherosclerosis and blockage of the vessel by a thrombus or a detached part of a loose or ulcerated plaque. The source of such emboli can be the aortic arch, the system of brachiocephalic vessels, or intracranial large arterial branches. Most often combined with vasospasm.
This type of stroke occurs against the background of arterial hypotension. A sharp drop in blood flow to the brain can result from:
- quick change from horizontal to vertical position;
- deep dream;
- physical activity;
- intense cough;
- taking a large dose of antihypertensive drugs;
- heart attack;
- blood loss, dehydration;
- arrhythmia;
- low blood output from the left ventricle.
These factors limit cerebral blood flow and, with severe atherosclerotic changes in the arteries, can provoke acute cerebral ischemia.
It usually occurs in hypertensive patients. The typical cause is thrombosis of small arterial pathways. The lesions are located in the internal medullary capsule, subcortical nuclei and corpus callosum. It has 25 flow options, of which the most common are:
- purely motor form;
- Sensory impairment only;
- mixed (motor and sensory changes);
- speech impairment and clumsy hand;
- weakness in the limbs and dizziness.
This type occurs with vascular spasm or incomplete blockage. The signs that appear gradually disappear within 20 days from the onset of the disease. A constantly relapsing course and transition to a more extensive lesion is possible with insufficient treatment.
Rare background pathologies in ischemic stroke include increased coagulation capacity of the blood, dissection of the vascular wall, and vascular damage in systemic vasculitis. In some patients it is impossible to detect the cause, or there are too many of them, so it is difficult to identify a specific one.
Edema
Swelling of the limbs
A common phenomenon is swelling of the limbs after a stroke. This may occur due to vascular damage during an attack . A rapid and acute disturbance of blood circulation in the brain occurs. In some cases, this subsequently affects the legs and arms.
If the patient and his relatives ignore the problem of swelling of the limbs, then in most cases this will lead to a sad outcome.
Long-term congestion in the extremities, which swell, can lead to the appearance of such a dangerous disease as trophic ulcers.
The disease is very difficult to treat . Especially when the patient's blood flow is impaired. Then such ulcers have a predisposition to develop into gangrene, and subsequently into sepsis.
It is also noted that poor circulation leads to dry skin and brittle nail plates.
Swelling can occur for various reasons. Let's take a closer look at each of the possibilities.
Heart failure
It is noted that if the patient had previously had heart failure, then after the attack it will develop for the worse. The heart cannot cope with its work and it is for this reason that the fluid in the limbs stagnates. And then they start to swell.
In order to improve the condition, you need:
- try to keep the load on the heart minimal;
- get rid of swelling in the legs.
Varicose veins
With varicose veins, a characteristic picture is visible . A professional doctor, after getting to know the patient and examining him, will immediately make the correct diagnosis and prescribe the necessary therapy.
Treatment will be aimed at bringing blood circulation back to normal.
The drugs should increase the tone of the vascular walls and are aimed at preventing the formation of blood clots.
Traditionally, the medications Detralex and Phlebodia are prescribed . In some situations, the doctor may refer the patient to physiotherapeutic procedures. They are done precisely on the swollen area.
Reference ! The use of compression garments brings good results.
Thrombosis
The properties of blood can change with little physical activity. The blood becomes thick. And the speed of its movement throughout the human body decreases accordingly. Consequently, a person has a certain tendency to thrombosis.
In the first stages, medications help . In advanced situations, operations are prescribed.
Kidney diseases
Renal failure and glomerulonephritis can trigger the development of stroke. These diseases are interconnected. After an attack, diseases of the urinary system only get worse.
Under such circumstances, swelling forms not only on the legs and arms, but also on the face. In case of kidney failure, the doctor has to prescribe diuretic drugs in large dosages.
Why do paralyzed limbs swell?
After a person has suffered a stroke, one can often note the fact of swelling of paralyzed arms and legs . The problem is twofold. This occurs for reasons:
- low elasticity of blood vessels;
- the presence of poor conductivity near the walls of blood vessels;
- interference in the form of prolapsed internal organs;
- cholesterol blockage;
- compression of large vessels.
This is also why swelling can occur in a paralyzed leg. What:
- the position of the patient's legs is incorrect;
- muscle tone is impaired;
- the patient does not feel his limbs.
In such situations, an examination must be carried out and a series of tests prescribed .
Treatment
In order to return swollen arms and legs to normal in a short period of time, you need to follow some rules, which we will talk about now.
- It is recommended to reduce the amount of liquid consumed. The figure should not be more than 1.5 liters per day. This volume includes any liquid, including soups.
- A small amount of salt, equal to a maximum of 2 grams.
- It is necessary to do gymnastics and massage daily. Even if you don't want it.
- Do not stay in one position for a long period of time.
- Control the volume of urine, which should be the same compared to the liquid consumed.
Among medications, the doctor prescribes diuretics and diuretics .
You should not prescribe such drugs yourself. Improper use of diuretics can lead to large amounts of potassium leaving the body.
And this will negatively affect cardiac activity and a recurrent stroke may occur. Under such circumstances, a person can be severely paralyzed and sometimes death can occur.
Prevention
There are preventive actions that you can take to avoid such unpleasant manifestations:
- If the legs and arms are deprived of motor activity, it is best for them to be in a horizontal position.
- If the patient has been sitting for a long time, then he needs to have a foot and knee massage.
- To prevent the limbs from swelling, you should not stay in one position for a long time. It is necessary to change it at intervals.
If you carry out such manipulations, the blood flow will increase, and thereby the fluid in the tissues will decrease. The most effective way is massage .
It is also recommended to adhere to a diet. It is valuable to avoid excess salt consumption.
Prognosis for recovery
To ensure that the patient does not have problems with edema, it is necessary to constantly monitor the composition of the blood. If treatment is avoided, some of the vessels may never recover . Normalization of the condition is observed when taking vitamins and unquestioningly following the therapy prescribed by the doctor.
It is imperative to systematically massage and put stress on the limbs. Some patients believe that, on the contrary, the limbs should not be disturbed again. That is why dystrophy of the muscles of the limbs can begin.
If you follow all the rules, your body’s recovery will end in 1.5 years. The arteries and vessels will return to normal and begin to perform their functions.
Brain swelling
In some cases, the patient may experience cerebral edema . This is too dangerous a phenomenon in which fluid increases in the area around the brain. As a result, intracranial pressure begins to increase.
Causes
Factors influencing the development of this pathology can be identified:
- Improper energy metabolism in the brain. Because of this, congestion and inflammation occur. As a result, excess liquid is formed.
- Poor circulation in arteries and veins.
- Lack of oxygen and necessary substances.
- The composition of the blood changes.
- There is a change in blood plasma pressure.
Varieties of the phenomenon
There are two types of edema:
- Local . Occurs due to the formation of edema or an increase in fluid volume.
- Generalized . A reaction to the processes described above occurs.
Consequences and complications
The most common consequences that you should pay attention to:
- the person becomes drowsy and lethargic;
- disturbance in speech and coordination;
- changes in consciousness;
- coma;
- mental disorders;
- paralysis.
Treatment
Treatment is prescribed conservatively and medicinally.
Medicines are prescribed that reduce the risk of blood clots. They also use means to normalize blood composition.
In addition, antihypertensive drugs and nootropics are effectively used . Diuretics give results.
Prevention
To avoid cerebral edema after an attack, preventive measures must be taken. It is important to maintain proper nutrition. The patient's rest is of high importance. This is especially true for people who are overweight and have blood pressure problems.
Forecast for life
There may be some problems in the future .
Death of nerve tissue occurs. This in turn can cause certain body functions to stop working.
Many processes that begin in the body are irreversible. Patients may often experience a recurrence of the attack.
If you observe signs of edema in a patient, you should immediately show him to the doctor. You cannot self-medicate . The consequences may be too serious.
Degree of damage
Based on how pronounced the focal and cerebral signs of stroke are, they are divided into three categories:
| Categories | Short description |
| Easy | There are minor neurological disorders that decrease over three weeks, one of the options is a minor stroke; |
| Moderate severity | The patient is conscious, focal signs predominate, and general cerebral signs are not expressed; |
| Heavy | There are general cerebral symptoms, the patient is unconscious, severe neurological disorders, cerebral edema or displacement of brainstem structures. |
First aid before the ambulance arrives
If a person suddenly develops weakness in the limbs, impaired speech and facial expressions, severe headache, nausea and vomiting, changes in consciousness or convulsions, then the main help is to immediately call an ambulance. Before her arrival, it is necessary to provide the patient with as much air as possible. To do this, you need to place it on a horizontal surface with its head slightly raised.
Unfasten the collar, remove dentures and vomit from the mouth. If the patient is unconscious, the head should be turned to the side. It is advisable to apply cold to the head, especially on the side opposite to the paralysis of the limbs.
You should not try to give water or food to the patient, or use medications to restore blood circulation without a doctor’s recommendation.
When does cerebral edema occur?
Local swelling occurs in the area of circulatory impairment. If the brain damage is severe, and treatment is not carried out, or there are no results from the use of medications, then the following changes occur:
- regulation of vascular tone is disrupted;
- cerebral vessels dilate;
- the pressure inside the arteries and veins increases;
- The liquid part of the blood passes through the walls into the brain tissue.
Impregnation with liquid, swelling and edema of the brain lead to compression of vital centers in the confined space of the skull. Patients gradually lose consciousness, which is manifested by disorientation and lethargy. As edema increases, cerebral coma and convulsive syndrome develop, which is replaced by complete muscle atony. If edema occurs against the background of a gradual deterioration in brain nutrition, then its manifestations are as follows:
- preserved consciousness;
- Strong headache;
- nausea and vomiting;
- disorders of limb movements, impaired coordination;
- decreased vision;
- slurred speech;
- hallucinations.
Watch the video about cerebral edema:
When the brain stem is compressed due to displacement into the foramen magnum region, symptoms appear that are considered extremely life-threatening:
Signs of left-sided cerebral infarction in the carotid region
Ischemic stroke in the internal carotid artery system is caused by severe hemodynamically significant stenosis or blockage within or extracranial of the left internal carotid artery. With thrombosis in the extracranial part of the internal carotid artery on the left, patients develop hemiparesis in combination with central paresis of the tongue and facial muscles, significant sensory impairment and the formation of visual field defects on the right (the opposite side of the body is affected).
With left-sided damage to the internal carotid artery, opticopyramidal syndrome may develop, which is characterized by decreased vision or complete blindness on the side of the blockage (left) in combination with hemiparesis of the right side of the body.
Ischemic cerebral stroke with intracranial blockage of the internal carotid artery on the left is manifested by right-sided hemiplegia and hemianesthesia in combination with severe cerebral symptoms: severe headache, vomiting, significant impairment of consciousness and/or psychomotor agitation and the formation of a secondary brainstem syndrome.
Treatment of ischemic stroke
The earlier drug treatment is started, the greater the results can be achieved. In the hospital, constant monitoring of blood circulation indicators, the balance of blood electrolytes, respiration, and cerebrospinal fluid pressure is carried out. The following groups of drugs are used:
- oxygen inhalations;
- antiplatelet agents (Clopidogrel, Aspirin), low molecular weight heparins (Fraxiparin, Cibor) and thrombolytics in the first three hours (Actilyse);
- neuroprotectors (Cerebrolysin, Actovegin, Somazina);
- calcium antagonists (Nimotop);
- to prevent cerebral edema (magnesium sulfate, Diacarb, Lysine aescinate);
- antioxidants and metabolic stimulants (Mexidol, Cytochrome);
- stimulants of motor activity (Neuromidin);
- for muscle spasms and convulsions (Mydocalm, Phenazepam).
What happens when damaged
Right-sided ischemic stroke occurs due to the death of neurons as a result of ischemia or oxygen deprivation. Blood clots can:
- Form directly in the cerebral arteries due to the deposition of cholesterol on their inner walls. These deposits are called atherosclerotic plaques. The blood clot blocks normal blood flow, leaving an area of the right hemisphere damaged without oxygen and nutrients. If the blockage of blood flow is not cleared within 3-5 hours, the area of the brain dies. It is these processes that cause the neurological consequences of a stroke.
- Form in other organs and enter the brain through the bloodstream. The clearest example is atrial fibrillation or atrial fibrillation. Chaotically contracting atria lead to the formation of blood clots in the heart cavity. The clots then travel through the bloodstream to the brain, causing vascular occlusion and stroke.
A damage zone is formed, which causes clinical manifestations and consequences. Only timely treatment, aimed at dissolving and removing blood clots, as well as neuroprotection, helps to avoid massive damage. Late initiation of treatment greatly worsens the prognosis for recovery.
Recovery and rehabilitation
The first stage of rehabilitation treatment is carried out while the patient is on strict bed rest. At this time, therapeutic exercises begin in the form of passive movements, active flexion and extension in the joints of the unaffected side of the body. Breathing exercises are a mandatory element to prevent decreased ventilation in the lungs. After stabilization of the main hemodynamic parameters, massage is prescribed.
After the appearance of independent movements and sensitivity, the rehabilitation plan includes physical therapy and sessions with a speech therapist to improve speech. At later stages, active restoration of walking, fine movements and self-care is carried out, and special simulators are used.
Neurological manifestations
The symptoms of two types of stroke - ischemic and hemorrhagic (hemorrhage) can be distinguished by a neurologist, but the signs of stroke and heart attack can be differentiated without having a higher medical education. In order not to get confused in such situations and, if possible, to be useful in emergency cases, the reader can try to learn how to identify these conditions by studying the distinctive signs of a stroke.
All consequences of right-sided cerebrovascular accidents can be divided into several groups:
- Physical activity disorders, that is, restrictions in the motor sphere
- Changes in the senses: vision
- Defects of the cognitive (cognitive) sphere
- Emotional problems
It is not necessary for one patient to necessarily have symptoms from all groups. It all depends on the extent of the damage and the mood for recovery.
Physical problems
Right-sided cerebrovascular accident causes motor problems in the left half of the summer. Moreover, not only the limbs, but also the muscles of the torso and face can be involved.
The following post-stroke disorders in the motor sphere are distinguished:
- Paresis is severe muscle weakness and the inability to perform usual actions. In other words, paresis is incomplete paralysis. As a result of a stroke, the normal transmission of nerve impulses from the brain to the muscles is interrupted. The degree of muscle weakening may vary. There are monoparesis - weakening of one arm or leg, and hemiparesis - disorders of two arms and legs, i.e. half of the body.
- Paralysis is a complete lack of motor activity. Often, not only the limbs are involved, but also the muscles of the trunk, which leaves the person bedridden.
- Poor coordination of movements, inability to hold the body in space.
- Tendency to move too quickly, impulsively, and not always adequately.
- Increased muscle tone (spasticity), which is often accompanied by pain and worsens the prognosis.
Recovery from disorders such as hemiparesis and paralysis is possible. However, such severe consequences require long-term and methodically correct rehabilitation. Such patients require additional care during the recovery period - severe weakness or immobility makes it impossible to care for themselves.
Sense organs
Circulatory disorders in the right hemisphere of the brain cause problems with “left-sided vision” - that is, a person has no perception of the left fields of vision. Such patients may leave food on the left side of the plate uneaten, because they simply do not perceive it. Some patients do not distinguish the right side of an object from the left, or the top from the bottom.
Since the right hemisphere is responsible for basic thought and communication processes, this group includes the most numerous and common consequences of brain stroke.
- Problems with attention and concentration – a patient with a right-sided stroke has difficulty concentrating on a task, focusing on what he sees. Such people cannot carry on a productive conversation, because they often do not catch what the interlocutor is saying. The prognosis for such disorders is ambiguous and requires long-term rehabilitation.
- Memory impairment – patients find it difficult to remember previously known information or recall any new data, even the simplest ones.
- Problems with social communication – the ability to communicate normally is impaired, as a person begins to take all words literally. There is no skill in generalizing and generating conclusions, understanding of metaphors, comparative phrases, jokes. Such consequences take a person out of his usual social circle and disrupt socialization.
- Self-organization - planning and information systematization skills disappear. For example, it is difficult for a person to tell a story following the sequence of events or episodes, to maintain the same topic of conversation, or to give any instructions.
- Disorientation – difficulty determining today's date, time, day of the week, time of year. Personal disorientation is possible, i.e. the patient does not remember his date of birth, age, last name.
- Violation of cause-and-effect relationships and difficulties in solving simple problems - a victim of a right-sided brain stroke cannot identify the problem, for example, that the medication has run out. And what actions need to be taken to deal with this, for example, write out a prescription, go to the pharmacy.
Right-sided cerebral circulatory disorders, in addition to serious physical disorders such as left-sided hemiparesis and paralysis, cause no less significant emotional and psychological consequences:
- Emotional lability – excessive laughter or tears “out of place”, inappropriate to the current situation.
- Apathy, decreased motivation for recovery and rehabilitation activities. Such sentiments can worsen the long-term prognosis for recovery.
- Denial of the fact of the disease and neurological defects, even such serious ones as hemiparesis, for example. The patient refuses to acknowledge the fact of a vascular catastrophe of the brain, as well as his physical defects.
- Reassessing your capabilities. Often patients refuse outside help and believe that they can take care of themselves completely independently. This is often not the case. Relatives should understand that the lack of outside help can lead to injuries and falls.
Prognosis for the patient
The consequences of an ischemic stroke depend on the location of the source of damage to the brain tissue (whether important brain centers are affected), the extent of the process and the age of the patient. The general condition of the body, the circulatory system, and the presence of diseases of the internal organs are of great importance. The first three days are considered the critical period; it is then that cerebral edema increases. Then there is stabilization of the condition and gradual restoration of lost functions.
And here is more information about brainstem stroke.
Ischemic stroke is often associated with atherosclerosis, heart disease, and impaired systemic or local circulation. It is manifested in most cases by focal neurological disorders - weakness of the limbs, impaired sensitivity, vision, speech. Depending on the location of the lesion, the symptoms have their own characteristics.
The most unfavorable course of an extensive stroke, as well as one complicated by cerebral edema. To provide adequate medical care, the patient must be hospitalized as soon as possible in a specialized department. Therapy in the first hours is aimed at dissolving the blood clot in the vessels, then complex drug treatment is prescribed. After a stroke, a long period of rehabilitation is required.
The main precursors of a stroke are quite pronounced. They differ in ischemic and hemorrhagic brains. It is important to notice the first signs in women and men in order to get help sooner.
If there was an ischemic stroke of the brain, the consequences remain quite severe. They differ depending on the affected area - left and right side, brain stem. Symptoms of the consequences are pronounced, treatment takes more than a year.
Ischemic stroke occurs quite often in the elderly. The consequences after 55 years are extremely severe, recovery is difficult and not always successful, and the prognosis is not so optimistic. Brain stroke becomes more complicated in the presence of diabetes mellitus.
When an ischemic stroke occurs, recovery takes a fairly long period. Is full recovery possible? Yes, if you complete a full course of rehabilitation, incl. to restore speech. What are the deadlines? What is needed after a major stroke of the cerebellum on the left side?
Drug treatment for stroke is prescribed to relieve severe manifestations of the disease. In case of hemorrhagic or ischemic brain damage, they will also help prevent the progression and increase of symptoms.
If a young person has a stroke, there is little chance of a full recovery. The causes of the pathology are often hereditary diseases and unhealthy lifestyle. Symptoms include loss of consciousness, convulsions and others. Why does ischemic stroke occur? What treatment is provided?
A real threat to life is a brainstem stroke. It can be hemorrhagic or ischemic. The symptoms resemble a heart attack and are also similar to other diseases. Treatment for a long-term, complete recovery after a brain stem stroke is almost impossible.
The reasons why a cerebellar stroke may occur are quite varied. Stroke can be ischemic, hemorrhagic, or stem. The treatment is long, recovery requires long-term rehabilitation. The consequences are problems with speech and movement.
A dangerous spinal cord stroke can lead to paralysis. The causes can be either congenital or acquired. Symptoms of ischemic stroke can be confused with other diseases. Treatment consists of taking pills, physical therapy and sometimes surgery. The consequences without treatment are dire.
. or: stroke of hemorrhagic type, cerebral hemorrhage, cerebral hemorrhage
Main problems
There is a whole list of possible complications.
Motor functions
Occurs with ischemic stroke of the left or right hemisphere and brain stem.
The chances of recovery directly depend on the extent and area of damage. As a rule, almost all patients recover partially. The disorder requires intensive rehabilitation lasting at least six months. The most effective treatment methods are:
- exercise therapy;
- walking training;
- massage;
- biofeedback with feedback;
- electrical stimulation of the neuromuscular system.
Paralysis
Find out whether the paralysis goes away or is permanent.
Observed when the cerebral hemispheres are damaged.
Each case of paralysis is unique and it is impossible to give an accurate prognosis. However, when the left hemisphere is damaged, it is much more favorable than when the right hemisphere is damaged.
Recovery occurs within six months to a year. However, severe brain damage cannot pass without leaving a trace on the body. Treated with:
- drug therapy;
- massage;
- acupuncture.
On our portal you will find detailed information about the causes and treatment of paralysis of the arms and legs after a stroke.
What is spasticity?
Increased muscle tone occurs with ischemic damage to the hemispheres and brain stem.
The prognosis is usually favorable; significant improvement in well-being with spasticity is possible within a year with complex treatment:
- medications (muscle relaxants, tranquilizers);
- It is also possible to use botulinum toxin, which relieves spasms;
- performing stretching exercises;
- electrical stimulation of motor points;
- surgical methods.
Bedsores
They arise due to the patient’s recumbent lifestyle. Such patients are forced to deal with trophic skin disorders. Complete disposal of them is possible only when the patient’s mobility is restored. In the meantime, while he is undergoing rehabilitation, it is very important to carry out regular prevention or treatment of bedsores:
- lining of special circles;
- regular change of body position every 2-3 hours;
- massage;
- use of special antiseptics;
- use of an anti-decubitus mattress.
Coordination
Appears when the vestibular apparatus is damaged, which occurs during a cerebellar stroke.
The prognosis is favorable if:
- start drug therapy as soon as possible;
- use biofeedback techniques;
- implementation of an individual exercise therapy program drawn up by a doctor.
Speech impairment and treatment
They occur with ischemia of the left hemisphere of the brain, and in left-handed people - the right.
This consequence is observed in 30% of patients who have had a stroke.
Restoring the ability to speak directly depends on the degree of damage to the speech center and is treated by taking nootropic drugs and classes with a speech therapist-aphasiologist-maphasiologist.
Motor aphasia
The patient's inability to speak, but understand speech addressed to him, develops with a stroke of the frontal lobe of the brain. Recovery depends on the work of defectologists, speech therapists and psychologists.
Sensory
Impaired understanding of someone else's and one's own speech while maintaining the ability to speak occurs with a stroke of the left temporal lobe of the brain.
The prognosis is positive with regular and constant work with a defectologist while taking a number of medications.
Amnestic
Occurs when the cerebral cortex zone is damaged in the parietal and temporal regions. The patient understands what kind of object is in front of him and what its function is, but cannot give it a name. Treatment consists of working with a speech pathologist.
Dysarthria
A person is able to write and read, understand the speech of others, but has problems with the pronunciation of his own speech. It is treated in the following ways:
- use of medications;
- performing special exercises for the tongue and lips;
- classes with a speech therapist.
Visual impairment
It is a symptom of damage to the visual analyzer, which is located in the occipital lobe of the brain.
In most cases, the phenomenon can be successfully treated, subject to proper selection of medications, timely surgery (if necessary), and regular oculomotor exercises.
Double vision
Characteristic of damage to the upper parts of the brain stem. The prognosis depends on the extent of the damage, but in most cases this phenomenon is reversible. With timely measures, it can be eliminated within six months.
Swallowing reflex
Read when recovery begins and how to teach a person to swallow if the swallowing reflex is impaired.
A common occurrence in strokes of the cerebellum and brainstem. Recovery begins in 2-3 weeks, some symptoms may persist for a long time. If the patient cannot swallow, this is treated with electrical stimulation of the laryngeal muscles.
What to do about hearing loss?
Characteristic of ischemic and hemorrhagic stroke of the left temporal lobe. The complication is difficult to treat, often requiring surgical intervention.
Hiccups
It develops due to a violation of the movement of the diaphragm, and is quite effectively treated with the use of Cerucal.
Vomit
Vomiting is a common manifestation of cerebellar stroke. But the question arises: “How to treat and what to do with this complication?” It is necessary to be treated with drugs based on metoclopramide.
Loss of consciousness
Occurs with extensive brain damage. Requires immediate hospitalization and administration of a number of medications. The prognosis depends on the area and extent of the lesion.
Headache
It can occur with any stroke, has a pronounced character, and can be relieved by taking painkillers.
In most cases, this complication completely resolves during the rehabilitation period.
Cognitive disorders, dementia or impairment of memory, intelligence
Frequent companions of ischemia of the cerebral hemispheres. The prognosis depends on the severity of symptoms. If they are severe, only partial recovery is possible. It is treated with the help of rehabilitation therapists, psychologists, and special classes.
Fecal and urinary incontinence
Urinary incontinence occurs when the frontal lobe of the brain is damaged. The prognosis is positive; in almost all patients it disappears after a few weeks.
Bowel control can be completely restored within a year in 2/3 of patients. The complication is treated with medication and diet.
Constipation
Constipation occurs when the conduction of impulses from the brain to the lower gastrointestinal tract is disrupted, also in bedridden patients. The symptom goes away within six months and is treated by taking laxatives and following a diet.
Insomnia
Insomnia is typical for patients who have suffered a stroke of the left hemisphere. Disappears during the first 3-6 months and is relieved by taking sedatives and sleeping pills.
Pneumonia
This complication is observed in almost half of patients with stroke. Bedridden patients are especially susceptible to pneumonia. Treated with antibiotics.
Cough
What does the presence of a cough in a patient indicate and how to treat it?
Most often, a cough is a sign of a respiratory tract infection, which is a common occurrence for patients, including bedridden patients with weakened immune systems in the hospital.
The prognosis is favorable with timely administration of antibiotics.
Epilepsy, as well as muscle spasms and cramps
With hemorrhagic stroke, pathology develops twice as often as with ischemic stroke.
The prognosis is usually unfavorable, and it is almost impossible to completely get rid of epilepsy. But the pathology must be treated with drugs based on valproic acid.
Read more about the causes of seizures after a stroke and treatment in our article.
Thrombosis and thromboembolism
Develops with ischemic brain damage. The prognosis is favorable provided adequate treatment in the form of aspirin and lifelong diet. If necessary, surgery can be performed.
Hallucinations
Find out whether hallucinations can be treated and what to do with this complication? Hallucinations are characteristic of extensive brain damage. They are treated in a hospital with the help of antipsychotics and work with a psychologist. As a rule, they pass without a trace, but in some cases they leave an imprint on a person’s personality.
Stupor and coma
A dangerous condition observed during a brain stem stroke. The prognosis is unfavorable, the risk of death is 80%.
We talked in detail about the causes, degrees and course of coma after a stroke here.
Repeated attack
It can be triggered by any type of stroke, is difficult to treat and has a disappointing prognosis - in 70% of cases it results in death.
Death
Death occurs in:
- 15% of cases of ischemic stroke;
- 65% - hemorrhagic;
- 45% - subarachnoid.
Forms
Depending on the location of the hemorrhage, the following forms of hemorrhagic stroke are distinguished.
- Subarachnoid hemorrhage (bleeding between the membranes of the brain).
- Intracerebral hematoma (accumulation of blood in the substance of the brain): hematoma of the frontal lobe;
- temporal lobe hematoma;
- hematoma of the parietal lobe;
- hematoma of the occipital lobe.
- Cerebellar hematoma (accumulation of blood in the substance of the cerebellum).
Depending on the presence of a breakthrough (entry) of blood into the cavity system of the brain (ventricles of the brain), the following forms of the disease are distinguished:
- hemorrhagic stroke with blood breaking into the ventricles of the brain;
- hemorrhagic stroke without bleeding into the ventricles of the brain.
Psychosomatic changes
Of course, brain damage during an illness leaves its mark on the patient’s behavior.
Aggression
Characteristic of hemorrhagic stroke. The prognosis depends on the severity of symptoms.
Depression
It occurs in almost all patients due to a deterioration in general well-being and a decrease in their quality of life.
Psychosis and emotional imbalance
Psychosis and emotional imbalance are difficult to treat , but in 2/3 of patients it is successfully treated within a year.
All of the listed psychosomatic disorders can be treated by taking special medications, working with a psychiatrist, and the support and patient attitude of loved ones.
Causes
- The cause of hemorrhagic stroke is rupture of the intracranial artery. Occurs due to a malnutrition of the vessel wall, its structural changes under the influence of various unfavorable factors.
- In addition, the causes of hemorrhage into the cranial cavity can be: rupture of a cerebral artery aneurysm (a saccular dilatation of the vessel with thinning of its wall. Can occur after injury, infection of the brain);
- rupture of arteriovenous malformation of the brain (an anomaly in the development of brain vessels, which develops in utero, after birth can increase in size. It is a tangle of intertwining arteries and veins).
- arterial hypertension (increased blood pressure more than 140/90 mmHg): especially prolonged increase to high numbers (more than 180/100 mmHg) without attempts to lower blood pressure with medication;
A neurologist will help in treating the disease
Bibliography
- Belova A.N. Outpatient rehabilitation of patients with consequences of cerebral stroke: a differentiated approach // Journal. neurology and psychiatry named after. S.S. Korsakov. 1996. - No. 1. - P.88-91.
- Vereshchagin N.V., Morgunov V.A., Gulevskaya T.O. Brain pathology in atherosclerosis and arterial hypertension. M.: Medicine, - 1997. - 288 p.
- Balunov O.A. On the issue of the effectiveness of rehabilitation of patients with consequences of stroke text. / O.A. Balunov, T.D. Demidenko, R.I. Lvova // Journal. neurol. and a psychiatrist. 1996. -No. 5. - P. 102-107.
- Lvova R.I. Occupational therapy of patients with motor disorders after cerebral stroke text. / R.I. Lvova//Organization and practice of occupational therapy in psychiatry and neurology: collection of articles. scientific tr.-L., 1982.-S. 98-105.
- Shklovsky V.M. Prognostic criteria for speech restoration in patients with consequences of ischemic stroke text. / V.M. Shklovsky, K.M. Shipkova, I.P. Lukashevich // Journal. neurol. and a psychiatrist. 1999. - No. 11. -S. 13-16.
Diagnostics
- Analysis of complaints and medical history: how long ago the complaints began (weakness in the limbs, difficulty swallowing, unsteadiness of gait, etc.);
- whether the patient previously noted an increase in arterial (blood) pressure, whether he took drugs that lower blood pressure (hypotensive);
- whether the patient abuses alcohol;
- whether the patient has previously been diagnosed with diabetes.
- the presence of disturbances of consciousness (does the patient answer questions, can he carry out simple commands, for example, raise his hands);
- CT (computed tomography) and MRI (magnetic resonance imaging) of the head: allows you to study the structure of the brain layer by layer, detect signs of hemorrhage, assess its volume and location.
- Echo-encephalography: the method allows you to assess the presence of displacement of the brain relative to the bones of the skull under the influence of pressure from intracranial hemorrhage.
- Lumbar puncture: using a special needle, a puncture is made in the subarachnoid space of the spinal cord at the lumbar level (through the skin of the back) and 1-2 ml of cerebrospinal fluid (the fluid that provides nutrition and metabolism in the brain and spinal cord) is taken. Since the subarachnoid space of the spinal cord communicates directly with the subarachnoid space of the brain, in the presence of hemorrhage between the membranes of the brain, blood or its remains can be detected in the cerebrospinal fluid.
Anatomy and functions
The cerebral cortex consists of two interconnected hemispheres. These hemispheres are formed by the gray matter of the brain, which consists of grooves and convolutions - the same characteristic type of brain to which we are all accustomed.
Each hemisphere consists of 5 lobes:
- Frontal
- Parietal
- Occipital
- Temporal
- The insula is the smallest and separates the frontal lobe from the temporal lobe.
Each lobe has its own tasks and functions, so defeat of any of them causes serious consequences. The hemispheres of the brain as a whole are its most important part, since they are responsible for higher nervous or, in other words, mental activity, thinking. This type of nervous activity is unique to humans and distinguishes them from all other mammals.
The main tasks of the right hemisphere of the brain:
- Control of movements of the left half of the body
- Thought processes, cause-and-effect relationships
- Memory, ability to concentrate
- Planning, self-organization
- Perception of yourself and the world around you
- Vision
- Communication skills
Of course, these are only the basic functions of the right hemisphere of the brain, many of them are still being studied and specified by medical scientists.
Treatment of hemorrhagic stroke
- Urgent hospitalization in a neurological or neurosurgical department with constant monitoring of the patient's condition.
- Hemostatic therapy (medicines that improve blood clotting).
- Decrease in arterial (blood) pressure when its values are too high (more than 220/100 mmHg).
- Drugs that improve the restoration of nervous tissue (neuroprotectors, neurotrophics).
- Complete care for a bedridden patient: physical therapy, breathing exercises, skin treatment, hygiene procedures.
- Restoration of impaired neurological functions: classes with a speech therapist, physical therapy.
- Surgical removal of the hematoma, if possible (for superficial hematomas): either aspiration of the blood is performed (through a syringe needle inserted into the hematoma) or removal of the hematoma through a trepanation hole (a hole in the bones of the skull).
Headaches due to hypertension
- 1 Why does pain occur?
- 2 Types and nature of pain
- 3 Other symptoms of hypertensive headache
- 4 Help for headaches 4.1 Drug treatment
- 4.2 Folk remedies for headaches
Head pain can be caused by many reasons, one of which is high blood pressure. Headaches due to hypertension occur due to the narrowing of blood vessels in the brain and dilation of veins, which provokes a sharp increase in blood pressure. Such symptoms cannot be ignored, since it is possible that there is a retinal hemorrhage, a heart attack or a stroke.
Why does pain occur?
The causes of headaches lie not only in high blood pressure, they can be very diverse. Therefore, with such attacks you should seek medical help. According to scientists, only 5-10% of people suffer from organic pain that requires medical attention. In other cases, the person himself becomes the culprit of these painful sensations. They are caused by the following factors:
on
- constant lack of sleep, stress, nervous tension;
- overwork;
- sudden change in weather conditions;
- eye strain;
- outbreaks of colds;
- fasting, diets;
- uncontrolled use of medications (self-medication).
If pain attacks occur no more than once a month for a known reason and are relieved with painkillers, there is no need to worry. But if migraine is present every day and does not recede, then this is hypertension. The source of pain in this case is the blood vessels of the brain, which narrow and can lead to a stroke.
Return to contents
Types and nature of pain
A drop in blood pressure in the range of 25-30% of normal will certainly provoke hypertensive pain that radiates to the head. Frequent pain of this type is called cephalalgia, which comes in the following types:
- During movement, the pain in the back of the head only intensifies.
Liquor. It is characterized by throbbing, bursting pain in the occipital part of the head, which increases with active movements. Possible nausea, blurred vision and weakness. Appears with increased blood pressure. Mostly it does not last long, but can recur with active movements or changes in weather conditions. - Ischemic. Dull, aching, prolonged pain in the occipital and temporal parts of the head, often arising due to nervous tension, possibly the appearance of asterisks and dizziness. It also appears as a result of increased blood pressure and insufficient blood supply to the brain.
- Neuralgic. It is localized in the back of the head, radiates to nearby areas, and is distinguished by its sharpness. The cause of the appearance is nervous stress, possibly the appearance of relapses.
- Muscular. Causes a feeling of squeezing of the head, which can increase and subside, accompanied by unsystematic dizziness, nausea, and vomiting. It occurs as a result of emotional shock, which provokes a spasm of the head muscles.
- Vascular pain - throbbing pain in the temples and back of the head, heaviness that intensifies when turning the head and coughing.
Several types of pain symptoms may occur simultaneously, however, only a doctor can understand the cause after a full examination. Only after an accurate diagnosis is established is medication prescribed for hypertension.
Return to contents
Other symptoms of hypertensive headache
High blood pressure can cause dizziness.
The main symptom of high blood pressure is headaches of various types. But often there are other symptoms that help to more accurately determine the diagnosis and prescribe treatment. Other symptoms include: swelling, rapid heartbeat, dizziness, blurred vision, nausea and vomiting, and eye pain. The above symptoms may indicate other diseases. Therefore, it is important not to self-medicate when you have a headache, but to seek medical help in time.
Return to contents
Help with headaches
Treatment of headaches should begin with determining the cause of the disease. If the patient is sure that the sensations arise from increased pressure, it is necessary to take medications to reduce pressure. However, treatment should only be done according to the doctor’s recommendations. Headaches with hypertension are a common occurrence. At different stages of the disease, different treatments are prescribed, but all prescriptions come down to the correct daily routine and diet. It is worth avoiding stressful situations, spending more time in the fresh air, resting and maintaining a sleep schedule. It is also important for hypertensive patients to limit themselves in salt intake, smoking and alcoholic beverages.
Return to contents
Drug treatment
Headache due to hypertension is caused by spasm of blood vessels in the brain. However, it can be treated with medications, which are divided into the following groups:
- Drug treatment should be supervised by a physician.
Beta blockers are medications that reduce the heart rate and neutralize the effect of adrenaline, which enters receptors in the blood vessels of the brain. - Tranquilizers relieve symptoms such as chills, migraines, and dry mouth. Such drugs include Valium, Phenazipam, and Xonax tablets. They are quite often prescribed to patients because they are well tolerated.
- Analgesics are taken to relieve pain. It is possible to use tablets such as Ibuprofen, Diclofenac, Analgin, Citramon.
- Antidepressants serve to neutralize increased levels of adrenaline. In a stressful situation, a person increases the production of this substance and increases blood pressure.
- Diuretics serve to remove excess fluid from the body, which helps normalize blood pressure and relieves signs of hypertension.
Return to contents
Folk remedies for headaches
Folk remedies are additional measures to eliminate migraines that will help relieve symptoms. Unlike drug treatment, which cannot be taken without a doctor's recommendation, these methods will not cause harm and will alleviate the condition. These include:
- Taking a hot foot bath.
- Use mustard plasters on the back of the head, as well as dry mustard on the feet at night.
- Using valerian tincture to improve sleep.
- Walking in the fresh air has a positive effect.
- It is possible to massage the head and neck (not allowed with very high blood pressure).
As well as folk methods, it is worth including tinctures and decoctions of herbs, such as clover flowers, oregano, and mint. Cranberries have healing properties. Its use has a beneficial effect on blood vessels, normalizes blood pressure, and protects against headache attacks. They are consumed both fresh and in the form of fruit drinks and compotes.
It is important to remember that folk methods alone cannot cure you; they can only relieve symptoms and make you feel better. The causes of headaches and high blood pressure are determined only by specialists after a complete examination. Medicines should be prescribed and monitored by a doctor. But don’t forget about the basic rules for preventing hypertension: spend more time in the fresh air, avoid stressful situations, eat well and rest.
on
A comment
Nickname
How quickly was the ambulance called?
You should seek medical help when the first signs of a stroke appear.
The patient's chance of survival depends on this. The main danger of ischemic stroke is that over time the area of damage to the brain increases. In this case, minutes count.
If it were not for the increase in the affected area, the disease did not require rapid action. The dead area would become like a scar (if it is large), or would disappear over time, being replaced by new cells (if it is small).
But it is necessary to save the area around the dead neurons, in which the blood flow is increasingly deteriorating, and the destruction of cells that have lost connections with the dead cells occurs. This is only possible with the elimination of the blood clot.
The blood clot that caused the stroke can be dissolved only within 1 hour from the moment the first symptoms of the disease appear. This is done using thrombolytic drugs, which are injected into a vein in the intensive care unit.
Thrombolysis is carried out after a computed tomography scan shows that the stroke is ischemic and not hemorrhagic. It will not be executed if:
- the stroke was caused by a brain tumor;
- there were seizures at the onset of the stroke;
- less than 3 months have passed since the person received a traumatic brain injury or surgery on the brain or spinal cord;
- less than 3 months have passed since the previous stroke;
- ischemia has already occupied more than 1/3 of the area supplied by the middle cerebral artery;
- blood pressure rose above 185/110 mm Hg;
- a person has poor blood clotting;
- in the last 3 months there have been any bleedings: gastrointestinal, renal, uterine;
- the person has cirrhosis or active hepatitis, which increases the risk of bleeding.
Thus, if you called an ambulance as soon as you realized that a relative had a stroke, then his chance of survival is higher. And if he does not have the above contraindications to the administration of a thrombolytic, the chance increases even more.
Manifestations of brainstem damage
A brainstem stroke is accompanied by damage to the pathways and nuclei of the cranial nerves, and is therefore accompanied by rich symptoms and severe disorders of the internal organs. Signs of the disease manifest themselves acutely, starting with intense pain in the occipital region, impaired consciousness, paralysis, dizziness, tachycardia or bradycardia, and sudden fluctuations in body temperature.
General cerebral symptoms are associated with increased intracranial pressure; they include nausea and vomiting, headache, impaired consciousness and even coma. Then symptoms of damage to the nuclei of the cranial nerves and focal neurological symptoms appear.
Ischemic brainstem stroke is manifested by a variety of alternating syndromes and signs of involvement of the cranial nerve nuclei of the side where necrosis occurred. In this case, the following may be observed:
- Paresis and paralysis of muscles on the side of the affected part of the trunk;
- Deviation of the tongue towards the affected side;
- Paralysis of the part of the body opposite to the lesion with preservation of the work of the facial muscles;
- Nystagmus, imbalance;
- Paralysis of the soft palate with difficulty breathing, swallowing;
- Drooping of the eyelid on the side of the stroke;
- Paralysis of the facial muscles on the affected side and hemiplegia of the opposite half of the body.
This is only a small part of the syndromes accompanying brainstem infarction. With small lesion sizes (up to one and a half centimeters), isolated disturbances in sensitivity, movements, central paralysis with pathology of balance, hand dysfunction (dysarthria), isolated disturbance in the functioning of the muscles of the face and tongue with speech disorder are possible.
With hemorrhagic brainstem stroke, symptoms increase rapidly ; in addition to motor and sensory disorders, intracranial hypertension is clearly manifested, consciousness is impaired, and the likelihood of coma is high.
Signs of hemorrhage in the trunk may be:
- Hemiplegia and hemiparesis - paralysis of the muscles of the body;
- Visual impairment, gaze paresis;
- Speech disorder;
- Decreased or absent sensitivity on the opposite side;
- Depression of consciousness, coma;
- Nausea, dizziness;
- Increased body temperature;
- Impaired breathing and heart rhythm.
A stroke usually occurs suddenly and can be witnessed by loved ones, colleagues or passers-by on the street. If a relative suffers from hypertension or atherosclerosis, then a number of symptoms should alert relatives. Thus, sudden difficulty and incoherence of speech, weakness, headache, inability to move, sweating, fluctuations in body temperature, palpitations should be a reason to immediately call an ambulance. A person’s life may depend on how quickly others orient themselves, and if the patient is admitted to the hospital in the first few hours, the chances of saving a life will be much greater.
Sometimes small foci of necrosis in the brain stem, especially those associated with thromboembolism, occur without a sharp change in condition. Weakness gradually increases, dizziness appears, gait becomes uncertain, the patient experiences double vision, hearing and vision decrease, and eating becomes difficult due to choking. These symptoms also cannot be ignored.
Trunk stroke is considered a severe pathology, and therefore its consequences are very serious. If in the acute period it is possible to save life and stabilize the patient’s condition, bring him out of a coma, normalize blood pressure and breathing, then significant obstacles arise at the rehabilitation stage.
After a brainstem stroke, paresis and paralysis are usually irreversible, the patient cannot walk or even sit, speech and swallowing are impaired. There are difficulties with eating, and the patient needs either parenteral nutrition or a special diet with liquid and pureed food.
Contact with a patient who has suffered a brainstem stroke is difficult due to speech impairment, but intelligence and awareness of what is happening can be preserved. If there is a chance to at least partially restore speech, then a specialist aphasiologist who knows techniques and special exercises will come to the rescue.
After a heart attack or hematoma in the brain stem, patients remain disabled, requiring constant participation and assistance in eating and performing hygiene procedures. The burden of care falls on the shoulders of relatives, who must be aware of the rules of feeding and handling a seriously ill person.
Complications from brainstem stroke are not uncommon and can cause death. The most common cause of death is considered to be edema of the brainstem with its entrapment under the dura mater of the brain or in the foramen magnum; uncorrectable disturbances of the heart and breathing, and status epilepticus are possible.
In a later period, urinary tract infections, pneumonia, thrombosis of the leg veins, and bedsores occur, which is facilitated not only by neurological deficits, but also by the forced recumbent position of the patient. Sepsis, myocardial infarction, and bleeding in the stomach or intestines cannot be ruled out. Patients with milder forms of brainstem stroke who attempt to ambulate are at high risk of falls and fractures, which can also be fatal.
Relatives of patients with brain stem stroke already in the acute period want to know what the chances of recovery are. Unfortunately, in a number of cases, doctors cannot reassure them in any way, since with this localization of the lesion we are talking about saving lives in the first place, and if the condition can be stabilized, then the vast majority of patients remain deeply disabled.
The inability to correct blood pressure, high, persistent body temperature, and a comatose state are unfavorable prognostic signs in which there is a high probability of death during the first days and weeks after the onset of the disease.
Atrial septal aneurysm (ASA)
Atrial septal aneurysm (ASA) is a sac-like protrusion of the septum between the right and left atrium. It usually occurs in the place where the septum is most thinned, due to one feature.
The fact is that during intrauterine development there is an opening in the interatrial septum (foramen ovale) that should close after birth. In most cases, this happens, but in some people, after closure, a “thin place” forms in this place, which, under blood pressure, begins to stretch and a protrusion is formed - an aneurysm.
Doctors have known about the aneurysm of the sac for a long time, but until now there have not been sufficiently large studies that would allow all specialists to come to a clear opinion on a number of important questions, including those that are often asked by patients with this anomaly or their relatives.
When do we talk about an aneurysm?
It is believed that it is possible to speak reliably about an aneurysm in cases where, according to ultrasound of the heart, the protrusion exceeds 10 mm. But this norm is conditional, so a protrusion of 9 mm, 7 mm, and even 5 mm can also be called an aneurysm.
Are there any special complaints in patients with this pathology?
There are no specific complaints that could lead to suspicion of an aneurysm of the sac.
How is an aneurysm of the sacral tract diagnosed?
The main diagnostic method is a conventional cardiac ultrasound with Doppler ultrasound. If necessary, clarifying examinations may be needed: transesophageal ultrasound, tomography or cardiac catheterization. But additional examination is usually carried out in cases where, in addition to the aneurysm, there is a suspicion of a defect in the aneurysm and next to it, or in the presence of another, concomitant, anomaly of the heart and large vessels.
Does an STD aneurysm interfere with the functioning of the heart?
Opinions agree on this issue: in the overwhelming majority of cases, the SCP aneurysm itself does not disrupt the functioning of the heart, that is, it does not reduce its pumping function.
Why is an aneurysm dangerous?
All patients are afraid of aneurysm rupture and understand this as almost a heart rupture, but this is not so. The pressure in the atria is not high enough to cause the aneurysm to rupture. But even if this happens, it will not entail any immediate consequences - it will simply form a defect that people can live with for decades without any serious consequences. So these fears can be put aside, but, unfortunately, there is another problem - the risk of cerebrovascular accident or stroke.
There are a number of statistics that suggest that patients with an aneurysm have a potential risk of developing blood clots in the aneurysm, which, if broken off, could potentially cause a stroke. Broken blood clots are called emboli.
This statement is based on statistical data that aneurysm of the bladder is quite common in patients who have suffered an embolic stroke (“broken thrombus”). However, perhaps the aneurysm itself has nothing to do with it. Perhaps the culprit for all this is a defect in the uterus or other associated anomalies, which often coexist with an aneurysm. This question is still open; too few patients were observed to answer definitively. However, it can be said that atrial aneurysms smaller than 1 cm do not increase the risk of stroke as significantly.
For those who are interested in knowing more, I provide accurate research data.
Data from the Mayo Clinic (USA). Stroke or TIA (Transient Ischemic Attack - a temporary and reversible disruption of the blood supply to the brain) was observed with an aneurysm of the bladder in 20% of patients. But in 75% of patients from this group, other concomitant anomalies in the development of blood vessels and the heart were identified.
From the author: that is, if we discard this 75%, then the risk is reduced to 5%. At the same time, it is not at all a fact that among these 5% there are no patients in whom concomitant anomalies were simply not diagnosed or there was another reason for the embolism.
Data from the article Belkin RN, Kisslo J. Hurwitz BJ. We observed a group of 36 patients with an aneurysm of the bladder. 28% of them had episodes of cerebrovascular accidents. Moreover, in 90% of cases, the examination also revealed a defect in the septum with a pathological discharge of blood (from the right atrium to the left), which could cause the so-called paradoxical embolism.
From the author: paradoxical embolism refers to cases when, for example, a blood clot (embolus) from the veins of the lower extremities breaks off and enters one of the arteries of the brain. This cannot happen in patients who do not have heart defects. Such blood clots usually enter the arteries of the lungs and do not pass to the left side of the heart, that is, they cannot enter the aorta, and from there to the arteries of the head.
In addition, it turns out that in this study, if we select only patients with just one aneurysm of the aneurysm, the risk decreases to 2.8%. This is not to mention that this study was conducted back in 1987.
Summary data (a number of European clinics). Of 78 patients with atrial aneurysm, 40% had previously experienced episodes of embolism, but in only about 10% of these, the aneurysm was the only possible source of thrombus.
From the author: that is, here too the risk of cerebral circulatory disorders was observed in only 4%.
Again, I repeat that the connection between strokes and aneurysm is only an assumption, since there are a number of other causes of embolism that may have been absent at the time of the examination or simply missed. That is, the percentages given in studies may be an order of magnitude lower. And as a result, they may become quite comparable with the average total risk of stroke and TIA in the population – 0.3%.
However, there is an expert opinion that the risk of embolism increases significantly if the aneurysm exceeds the size of 10 mm - this is a fact.
Treatment of aneurysm
Treatment for aneurysms up to 10 mm in size is usually not required.
In case of large sizes or previous embolisms, the prescription of blood thinners is obviously required. But if for patients who have already had a stroke or transient ischemic attack there are recommendations tested on hundreds of thousands of patients, then for an asymptomatic aneurysm more than 1 cm there are no such schemes and, probably, there will not be for a long time.
It can be assumed that for this group of patients it would be beneficial to use regular aspirin or another antiplatelet agent as prophylaxis. But I have not come across such recommendations, so this remains at the discretion of the attending physician, especially when it comes to children (for whom aspirin is generally contraindicated).
As for surgical treatment, it will be indicated only in cases where there is a large aneurysm that disrupts the functioning of the heart, or a significant defect in the interatrial septum forms simultaneously with the aneurysm.
- Treatment of atrial septal defect
- Atrial septal defect
- What happens with an atrial septal defect?
- Symptoms and diagnosis of atrial septal defect
- Is it possible to play sports with an atrial septal aneurysm?
- Aneurysmal protrusion of the interatrial septum
- Is an atrial septal defect life-threatening?
Is it possible to drink alcohol if you have arrhythmia?
Arrhythmia is a general term for a rhythm disorder...
The formulation of hypertension - how to decipher the diagnosis
Ten years ago, a diagnosis of hypertension with indication...