Description of the method
The design of a spiral CT apparatus consists of a movable couch and a ring frame, which encloses an X-ray tube with high heat capacity and a set of sensors.
When scanning is started from the control console, the X-ray tube begins to continuously rotate around the object under study and emit a beam of rays along a fan-shaped trajectory.
At the same time, the table with the patient makes a continuous linear movement at a given speed, depending on the purposes of the study.
The beam passing through the body is captured in the form of a signal by a system of receiving devices on the opposite side. Information from the sensors is transmitted to the control room, processed and converted into an image on the monitor screen.
The abbreviation SCT fully reflects the essence of diagnostics, which is one of the methods of X-ray tomography with computer processing of the information obtained.
What happens during the examination
The image of the examined organ is obtained through several mandatory steps:
- X-ray beam width adjustment;
- Scanning the kidneys, lungs, liver or other organs using X-rays;
- Capturing pulses with special sensors and processing them into digital data;
- Computer data processing;
- Displaying information on the monitor screen.
The resulting SCT images must be examined by a radiologist (a doctor who specializes in CT, MRI, X-ray studies and has the appropriate certificate). It is necessary to “read” all the scans, study the provided medical information. documentation, compare it with the obtained CT image, describe the study, draw a diagnostic conclusion, shoot film with scans. On average it takes about 1-3 hours. At ACMD, we undertake to prepare the results for delivery by the end of the Clinic’s working day.
To diagnose which organs is SCT used?
SCT has been widely used in medicine since 1989. The method has accuracy, high scanning speed, and the ability to visualize organs, soft tissues and bone structures.
SCT reveals pathological changes in the following organs:
- brain;
- organs and tissues of the neck: thyroid gland, laryngopharynx, lymph nodes, sublingual space;
- chest organs: lungs, thymus, heart, esophagus, trachea, lymph nodes;
- organs of the abdominal cavity and retroperitoneal space: liver, pancreas, spleen, kidneys with adrenal glands;
- pelvic organs: uterus, ovaries, prostate, bladder;
- spine, osteoarticular apparatus;
- vascular structures: coronary arteries, aorta, renal arteries, cerebral arteries.
In what cases is it carried out?
Spiral CT is prescribed when it is necessary to diagnose an organ as quickly as possible. This can happen in a number of situations:
- if internal organs and the brain are seriously injured;
The study is carried out on brain injuries
- when a chest examination is required, but the person is unable to hold his breath for a long time;
- if necessary, examine patients with whom close contact cannot be established at this moment;
- to diagnose those patients whose pain increases when lying down.
In addition, the SCT procedure is performed in situations where the exposure received from X-rays should be minimal, for example:
- children under twelve years of age;
- if necessary, establish the presence or absence of pathology of blood vessels, especially the coronary arteries;
- if virtual endoscopy is required.
The procedure is suitable for examining children
Difference between CT and SCT
With step-by-step CT, a single slice image is obtained during one rotation of the “tube-detector” system around the area of interest.
The table is then moved a predetermined distance and the rotation of the tube is repeated again to obtain the next image. The thickness of the resulting slice is 1 cm.
During diagnostics, a spiral tomograph collects data continuously due to the synchronous movement of the couch with the patient and the tube describing a helical trajectory.
This allows you to increase the speed of diagnosis, examine one anatomical area in 1 phase of the respiratory cycle and obtain sections 2-3 mm thick.
Distinctive features of MSCT from SCT
MSCT is based on the operating principle of SCT. To increase the speed of diagnosis, the devices were equipped with multi-row detectors.
MSCT scans an object with 4-helices in one revolution of the tube, while the rotation speed is 0.5 seconds faster than the MSCT.
As a result, it became possible to obtain from 4 to 64 sections simultaneously, with a minimum tube rotation time of 0.3 seconds.
The duration of scanning of all anatomical structures of the human body was 10-15 seconds.
Advantages of SCT over MRI
A valuable property of SCT is the speed of scanning and the speed of obtaining diagnostic information necessary for making a diagnosis and starting treatment measures.
Unlike MRI, which takes up to 1 hour to visualize pathology, with SCT the same amount of information is obtained in 10-15 minutes.
The strength of MRI is considered to be the staging of cancer, the detection of diseases of soft tissues and the spinal cord, while bone structures are poorly visible.
SCT, on the contrary, clearly visualizes the osteoarticular apparatus, and is the method of choice for determining painful changes in this area.
In what cases is SCT prescribed?
The method is indicated for emergency diagnosis of acute conditions caused by head and torso injuries in unconscious patients with severe pain, when the patient cannot remain in a stationary position for a long time.
A routine scan is prescribed to identify:
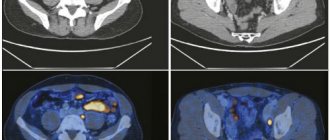
- formations of a malignant and benign nature, determining the stage, metastatic damage to neighboring organs, lymph nodes;
- inflammatory, purulent-destructive processes;
- degenerative-dystrophic processes;
- congenital anatomical disorders;
- foreign bodies, stones;
- circulatory disorders;
- mechanical damage.
CT or MRI?
Which study is more informative: CT or MRI?
– These are not entirely alternative research methods, since they are suitable for different structures of the body. MRI better shows organs with a high fluid content, deeply hidden under the bone skeleton: these are the brain and spinal cord, intervertebral discs, joints and pelvic organs.
With CT, the skeleton itself and lung tissue are distinguished in detail, so X-rays and the high resolution of a computed tomograph can be most useful for studying these structures. In addition, fresh bleeding is clearly visible on CT, so CT is used in studies of patients with head, chest, and abdominal and pelvic injuries, as well as early-stage strokes.
When diagnosing diseases of the digestive organs and digestive glands, neck organs, kidneys, especially with contrast enhancement, both spiral CT and MRI can be used with equal success. However, spiral CT is a faster (and cheaper) diagnostic method. If in an emergency you need to make a diagnostic decision instantly, then CT has no competition. In some cases, the same organ can be studied using both CT and MRI, but there are certain nuances known only to a professional. For example, for problems with the spine, both CT and MRI can be used. CT is ideal for diagnosing bone lesions and spinal injuries.
How does the procedure work?
Spiral computed tomography is performed in accordance with recommended diagnostic algorithms by a specially trained radiologist.
The diagnostician is assisted by an x-ray technician. If the scanning requires the administration of narcotic substances, the anesthesiology team is involved.
Before the procedure, the patient undergoes training and undergoes additional laboratory and diagnostic tests.
When planning the use of contrast agents during tomography, an allergy test is first performed.
Siemens Somatom Perspective (MSCT) device
An explanatory conversation is held with the patient in the CT room. The patient is informed about the progress of the scan, behavior during the procedure, and possible side effects. When using contrast or anesthesia, informed consent is signed.
In the equipment room, a laboratory assistant helps the patient take the correct position on the diagnostic couch of the tomograph.
If necessary, place cushions under the head and limbs. To avoid the appearance of artifacts in the images, the patient is fixed to the table with belts.
With contrast enhancement, a catheter is inserted into the vein, to which an automatic syringe is attached to deliver the substance.
Pediatric patients with uncontrolled motor activity are given sedatives or short-acting anesthesia. Communication with the doctor is maintained through an internal two-way channel.
In the control room, the doctor starts the scan through the control console, controls the movement of the table and the tilt of the gantry.
The couch with the patient slides into the frame of the device and stops in the target area. The rotation of the tube-detector system around the patient's body is accompanied by continuous translational movement of the table.
At the end of the procedure, which lasts an average of 15 minutes, the patient goes home or awaits the results at the diagnostic center.
After intravenous contrast enhancement, the patient is left under observation for 30-40 minutes. Depending on the complexity of the case, it takes from 1 to 24 hours to decipher the data and draw up a protocol of identified changes.
Note to readers
In which cases is which research more informative?
Our table will help you determine this.
| MRI | CT | MRI and CT with contrast agent injection |
| Chronic processes | Fresh hemorrhage | Diagnosis of diseases of the digestive and excretory organs |
| Osteochondrosis, herniated discs | Trauma to bones, head, chest, pelvis | |
| Late stage stroke | Early stage stroke |
Negative effects of the technique on the body
SCT is considered a relatively safe examination method. A potential threat to the patient’s health and life is associated with the effect of ionizing radiation on the body’s cells.
The risk of developing cancer increases over the next 10-20 years when using one or more x-ray techniques whose annual dose exceeds 5 mSv.
To determine the dose, use the “Dosimeter”.
When the fetus is exposed to rays during intrauterine development, the likelihood of disruption of the formation and maturation of organs and tissues increases, which leads to anomalies and developmental defects. In children under 18 years of age, physical development may be delayed during the period of active growth.
Acceptable frequency of diagnostic procedures
For each patient who has been exposed to radiation for diagnostic purposes, a dose load recording card is created.
It records the types of x-ray procedures performed during the year and the individual effective doses used.
When making a primary or repeated referral for tomography, the doses received from the previous diagnosis are taken into account.
The radiation dose for SCT depends on the volume, scanning area, and contrast enhancement. It is allowed to do SCT 1-2 times a year.
According to vital indications, the frequency of diagnosis is increased at the discretion of the attending physician and radiologist.
Research stages
Carrying out spiral tomography, taking into account the time spent on preparation, data processing, formation of orders and recommendations by a radiologist, takes no more than 4 hours. No special preparation is required. The patient is recommended to undergo a preliminary MRI and ultrasound, and should not eat, drink or smoke 4 hours before the examination.
Stages of SCT diagnostics:
- administration of contrast (intravenously or orally);
- placing the patient on a mobile table (since you will need to lie still, in some cases the doctor prescribes sedatives);
- the table moves inside the gantry - “pipe” (the irradiation source rotates along a spiral trajectory);
- a scan is performed (usually the procedure takes from 5 to 30 minutes);
- information is displayed on a computer monitor (if desired, it can be recorded on a portable device);
- The radiologist deciphers the diagnostic result and issues a referral for consultation with specialists.
Examination using SCT is absolutely painless and may cause minimal discomfort associated with being in a confined space.
In order for the interpretation of the study results to be as accurate and reliable as possible, you need to provide the radiologist with your medical card or a report from the attending physician indicating a preliminary diagnosis. Then the doctor will be able to take into account all previous diseases and injuries, as well as the individual structural features of the patient’s body.