Many people experience pain in the back of the skull. For some, it goes away quickly, while others are forced to look for the cause of constant discomfort. Pain at the base of the skull and neck can have a different character - aching, throbbing, pressing. Sometimes there is a connection with physical activity, hypothermia or stress, but in some cases the cause cannot be determined.
According to doctors, the most likely culprits of pain are vascular pathologies or degenerative processes in the spine. Is it really?
What can hurt
The cervico-occipital zone contains many structures - muscles, tendons, nerve endings, cervical vertebrae, as well as the occipital bone and brain. There is an extensive network of arteries and vessels, damage to which can lead to serious complications. The most important are the occipital, posterior cerebral and auricular arteries, and the posterior branches of the middle cerebral artery.
The innervation of the neck and shoulder girdle is quite complex, so the pain is often diffuse. Having arisen, for example, behind the back of the head, pain spreads to the upper back, shoulders or sides of the skull. This feature sometimes makes diagnosis very difficult.
Pain at the base of the skull can be caused by the following reasons:
- osteochondrosis;
- spondylitis;
- spondylosis;
- cervical migraine;
- occipital neuralgia;
- increased blood and intracranial pressure;
- myositis;
- myogelosis;
- pathologies of the temporomandibular joints.
Important: each disease has its own characteristic symptoms, indicating damage to one or another structure.
Severe pain in the head at the base of the skull
Head pain at the base of the skull may be caused by increased intracranial pressure. In this case, it is worth paying attention to accompanying clinical symptoms such as dizziness, nausea and vomiting. If all these signs are present, it is necessary to call an ambulance team as quickly as possible.
You will also need urgent medical attention if severe pain at the base of the skull is accompanied by nosebleeds, increased heart rate, or numbness in certain parts of the body. This may be a clinical picture of a developing transient cerebrovascular accident. It often occurs in people who have suffered for a long time from cervical osteochondrosis, complicated by posterior vertebral artery syndrome.
Impairment of the spinal canal is another potential cause of pain in the base of the skull. This may be a consequence of displacement of the vertebral bodies, traumatic damage to the bone structure, prolapse of the intervertebral hernia, etc. If there is throbbing pain at the base of the skull, then exclude all further physical activity. Take a horizontal position with your head raised. Provide fresh air. Call an ambulance. In such situations, you should not provide first aid to yourself. This can lead to tragic consequences.
Cervical migraine
Against the background of osteochondrosis affecting the first or second vertebra, cervical migraine may develop. This pathology is sometimes associated with congenital abnormalities of the spine, but most often it is caused by thinning and destruction of the intervertebral discs.
Initially, cervical migraine is reversible and occurs only during exacerbations of osteochondrosis. Vascular spasm occurs periodically, but over time the vessels do not return to their normal physiological state. This leads to almost constant pain in the back of the neck at the base of the skull.
Characteristic symptoms of cervical migraine:
- sharp or throbbing pain;
- spread of pain to the forehead, temples, eyes and bridge of the nose;
- dizziness;
- decreased visual acuity;
- nausea;
- touching the head with a comb or fingers causes severe discomfort;
- fainting (in severe cases).
Headache in the back: types of pain, causes, symptoms and treatment methods
Having pain in the back of the head is a problem that should not be underestimated. The causes of unpleasant sensations may lie in diseases and pathogenic conditions.
Often the pain syndrome is accompanied by nausea, vomiting, and increased sensitivity to external factors.
To prevent the development of dangerous complications, it is necessary to have an understanding of the etiology of pathological processes, their types, as well as modern methods of diagnosis, treatment and prevention.
Causes of headaches from behind
In most cases, discomfort in the back of the head develops due to chronic fatigue. In addition, pathology can be observed in the presence of a number of factors, the main of which are:
- spasm or dilation of the lumen of cerebral vessels;
- intoxication of the meninges with various chemical and toxic substances;
- increased blood or intracranial pressure;
- damage to the body by agents of viral and bacterial etiology;
- overstrain of muscle fibers;
- metabolic disorders;
- frequent stress, depression, emotional stress;
- dehydration;
- heat and sunstroke;
- skull injuries.
Among the provoking factors, the most common are increased blood pressure, insomnia, and increased weather sensitivity.
In addition, smoking and frequent consumption of alcoholic beverages can lead to pain in the back of the head.
Possible diseases
The causes of pain in the back of the head also include diseases that can lead to the development of a pathological syndrome. The most common among them are:
- diseases of the cervical spine;
- pathologies of the brain, cerebellum, pons, kidneys and adrenal glands;
- diseases that are accompanied by increased intracranial pressure;
- damage to the muscular system of the neck;
- disturbances in the regulation of blood vessel tone;
- arthrosis, arthritis;
- myositis;
- myogelosis;
- spondylosis, spondylitis;
- migraine;
- occipital neuralgia;
- hormonal imbalances;
- disorders in the musculoskeletal system.
Hypertension is one of the most common causes of pathology. It is accompanied by nausea, possible vomiting, a feeling of heat, flushing of the skin of the face and pain to the left of the sternum. This disease is most often observed in the presence of the following factors:
- age over 45 years;
- excess weight;
- systematic consumption of alcoholic beverages;
- history of stroke or heart attack.
Osteochondrosis of the cervical spine is the second most common cause of pain in the back of the head.
The disease is characterized by a malnutrition of the intervertebral disc, as a result of which it is erased, and its shock-absorbing component is displaced with further exit into the lumen of the spinal canal.
In place of the thinned disc, osteophytes form, which can impinge on or damage the nerve structures that nourish the tissues of the head and neck.
Cervical migraine is a condition in which the vertebrae compress the nerves located near the vertebral artery.
Useful information The main symptom of the pathology is periodic head pain on the back left or right, which can radiate to the area of the eye sockets and forehead. In addition, patients may experience nausea, vomiting, and acute visual or hearing impairment.
In the absence of adequate treatment, attacks of the disease become more frequent. They are also accompanied by nervousness, irritability, aggressiveness and depression.
Cervical spondylosis is a pathology in which thinning of the lateral and anterior parts of the spinal column occurs. In addition to pain in the back of the head, the disease manifests itself as impaired mobility in the neck, increased pain when tilting and turning the head, as well as problems with sleep.
Spondylitis develops as a result of damage to the cervical vertebrae by bacterial agents. As a result, the spinal column is susceptible to deformation processes in which the neurovascular bundle is compressed. The disease is manifested by local numbness of the skin, increased body temperature, general weakness, and difficulty in neck movements.
In addition, the cause of discomfort in the occipital region can be a syndrome of damage to the vertebrobasilar artery system. This is accompanied by a number of clinical symptoms, including:
- headache on the back left or right;
- loss of visual fields;
- strabismus;
- anisocoria;
- facial asymmetry;
- impaired coordination of movements;
- frequent dizziness;
- dysphagia;
- nausea, vomiting;
- increased sweating.
Myogelosis can also lead to pain in the back of the head. Among the factors that provoke the development of the disease, the most common are:
- drafts;
- stress;
- sleeping in an awkward position;
- passive lifestyle.
The disease is accompanied by pain in the neck and back of the head, which radiates to the back and upper shoulder girdle. In addition, patients may often experience dizziness.
Myositis is an inflammation of the muscle fibers of the neck, which in most cases is bilateral. The disease is diagnosed based on pain that occurs when moving the head and extends to the back of the head and upper shoulder girdle.
Neuralgia of the occipital nerve occurs when the fibers of this structure are damaged. This can be caused by osteoarthritis, gout, constant tension in the neck muscles, benign and malignant neoplasms, inflammatory diseases of the soft tissues of the neck and head, various injuries, as well as insulin-dependent diabetes mellitus.
Neuralgia pain resembles electric shocks that radiate to the eye sockets, lower jaw, neck and ears. Patients describe it as a strong, throbbing pain syndrome. It can occur on one or both sides and intensify during neck movement.
Intracranial increased pressure develops with hypoxia, traumatic brain injury, impaired venous outflow, benign and malignant formations, meningitis, low blood pressure, hydrocephalus, and subarachnoid hemorrhage. In addition to pain in the back of the head, symptoms of the pathology are:
- nausea, possible vomiting;
- increased sweating;
- hyperesthesia to external factors;
- sensations of heartbeat;
- weakness, fatigue;
- weather sensitivity;
- irritability, nervousness.
Diseases of the temporomandibular joint are also accompanied by the presence of pain in the back of the head. Usually the pain is one-sided, radiating to the ear or crown. They begin in the daytime and intensify in the evening. In this case, clicking or crunching may be felt in the area of the affected joint.
Types of headaches in the back of the head
Pain syndrome in the back of the head is divided into 6 types, which depend on the cause of the development of the disorder. These include the following types of pathology:
- vasomotor;
- vascular;
- infectious-toxic;
- tension headache;
- neurological;
- liquorodynamic.
Vasomotor pain is often associated with muscle tension. The pain is usually mild or moderate in intensity. Patients note a feeling of tightness of the head and stiff neck. This type of pathology in most cases is caused by emotional stress and mental disorders.
Vascular pain in the back of the head is observed due to constant spasms or narrowing of cerebral vessels. The pain syndrome is accompanied by characteristic pulsation and a feeling of squeezing.
This form of the disease is observed with migraines, exhaustion of the body or vegetative-vascular dystonia.
Due to impaired vascular tone, the supply of oxygen to the brain tissue is disrupted, which contributes to the development of hypoxia.
The infectious-toxic form of the disease is characterized by progressive intensity. In the early stages, the pain syndrome is localized in a limited area, but over time it spreads to the entire head. Its development is due to the negative influence of pathogenic agents of bacterial or viral etiology, as well as poisoning of the body.
Tension pain occurs during physical or emotional overload. They are accompanied by a feeling of compression of the head, pulsation and irradiation into nearby structures.
Neurological pain is a response of inflamed nerves to external factors. Patients report complaints of intense pain of limited localization. They also experience lumbago in the eye sockets, jaws, ears while performing movements, sneezing, coughing or eating.
A decrease or increase in the level of cerebrospinal fluid leads to pain in the back of the head. The causes of the development of liquorodynamic pain are cysts, hydrocephalus, impaired venous outflow, oncological tumors, as well as pathologies of the meninges.
Diagnostics
If you have unpleasant sensations in the back of your head, it is important to find out why your head hurts in the back. For this purpose, the doctor can prescribe a number of instrumental and laboratory diagnostic methods, among which in this case the most effective are:
- general and biochemical blood test;
- clinical urine analysis;
- Dopplerography of head and neck vessels;
- radiography of the cranial cavity and temporomandibular joint;
- computed and magnetic resonance imaging.
Treatment
To eliminate pain in the back of the head, conservative methods of therapy are used. These include:
- drug treatment;
- wearing a Shants collar;
- alternative medicine.
Drugs
The use of medications allows you to influence the cause of pain, as well as reduce the severity of pain during attacks. For this purpose, the attending physician may prescribe:
- Anti-inflammatory drugs. Among them, the most effective are Ibuprofen, Celecoxib, Ketoprofen, Dexamethasone, Prednisolone.
- Antibacterial drugs. Azithromycin, Tetracycline, Cefuroxime, Doxycycline are used to treat infectious processes.
- Muscle relaxants. If there is a need to relieve spasms of the muscle fibers of the neck, Baclofen, Mydocalm, Sirdalud are used.
- Chondroprotectors. This group of remedies is effective in the presence of problems with the spinal column, the structures of which pinch the nerve fibers. In this case, it is recommended to use Chondroitin, Alflutop and Teraflex.
- Painkillers. Acute pain is relieved with Dexalgin, Ketanov, Amidopyrine or Sulindac.
Shants collar, what is it for?
The use of this device makes it possible to significantly reduce the load on the muscular system of the neck. As a result, pain in the back of the head is relieved.
Doctors often prescribe wearing a Shants collar after surgery or injuries to the cervical spine.
He is able to make your posture correct and securely fix your neck in the desired position.
ethnoscience
Alternative medicine recipes are used in combination with medications and only after the permission of the attending physician. The most effective remedies for treating pain in the back of the head are:
- Lavender oil. To prepare the product, dissolve 1 teaspoon of oil in 3 cups of boiling water. Inhalations should be done for at least 15 minutes. It can also be used to massage the temples along with lemon balm.
- Apple vinegar. This remedy has a number of medicinal properties in the treatment of pain in the back of the head. To prepare the medicine, you need to stir 2 tablespoons of vinegar in 200 ml of water and drink the mixture. This manipulation will significantly reduce the intensity of headaches and also normalize the general condition of the body.
Headache prevention
To prevent the development of pain in the back of the head or reduce the number of attacks, it is necessary to adhere to certain preventive measures that affect the factors contributing to the emergence of pathogenic processes. Among them are:
- sleeping on an orthopedic pillow;
- avoiding hypothermia, stress, heavy physical activity;
- maintaining an active lifestyle
- spending free time outdoors;
- balanced diet;
- regular exercise;
- yoga, meditation classes;
- breaks for 10 minutes every hour of working at the computer;
- controlling blood pressure levels;
- massage of the neck and upper shoulder girdle.
If you have a headache in the back, you need to consult a specialist. Timely diagnosis makes it possible to detect the cause of the development of pathological processes and prescribe the most effective treatment tactics, which will prevent the development of dangerous complications and also preserve the patient’s health.
Source: https://nervy-expert.ru/golovnye-boli/bolit-zatylok/bolit-golova-szadi/
Osteochondrosis
Osteochondrosis is a complex of dystrophic disorders in the cartilage tissue of joints. In the vast majority of cases, this disease affects the intervertebral discs and manifests itself as pain in the neck and upper back, radiating to the arms and back of the head. A distinctive sign of osteochondrosis is the appearance of pain after sleep or sudden movement, including coughing and sneezing.
There is a relationship between cervical osteochondrosis and changes in blood pressure. High blood pressure values do not remain constant, since the increase in pressure is directly related to reflex irritation of the nerve roots and blood vessels. Therefore, blood pressure can rise sharply during the day and drop just as suddenly. An increase in blood pressure is accompanied by headache and decreased sensitivity in the collar area, discomfort in the chest.
The progression of osteochondrosis leads to the formation of intervertebral hernias and marginal bone growths on the vertebral bodies
The pain syndrome due to osteochondrosis is localized in the depths of the neck; when you turn your head, you can hear a characteristic cracking sound. In the early stages, the pain goes away quite quickly, but as the disease progresses it becomes constant.
Diagnostics
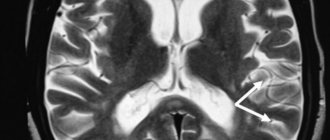
To find out exactly why the back of the head on the right side of the head hurts, you need to make an appointment with a neurologist. After a visual examination, collecting anamnesis, checking reactions and reflexes, the patient’s neurological status is determined, and the probable causes of headache localized in the occipital part of the head on the right are named. To clarify the diagnosis, an instrumental examination is prescribed:
- MRI, CT. Allows you to detect pathological conditions (narrowing, compression of the ducts) that provoked a violation of the outflow of cerebrospinal fluid. The study reveals brain pathologies - tumors, areas of hemorrhage, signs of infectious or ischemic lesions of the brain matter.
- Rheoencephalography. Study of the circulatory system of the brain, blood flow speed, features of blood supply to areas of the head.
- Electromyography. Shows the nature and intensity of bioelectrical activity in muscle tissue.
- Dopplerography. Study of the bloodstream in the area of the back of the head and neck.
Intracranial pressure is measured using a lumbar puncture or ventriculostomy procedure. Certain difficulties in differential diagnosis arise due to the large number of structures studied (intervertebral discs, arteries, meninges, muscle tissue, ligaments) and mechanisms responsible for the development of cephalalgia.
Spondylitis
An inflammatory disease of the spine, called spondylitis, is characterized by the gradual destruction of the vertebral bodies with subsequent deformation of the spinal column. Spondylitis occurs against the background of a bacterial infection - tuberculosis, gonorrhea or syphilis; Bekhterev's disease and in rare cases after injury.
Patients complain of severe pain and muscle stiffness when straining the neck and turning the head. Most often, the pain is nagging in nature and varies in intensity. A characteristic sign is a bowed head, as if a person is looking at his feet. It takes effort to straighten and keep your neck straight.
With spondylitis, there is weakness throughout the body, aching pain in the extremities, and a possible increase in temperature. In addition, the immune system weakens, which leads to frequent colds.
Groups of drugs effective for episodic attacks of pain
Medicines to treat this pathology are non-steroidal anti-inflammatory drugs (NSAIDs). They have an analgesic effect, relieve inflammation, and eliminate swelling.
Often prescribed:
- Ibuprofen-400 mg per day;
- Ketoprofen-100 mg/s;
- Naproxen-500 mg/s;
- Meloxicam-7.5-15 mg/s;
- Celecoxib-200 mg/s.
Most NSAIDs have a negative side effect: with long-term use, they negatively affect the organs of the gastrointestinal tract, including the development of drug-induced gastritis.
Medicines Meloxicam and Celecoxib are new generation drugs that do not have a negative effect on the gastrointestinal tract. The disadvantages of using these drugs include the relatively high price.
Analgesics are often used at home to relieve an attack. They do not treat the disease, but only relieve pain. Drugs in this group are suitable for stopping episodic attacks, but their systematic use leads to the occurrence of abuse syndrome.
During an attack of pain, you can take Paracetamol-100 mg, Citramon, Analgin-500 mg or Mig 200-400 mg.
If the examination revealed the appearance of cephalgia after exercise as a result of increased blood pressure, the doctor will prescribe medications prescribed at an early stage of the development of hypertension. These include: vasodilators, ACE inhibitors, diuretics, calcium channel blockers.
Self-prescribing antihypertensive drugs is unacceptable. Self-medication leads to serious consequences.
For muscle tension, drugs from the group of muscle relaxants are used as part of complex treatment. They relax the spasmodic muscles of the head and neck, relieving pain of a spastic nature, and help restore blood flow.
Often prescribed:
- Mydocalm-150-450 mg per day;
- Sirdalud (Tizanidine) - 4 mg/s;
- Baclofen-15 mg/s.
Nootropic drugs are often prescribed as part of complex treatment: Phenibut, Nootropil, Glycine. Nootropics have an activating effect on brain function and increase its resistance to damaging factors. The drugs improve cerebral circulation and eliminate the consequences of traumatic brain injuries.
For severe attacks, a combination of drugs is used: Sirdalud 2 mg + Aspirin 500 mg or Analgin 250 mg + sedative.
The use of vitamin B complexes has proven itself. Vitamins B1, B6, B12 have a beneficial effect on the central nervous system and restore the structure of nerve tissue. Vitamin complexes are often prescribed: Neuromultivit, Milgamma, Neurovitan.
If attacks of pain recur more than 10 times a month, a course of treatment with Ibuprofen at a dose of 400 mg per day for 2-3 weeks and treatment with muscle relaxants is prescribed for 2-4 weeks.
There is no single scheme for pain relief. Depending on the cause, each patient needs an individual selection of drugs.
Spondylosis
The dominant symptom of spondylosis is pain in the occipital region associated with pinched nerve roots. Its occurrence is caused by bone growths that compensate for worn-out intervertebral discs. These bone growths are called osteophytes and can reach large sizes. In the later stages, with total destruction of the discs, adjacent vertebrae grow together.
The growth of osteophytes causes a narrowing of the spinal canal, where the nerves are located. However, before this happens, the bone spikes irritate the spinal ligaments, which is also accompanied by pain.
Spondylosis can develop slowly, rapidly or in attacks. The most common is the first option, in which, in addition to pain at the base of the skull, a number of typical symptoms are noted:
- headaches caused by compression of numerous vessels in the cervical area;
- stiffness in the neck due to soreness or osteophytes;
- weakening and atrophy of the muscle corset;
- fainting states.
Pain in the collar area is felt when the neck moves, which is explained by stretching of ligaments and nerve endings. Most often, pain appears in the first half of the day due to stagnation of blood in the vertebral arteries. It is extremely difficult to determine the location of the pain, since it radiates (radiates) to the shoulders, eye or ear.
Headache also has its own characteristics and is accompanied by loss of balance, tinnitus and blurred vision. Poor visibility is due to the fact that the visual center is located in the back of the head.
Stiffness is especially pronounced when the osteophytes are large and the affected area is large. The more vertebrae are blocked, the stronger the stiffness and pain. In the later stages of spondylosis, the muscles lose their shape, flatten and atrophy due to impaired blood supply.
With significant compression of the vertebral arteries, blood access to the brain is blocked, and nerve tissue experiences oxygen starvation (ischemia). The result is loss of consciousness - fainting, which usually does not last long. Before fainting, general weakness or nausea may occur.
Causes
More than 35% of the blood flows to the brain through the vertebral arteries, which pass through openings in the vertebrae in the back of the neck. The surrounding bone tissue of the vertebrae protects the arteries from damage. On the other hand, such an arrangement contributes to the compression of blood flow elements in diseases of the spine, accompanied by deformation, changes in the shape of the vertebrae, the appearance of osteophytes, and the proliferation of cartilage tissue.
Such destructive changes are caused by diseases such as osteochondrosis, displacement of the vertebrae as a result of injury, or a hernia in the area of the intervertebral disc. As a result, vertebral artery syndrome develops. This is why there is a headache in the back of the head on the right and disorders such as increased fatigue, asthenia, deterioration of cognitive abilities, visual dysfunction, and rarely speech disorder are observed. Causes of the pathological condition when the back of the head on the right side hurts:
- Degenerative diseases of the cervical spine (osteochondrosis, hernia in the intervertebral disc area).
- Injuries in the cervical spine.
- Infectious diseases (meningitis, encephalitis).
- Diseases of muscle tissue.
- Increased values of intracranial pressure.
- Neuralgia (inflammation of the nerves).
If you have a headache in the back of the head on the right, the discomfort is often associated with long-term arterial hypertension. If foci of ischemia and narrowed vessels are located in the occipital zone, an increase in blood pressure is accompanied by painful sensations in this location. High blood pressure is characterized by problems such as tinnitus, dizziness, and the appearance of foreign objects in the field of vision. A condition where the right side of the back of the head hurts can be caused by the following factors:
- Physical and mental stress, frequent stressful situations.
- Insufficient or excessive sleep.
- Unhealthy, unbalanced diet, characterized by a deficiency of nutrients.
- Sedentary lifestyle.
- Bad habits (alcohol, smoking).
An uncomfortable neck position in women who constantly wear high-heeled shoes can provoke cephalgic syndrome. If cases of headaches in the back of the head on the right are isolated and not associated with illness, simple measures will help eliminate the discomfort - wearing comfortable shoes, a proper daily routine and a healthy lifestyle. Often, episodes when the right occipital part of the head regularly hurts indicate serious malfunctions in the body.
Cervical osteochondrosis is characterized by deformation of the vertebrae, accompanied by compression of blood vessels and nerve endings. As a result, there is a disturbance in blood flow, and a bursting, throbbing pain occurs behind the right ear in the back of the head, characteristic of a condition when blood pressure values sharply increase.
Myogelosis is a violation of blood flow in muscle tissue, occurring against the background of loss of elasticity and softness of muscle fibers. Develops due to chronic muscle overstrain. The processes of muscle contraction and relaxation are accompanied by the destruction and subsequent restoration of protein structures. With intense, prolonged stress on the muscles, protein tissue is not fully restored.
As a result, various physiological and physicochemical disorders occur, which leads to a change in the normal excitability and lability of muscles. Some muscle fibers are in a state of pessimum - inhibition of the activity of nervous and muscle tissue, which develops as a result of intense and frequent nervous stimulation.
The other part is in a borderline state of loss of sensitivity that occurs in response to strong external irritation. The pathological process is called parabiosis. As a result of partial hyaline degeneration, individual muscles are in a state of contracture (tight, inactive).
Myogelosis is characterized by the appearance of persistent, painful compactions in muscle tissue. The disease leads to decreased muscle elasticity, limitation, and stiffness of movements. Persistent pain in the back of the head on the right side of the head indicates serious disorders and the possible development of myofibrosis, in which muscle tissue is replaced by connective tissue.
Cervical migraine
If the right hemisphere of the head hurts, the cause may lie in impaired blood flow in this area. Cervical migraine or Barré-Lieu syndrome is a form of vertebral artery syndrome. It manifests itself as excruciating painful sensations that are associated with compression of the nerve endings surrounding the vertebral arteries in the form of sympathetic plexuses.
Occipital neuralgia
Damage to the nerve fibers of the cervical plexus, accompanied by severe pain, is called occipital neuralgia. The nerves of the cervical plexus innervate the occipital, postauricular, cervical and collar zones. In the case of isolated damage to the occipital nerve, pain occurs only at the base of the skull, but most often other nerve trunks are also involved in the pathological process.
The lesion is usually unilateral, so pain occurs on the right or left of the back of the head. The pain intensifies with movements, turning the head, and even when accidentally touching the occipital nerve. Photosensitivity is another sign of neuralgia: in bright light, the eyes hurt greatly.
With this disease, changes in the skin are observed - redness, increased sweating or dryness.
The development of occipital neuralgia is caused by pathology of the spine in the cervical region, tumor or injury.
Treatment methods
Treatment of pain localized in the right occipital part of the head is prescribed after identifying the causes of the pathology. Depending on the type of disease, the following groups of drugs are prescribed:
- Painkillers, antipyretics.
- Nonsteroidal anti-inflammatory drugs.
- Muscle relaxants (lower muscle tone, eliminate muscle spasms).
- Osteoprotectors (restore bone tissue, inhibit degenerative changes in the bone structures of the spine).
- Nootropic (stimulate cellular metabolism in nervous tissue).
If the pain is associated with an infection, taking antibacterial drugs is indicated. For diseases of the muscle tissue and musculoskeletal system, in addition to drug therapy, physiotherapy, massage in the cervical-collar area, and restorative water procedures are indicated.
Cervical myositis
The neck muscles can become inflamed from hypothermia, unusual physical activity, prolonged exposure to an uncomfortable position, and infections. In most cases, myositis is provoked by drafts, and somewhat less often by overexertion or too intense sports training. Sometimes this pathology is a complication of sore throat, flu or acute respiratory viral infection. Risk factors include nervous stress, which causes tension in the neck and shoulder muscles.
Symptoms of myositis appear several hours after exposure to an unfavorable factor. First, a person feels that one side of the neck is sore, and the pain is clearly localized. Gradually, the pain intensifies and spreads to neighboring areas - the back of the head, collar area, shoulder and shoulder blades.
Any movement of the neck, especially involving the affected muscle, causes shooting pain and makes you literally freeze in one position. Inflamed muscles are tense and hot to the touch, touching them causes acute pain. Adults suffer from myositis somewhat less than children. In young patients, body temperature rises to 38-39° and loss of appetite.
Most often, the course of myositis is acute and rapid. After a few days, or less often weeks, all symptoms disappear. However, there are cases of myositis becoming chronic, when the muscles become inflamed even from minor overload or with every cold.
Important: recurrent myositis requires mandatory examination by a rheumatologist or infectious disease specialist, since the disease can cause systemic damage to connective tissue and the presence of parasites in the body.
The back of the head hurts on the right side: causes and treatment
Headache is known to many people. If it is not constant, but occurs sporadically, then this phenomenon can be considered normal.
But when the back of the head on the right side often hurts, you should find out the reasons for the pain. They can signal serious problems.
Symptoms
If you have a headache on the right side of the back of the head, this should alert you; symptoms associated with the disease may appear. Basically, they are typical for pathologies that are accompanied by headaches:
- darkening in the eyes, roaring in the ears;
- nausea leading to vomiting;
- limbs begin to go numb;
- I feel dizzy and lose coordination in space.
All these signs can be harbingers of an impending cerebral hemorrhage.
When there is a headache in the back of the head, this condition also differs in the form of its occurrence. Pain happens:
- paroxysmal;
- pulsating;
- increasing with changes in head position.
But usually right-sided pain in the back of the head is characterized by pressing sensations. Depending on the reason that determines why the back of the head on the right side hurts, the doctor prescribes treatment.
Causes of pain syndrome
Pain in the occipital part of the head on the right usually signals an inflammatory process on this side. The back of the head hurts on the right in these conditions:
- Neuritis of the occipital nerve, which is located on the right side of the head. Occurs from hypothermia or prolonged uncomfortable body position.
- Damage to the vessels of the vertebral artery passing along the spinal canal on the right. The pain is paroxysmal. Shooting sensations. Between attacks there is pressure on the occipital region.
- Myelogelosis of the trapezius muscle on the right. These seals that occur in the neck muscles lead to severe pain in the back of the head.
- Cervical spondylosis. With this pathology, the lateral vertebral processes begin to grow to the side. The disease develops mainly in older people who are physically inactive. The pain syndrome is present around the clock.
- Intracranial pressure. With this pathology, pain can be localized in any part of the head. Accompanied by nausea.
- Epidermal cyst. A hard lump on the back of the head is often a cyst. It needs to be removed urgently. The painful sensations are debilitating.
- Vascular spasm. There is a pulling sensation, and the occipital region becomes numb.
- Pain in the occipital part of the head on the right also occurs with migraine, but with additional symptoms, which are manifested by a buzzing in the ear or a pain in the right eye.
- If the occipital region of the head hurts in the presence of vascular dystonia, then over time the pain will change its location and concentrate in the area of the right temple.
- If nausea occurs with occipital pain, then the person has hypertension or a concussion.
- We cannot exclude injuries, which quite often cause right-sided pain in the occipital area.
There are many reasons that cause pain symptoms in the back of the head. These are both serious pathologies and an incorrect lifestyle. To prevent the occurrence of such conditions, it is necessary to adjust your daily routine, review your diet and exercise.
Diagnostic methods
If the back of the head hurts severely on the right side, you should immediately consult a neurologist. After listening to complaints and conducting a visual examination, the doctor refers you for an in-depth examination.
- You need to donate blood and urine for analysis.
- You should check your cholesterol levels.
- It is advisable to conduct daily blood pressure monitoring.
- X-ray. Allows a thorough examination of the cervical spine. X-rays can reveal cracks in the occipital bone, the formation of tumors and unwanted curvature of the cervical spine.
- Study of the vessels of the brain and neck. This measures the intensity of blood flow. Prescribed to eliminate migraine and high intracranial pressure.
- CT scan. It resembles an x-ray, but pictures are taken in different projections and the data is processed on a computer. Makes it possible to see anatomical formations much better. For occipital pain, this study is performed if there is a suspicion of tumor development.
- MRI. It is not carried out if there are metal objects in the body. Not recommended for people with mental disorders and pregnant women. The study is very informative and is carried out if other methods have not identified the cause of the pain.
- 8. Neuromyography. The study clarifies the diagnosis.
If painful sensations are provoked by external factors and not diseases, they often disappear on their own.
How to treat
The formation of treatment tactics is influenced by the cause of pain in the occipital part on the right. Only by eliminating the source of pain can we hope for a positive treatment result.
The problem should be eliminated at the first stage of the disease, otherwise the intensity of pain in the back of the head will increase. The following types of therapy are mainly prescribed:
- Painkillers. If pain in the back of the head on the right is caused by an inflammatory process, then take Diclofenac, Nurofen and Nimesil.
- Nootropic drugs. Phenotropil or Piracetam will improve the functioning of the nervous system and restore nerve fibers.
- Muscle relaxants. Muscle tone is normalized by Mydocalm and Tizarlud.
- Warming agents. They relieve inflammation caused by neuritis or myositis.
- Classic massage. It is performed if a headache in the back of the head is caused by cervical osteochondrosis. Since the cervical spine is unstable, only the shoulders are massaged.
- Cranial osteopathy. Normalizes the outflow of cerebrospinal fluid during intracranial hypertension, and relieves tension from the walls of blood vessels.
- Physiotherapy. The procedures successfully relieve acute inflammation. Modern means are available: electrophoresis, laser and magnetic therapy.
- Acupressure. Relieves pain and relaxes muscles in the cervical area.
Complex treatment using these techniques is carried out after a thorough examination. Self-medication will not alleviate the condition, but will significantly increase the risk of the pathology becoming chronic.
Some diseases require surgery. This happens rarely when it is necessary to remove a malignant neoplasm.
Folk remedies
If it is not possible to take medicine, then you can resort to traditional methods. With their help, it is quite possible to relieve pain or even completely eliminate pain.
- Compresses with cabbage leaves on the back of the head.
- Tea with linden or sage.
- Rubbing lavender oil onto the right side of the back of the head.
- Warm compresses to the earlobes.
- St. John's wort decoction.
- Infusion of coltsfoot.
It should be clarified that these methods will help if a person has already been diagnosed. But in general, the effectiveness of folk recipes is relatively low. It is unlikely that medicinal herbs will help with meningitis or a migraine attack.
Prevention
To avoid right-sided pain in the back of the head, you should constantly and correctly follow the recommendations for preventing pain. They are elementary:
- Overexertion should be avoided, but you should not completely give up exercise.
- Avoid drafts and sudden hypothermia.
- It is advisable to purchase an orthopedic mattress.
- Avoid smoking.
Such preventive measures will minimize the manifestation of right-sided pain in the occipital region. When the right side of the head in the back of the head is bothered, it is not just stress or incorrect body position during sleep.
This is often a serious pathology requiring emergency treatment. If the back of the head begins to constantly hurt, then you should not drown out the pain syndrome with analgesics, but rather begin adequate treatment.
Myogelosis
The term “myogelosis” translates as “muscle thickening” formed in the cervical region. There can be several causes of myogelosis - osteochondrosis, spondylosis, previous myositis, high physical activity and hypothermia (drafts). Congenital vascular abnormalities and atherosclerosis also contribute to the development of the disease.
The immediate cause is poor circulation and insufficient oxygen supply to the muscles. This leads to a compensatory reaction with the replacement of normal tissue with sclerotic tissue, which is more resistant to oxygen deficiency.
The leading symptom of myogelosis is pain, which is most often very severe. The growth of the seals causes compression of the nerve roots and blood vessels, as a result of which the blood supply to the brain is disrupted. The subcutaneous nodules are painful to the touch, stiffness is felt in the neck muscles, and movements are limited.
Headache treatment
The Clinical Brain Institute has developed comprehensive headache treatment programs. They are adapted individually for each patient, depending on the exact diagnosis, the person’s age and other characteristics. The complex of treatment measures may include the following techniques:
- drug treatment - consists of taking painkillers, anti-inflammatory drugs, specific muscle relaxants (muscle relaxants), antibiotics;
- physiotherapy - a set of techniques for improving blood circulation and innervation of certain areas using electric current, magnetic radiation, thermal and other procedures;
- nerve blocks - injections of hormonal anti-inflammatory drugs in combination with local anesthetics;
- surgical methods are prescribed for the removal of tumors, hernias of the cervical spine, as well as for the treatment of traumatic brain injuries.
The Clinical Brain Institute offers outpatient and inpatient treatment. There are all the necessary conditions for conducting a full diagnosis and for effective treatment of different types of headaches. The center is equipped with modern equipment and works with the participation of specialists of a narrow and broad profile. Here you can get competent advice, as well as undergo all prescribed examinations.
Clinical Brain Institute Rating: 5/5 — 1 votes
Share article on social networks
Increased intracranial pressure
The first symptom of intracranial hypertension is dilation of the eye pupils that do not respond to light, drowsiness and persistent yawning. Weakness in the limbs and facial muscles may occur. Further, these symptoms are accompanied by pain in the back of the head or throughout the head, which occurs mainly in the morning and subsides in the evening.
Pathology may also manifest itself:
- pain in the eyes;
- gagging not related to food;
- unabating hiccups;
- decreased attention;
- changes in blood pressure;
- excessive sweating;
- increased heart rate;
- fatigue, lethargy;
- dark circles and dilated capillaries under the eyes;
- blurred vision and inability to focus.
Why does intracranial pressure increase? The cause may be congenital vascular pathology, endocrine disorders, taking certain medications, infectious diseases and tumors.
Causes of pain on the right side of the head
Cephalgia, or just a headache, is familiar to everyone. Its causes are varied and sometimes indicate serious health problems. Unilateral pain is less common, but is also quite often present in a person’s life, causing him significant discomfort. What does pain in the back of the head on the right indicate, why does it occur, what factors influence its appearance?
People should know the origins of pain in this part of the head so as not to miss serious diseases and start treatment on time.
Origin of pain
The nervous system is the most complex and sensitive mechanism of the human body. It is this that makes it possible to feel pain and signals that a failure is occurring in a coherent system.
Pain sensations are generated in pain receptors (nociceptors) - sensory neurons.
Nerve fibers are located in the central and peripheral parts of the body and are designed to send signals to the brain, where information processing occurs.
To generate a signal, a certain degree of irritation is necessary, so sensations appear when the process has already developed.
Causes of headaches
There are no pain receptors directly in the brain, so it itself does not give the sensation of pain. But its shell is an extremely sensitive instrument; it contains intracranial nerves and spinal cord roots.
The superficial receptors of the skin, tendons, oral cavity, middle ear, and neck are also responsible for the feeling of pain.
Therefore, it is easy to conclude that there are many reasons for the formation of cephalalgia in the posterior part of the head; these can be internal and external factors.
Cephalgia can spread throughout the head, right and left, front and back. The area of localization of the pain syndrome is associated with the source of neuronal irritation, which provokes negative sensations.
The set of factors influencing the appearance of pain in the right side of the head is divided into groups:
The first group includes pain associated with the cervical spine:
- congenital pathologies of the spine;
- injuries;
- vertebral artery syndrome (abbreviated as SPA).
The second group is factors not related to the spine:
The third group of problems affects the vascular and nervous system:
- arterial hypertension;
- its complication is stroke;
- changes in intracranial pressure;
- neuralgia and neuritis.
Cervical migraine (SPA)
The disease affects almost a third of the world's population, which indicates its prevalence. The pain syndrome indicates that the posterior and lateral parts of the brain suffer from a lack of oxygen due to a narrowing of the lumen of the vertebral artery. What factors influence the development of pathology?
- congenital vertebral anomaly;
- injuries;
- atherosclerotic lesion of the vessel;
- osteochondrosis and osteophyte;
- muscle spasm.
External manifestations
Since there are several factors leading to changes, the manifestations of symptoms are diverse:
- With atherosclerosis and osteochondrosis, symptoms develop gradually. The body has a high ability to replenish the lack of blood supply, so it will take several years until symptoms become apparent. At first, the sensations are insignificant, appear periodically, pain in the occipital part is concentrated on both sides. As the process progresses, the symptoms become brighter and occur more often. If the first signs of illness are left unattended, they become unbearable.
- With osteophytes, bone tissue grows, usually on one side; if the anomaly is located on the right, that is where the pain will occur.
- During the period of increased pressure, the muscles spasm, therefore, the appearance of pain on one side is characterized by the frequency of attacks.
During SPA pain syndrome, pain is accompanied by:
- dizziness:
- ringing in the ears;
- blurred vision;
- hearing loss;
- sometimes the palate and tongue become numb;
- sometimes the pain radiates to the ear, eye or temple;
- at the site of pain, skin sensitivity is increased;
- a burning sensation appears.
During severe attacks, loss of consciousness occurs.
Treatment
The choice of therapeutic tactics for SPA is associated with the reasons for the development of the process.
Conservative treatment:
- anti-inflammatory drugs are prescribed: Diclofinac, Meloxicam;
- antispasmodics: Mydocalm; Spasmalgon; Serdalud;
- drugs that increase brain perfusion: Trental, Cinnarizine;
- To eliminate oxygen starvation of brain tissue, Piracetam, Glycine, and a complex of vitamins are prescribed.
Physiotherapeutic treatment:
- represented by hardware methods;
- massages, therapeutic exercises;
- water procedures.
Surgical intervention. Includes removal of growths, vascular shunting, and restoration of vertebrae.
Myositis
Cervical myositis is of an inflammatory nature, occurs in the muscles of the neck, and often causes severe pain in the back of the head on the right. Provoking factors for its appearance include:
- incorrect neck position;
- hypothermia;
- muscle spasm;
- bacterial infection (rheumatic fever, tonsillitis, sore throat)
- helminthic infestation (trichinosis);
- systemic diseases (diabetes, gout).
Myositis is expressed by asymmetric pain syndrome:
- for example, pain appears in the neck and back of the head on the right side;
- radiates to the shoulder, ear or temple;
- acute myositis is manifested by swelling of the inflamed muscle and skin surface.
Treatment includes a set of measures aimed, inter alia, at eliminating the circumstances contributing to the development of the inflammatory process:
- ointments (Finalgon) are used to reduce pain;
- anti-inflammatory drugs (Reopirin) are used;
- for purulent processes, antibiotics are recommended;
- anthelmintics.
Myogelosis
A disease when an area of healthy muscle tissue becomes denser due to insufficient blood supply and degenerates into connective tissue.
Occurs due to:
- osteochondrosis;
- hypothermia;
- cervical migraine;
- prolonged or severe physical overstrain (in athletes due to professional duties);
- rachiocampsis.
Often develops in the neck area and manifests itself:
- pain that increases when turning the head;
- with a one-sided course, it can occur asymmetrically in the occipital part of the head on the right;
- at the site of the process, muscle tissue becomes dense;
- a person’s movements are constrained or limited;
- in severe cases, contracture develops.
It is preferable to treat the disease at an early stage, before the changes lead to degenerative processes in the muscles.
The following will help restore blood circulation:
- massage, gymnastics;
- ointments;
- measures to straighten posture;
- warming up;
- hirudotherapy;
- if inflammation is present, NSAIDs are used;
- For severe pain, use painkillers.
When the process becomes irreversible, surgery is indicated.
Intracranial pressure (ICP)
A headache in the back of the head is often evidence of an increase in intracranial pressure. The narrowing of blood vessels in the brain is caused by the following factors:
- The development of anomalies is caused by pathologies of pregnancy and complications during childbirth (hypertension and edema during pregnancy, entanglement of the umbilical cord, difficult childbirth).
- Tumor formations in the brain and hematomas.
- Taking medications.
- Infectious diseases of the brain.
- Operations and injuries.
- Endocrine and systemic diseases.
Typically, manifestations of ICP spread throughout the entire head, the pain is bursting in nature, but in the case of subarachnoid hemorrhages due to rupture of an aneurysm or strokes, they acquire a local course. It seems that the person received a sharp blow to the back of the head. Then there is a severe headache in the back of the head, radiating to the temple.
Characterized by symptoms:
- nausea and vomiting;
- dizziness;
- speech and hearing impairment is observed;
- sometimes the pain is accompanied by loss of consciousness;
- paralysis
If the pain occurs suddenly, its manifestation is vivid, the person speaks slurred or cannot utter a word, loses consciousness, an ambulance should be called immediately. Symptoms indicate the severity of the process, and delay is sometimes fraught with coma or death.
Depending on the reason affecting the ICP, treatment is prescribed:
- during drug therapy, diuretics are used;
- hormonal medications;
- sometimes antibiotics.
Physiotherapy, massage, and surgical treatment are used.
Neuritis
With prolonged compression of nerve tissue, neuritis develops. The occipital region suffers when the peripheral nerve in the spinal column is damaged. This happens due to:
- incorrect head position;
- osteochondrosis and osteoarthritis;
- hypothermia;
- infectious diseases;
- endocrine problems and diabetes;
- due to salt metabolism disorders;
- injuries;
- obesity.
With inflammation of the occipital nerve, the unilateral pain syndrome is minor and dull in nature. Sometimes it starts to hurt quite badly, and shooting occurs. The sensation intensifies when tilting or turning the head, straining, and skin sensitivity increases.
Drug treatment is used, and it is also aimed at reducing the influence of primary factors influencing the development of neuralgia:
- local treatment is used
- anti-inflammatory and painkillers:
- anticonvulsants;
- physiotherapeutic procedures.
Other reasons
Pain in the back of the head also occurs for other reasons not related to diseases of the spine and blood vessels. The following can contribute to the development of an attack of cephalgia:
- nervous disorders;
- stress;
- overvoltage;
- physical activity that affects neck muscle tension;
- improper organization of sleep;
- poor nutrition, since it has been proven that some foods provoke headaches;
- alcohol and smoking.
If the root cause is not eliminated, the pain syndrome becomes chronic, which creates the preconditions for the development of complex diseases.
First aid
To prevent pain in the right and left side of the head from bothering you, you should first eliminate the factors influencing the development of the condition:
- avoid overloading the neck area;
- avoid static poses and sudden neck movements;
- during working hours you need to take a short break and do gymnastics;
- get rid of bad habits;
- balance the diet;
- regulate sleep and rest patterns;
- eliminate stress.
If the back of your head hurts, it is better to lie down and relax. When the origins of the pain syndrome are known, for minor symptoms you can use home remedies:
- rub the painful area with ointment;
- take a painkiller:
- drink soothing tea with chamomile or mint infusion.
Regardless of the etiology of pain in the right side of the head, massage and warming procedures are contraindicated during the period of exacerbation. These actions can provoke an increase in symptoms, in some cases they can threaten the patient’s life.
When the pain is severe, the syndrome increases, and cephalalgia is accompanied by additional symptoms: fever, vomiting, convulsions, you should immediately consult a doctor.
If pain in the back of the head begins to bother you more often, there is no need to postpone the examination; a timely visit to the doctor will help to avoid serious problems and suffering in the future, and stop the development of the disease at an early stage.
Myogelosis
Myogilosis is a disease that is characterized by the degeneration of part of normal muscle fibers into connective tissue (hyaline degeneration) against the background of a constant lack of blood flow in the muscle tissue.
Causes:
- local hypothermia;
- prolonged exposure to an incorrect position, usually for years (illness of drivers, dentists);
- significant curvature of posture.
Manifestations:
- most often the disease occurs on the back of the neck and is characterized by pain in the occipital region of the head;
- sometimes asymmetry of pain is possible;
- local compaction of muscle tissue, stiffness and limitation of movement or its complete absence (contracture).
How to treat?
- restoration of blood flow in the muscle in the early stages of the disease - maintaining correct posture, breaks for gymnastics, massage and manual therapy, treatment with leeches, warming up;
- elimination of inflammation, if any, by using ointments with NSAIDs;
- painkillers for severe pain;
- surgical treatment in very advanced cases.
Neuritis, neuralgia
Neuritis is pain associated with inflammation in the nerve tissue.
Neuralgia is pain that occurs without an inflammatory process.
Provocative factors:
- prolonged uncomfortable neck position;
- hypothermia;
- osteochondrosis and osteoarthritis;
- infections;
- diabetes mellitus and gout.
Manifestations of neuritis and neuralgia of the occipital nerve:
- pain in the back of the head of varying degrees of intensity (from slight to severe, often in the form of a feeling of “lumbago”);
- increased pain when turning and tilting the head;
- pain is often one-sided;
- increased skin sensitivity.
How to treat?
- medicinally:
- local ointment medications with NSAIDs;
- painkillers, anti-inflammatory, anticonvulsants;
- blockade of nerve plexuses with dexamethasone, metipred, novocaine;
- physiotherapy (massage, warming procedures).
Disease prevention:
- it is necessary to maintain normal posture and frequently change position when sitting;
- If possible, maintain an active lifestyle;
- healthy eating;
- sleep at least 8 hours a day;
- morning exercises;
- if possible, use special mattresses and pillows;
- avoid sudden turns and tilts of the head;
- Avoid hypothermia and drafts.