When an expectant mother finds out that she is pregnant, her life takes on a completely different meaning. Now you need to take care not only of yourself, but also of the little lump that already lives under your heart. The first thing a woman should do is register with a good specialist whom she trusts in order to be sure of the normal course of pregnancy.
Of course, the last thing young parents want is to think that their child may not develop properly. But if problems are still discovered, do not despair. Gather all your will into a fist and do everything possible to ensure that the child is born healthy.
Neural tube in the fetus - what is it?
Many expectant mothers who are just learning the good news about pregnancy rush to study all the available literature about the upcoming birth. That’s when they come across the information that on days 19-22 from conception, the neural tube in the fetus begins to form. What it is? After all, an adult simply does not have such an organ. The answer is simple: the fetal neural tube is the primary form of development of the nervous system, including the brain and spinal cord. The open nerve compartment is a platform for the formation of the anterior, middle and posterior bladder.
Phylum Chordata. Subtype Skullless. Lancelet
- Aromorphoses
Chord
Neural tube
Intestinal tube
- Representative: lancelet
- Habitat: seas
- Lifestyle: free-living, sedentary, burrows into the ground at the bottom
- Fins: dorsal, caudal (lanceolate), subcaudal
- Internal skeleton: the notochord appears for the first time
The notochord (consists of acellular supporting tissue) stretches from the anterior end of the body to the posterior
Skull – missing
- Limbs: none
- Circulatory system: closed; 1 circle of blood circulation
; blood is colorless
Heart – absent; its f: performed by the abdominal aorta (under the pharynx)
Abdominal aorta - branchial arteries - carry venous blood to the respiratory organs Arterial blood - to the dorsal aorta - to all organs and tissues
Venous blood - from organs and tissues through the 4 cardinal veins - into the abdominal aorta
- Digestive system:
Oral opening (surrounded by 10-20 pairs of tentacles) – perioral funnel – pharynx – peribranchial cavity – intestine (has a blind outgrowth, f: liver) – anus
Stomach – absent;
Nutrition – passive, by water filtration
- Excretory system: 100 pairs of nephridia -
tubes, on the sides of the pharynx;
One end of the nephridium - as a whole, the other end - into the peribranchial cavity
- Respiratory system: pharynx with gill slits;
Water – into the mouth opening – pharynx – gill slits – peribranchial cavity – atriopore (the opening where the peribranchial cavity communicates with the external environment) – external environment
Gas exchange - through the skin and when washing the gills with water
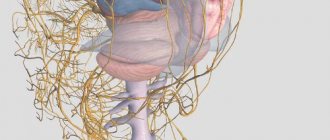
- Nervous system: the neural tube appears for the first time
There is a neurocoelus, expanding towards the anterior end
From the neural tube - peripheral nerves
- Sense organs: poorly developed;
There are pigment cells
(Hessian eyes) – perceive light stimulation (along the entire length of the neural tube)
Tactile cells
– on the skin;
Olfactory fossa
- chemical sense organ
- Body covering: skin - single-layer epithelium and gelatinous dermis
There are skin glands (they secrete mucus)
- Reproductive system: dioecious
On the sides of the pharynx - gonads (sex glands) - do not have their own ducts
Fertilization - external
- Reproduction: sexual
Sex cells – into the peribranchial cavity – through the atriopore – into the water – fertilization occurs – development with metamorphosis – egg – larva – 3 months leads a pelagic lifestyle (in the water column - pelagial) - swims with the help of cilia covering the body
- Development:
Development with metamorphosis
– egg – larva – leads a pelagic lifestyle for 3 months (in the water column - pelagic zone) - swims with the help of cilia covering the body
- Body symmetry: bilateral
- Muscles: transversely striped (two longitudinal stripes, on the sides of the chord)
- Origin: from annelids
Terrible diseases that are incompatible with life
As we understand, one of the most important stages in the origin of life that occurs during pregnancy is the formation of the neural tube, from which the baby’s brain and spinal cord will very soon develop. But sometimes it happens that the process of closing the upper section is disrupted, resulting in anencephaly (absence of the brain in the fetus). If there is a violation in the closure of the lower part of the neural tube, spina bifida occurs. Unfortunately, both of these pathologies are incompatible with life, but they are very rare. Statistics confirm that this disease affects one fetus in a thousand.
Sometimes there are situations when the neural tube in the fetus begins to develop incorrectly. What does this mean and should I worry about it?
The role of folic acid in the prevention of developmental defects
A deficiency of folic acid in the body contributes to disturbances in the formation of the neural tube, the development of atherosclerosis, coronary heart disease and the occurrence of mental disorders.
Folic acid
Pregnant women are especially susceptible to folic acid deficiency, and the need for folic acid increases 2-4 times during this period. An insufficiently enriched diet in pregnant women has an impact on the increase in the number of miscarriages, numerous pregnancy complications, decreased body weight at birth of the newborn, placental hypoplasia, as well as the formation of various birth defects in the embryo and fetus.
Even a slight deficiency of folic acid can be harmful to the health of women of childbearing age and in the early months of pregnancy, and also pose a risk of birth defects in the developing fetus.
MAKE AN APPOINTMENT
Abortion and contraception clinic in St. Petersburg - department of the medical gynecological association "Diana"
Make an appointment, tests or ultrasound via the contact form or by calling +8 (812) 62-962-77. We work seven days a week from 09:00 to 21:00.
We are located in the Krasnogvardeisky district, next to the Novocherkasskaya, Ploshchad Alexander Nevsky and Ladozhskaya metro stations.
The cost of a medical abortion in our clinic is 3,300 rubles. The price includes all pills, an examination by a gynecologist and an ultrasound to determine the timing of pregnancy.
Share link:
What are the types of neural tube defects?
Neural tube defects are a number of individual defects that can develop in the fetus. Fortunately, such deviations are quite rare.
It is important to understand that fetal neural tube pathology is not a modern disease that is caused by current human living conditions. As confirmed by the records of paleontologists who conducted relevant research, defects in the development of the spinal cord or brain (this confirms the incorrect development of the skull and spine) were found in the remains of a person who lived 7,000 years ago.
The first mentions in scientific medical works, on the basis of which, one might say, neurosurgery began to develop, were noted in the works of Hippocrates. The Italian anatomist Morgagni Batista was perhaps one of the first to give approximate descriptions of neural tube defects. At that time, of course, such pathologies were not subject to treatment, because medicine was still at a very low level of development.
Reasons for the development of such problems
Unfortunately, sometimes there is a defective neural tube in the fetus. What kind of pathology is this and what causes it? Let's find out the reasons for the deviation from the norm.
So, on the 19-20th day after conception, a specific plate is formed in each fetus - the very first form of development of the human nervous system. On days 20-22, it should begin to close, resulting in the formation of the neural tube in the fetus. The fact that everything is going according to plan is confirmed by the absence of pathologies of the nervous system in the child who is born. If, on the 23rd day from conception, the neural plate has not completely closed into a tube, the fetus will develop problems with the spine. This can be caused by increased pressure in the spinal larkspur, which was observed in the first trimester of pregnancy.
One of the most common causes of such pathologies are viral infections, radiation received by a future mother who has cancer, as well as environmental factors. But more often such deviations occur in pregnant women who also had a neural tube defect. High risk is caused by genetic inheritance.
Reproduction
The lancelet is a dioecious animal. The release of mature eggs and sperm occurs immediately after sunset, fertilization is external (in water). The larvae live in the water column for about three months, feeding on planktonic animals, and then sink to the bottom. The lancelet reaches sexual maturity in the second (third) year of life.
The peculiarities of the embryonic development and structure of the lancelet were studied by the Russian evolutionary zoologist Alexander Onufrievich Kovalevsky (1840-1901), who established the proximity of these animals to the most ancient ancestor of vertebrates.
External factors that can become the root cause of the development of the defect
Yes, a genetic predisposition to such a defect significantly increases the risk of its occurrence. But today doctors consider radiation to be a very common cause of the development of such a pathology (the expectant mother can receive radioactive exposure not only during treatment, but also simply while living in an area contaminated with radionuclides). Pesticides, petroleum products and various types of synthetic fertilizers also cause the neural tube in the fetus to develop incorrectly.
Today, many people know that consuming genetically modified food is very dangerous for human life. However, not everyone knows that if an expectant mother abuses such products, she thereby increases the risk of developing a fatal pathology in her baby. Even a hot bath that a woman takes at the beginning of pregnancy can trigger the occurrence of such a defect.
Doctors also attribute unbalanced maternal nutrition to the root causes of the development of a neural tube defect. A woman should pay special attention to herself throughout the entire period of pregnancy. In the event that several of the above factors are detected in the life of the expectant mother, you should be prepared for the fact that the pregnant woman will be included in a high-risk group for giving birth to a child who will have a neural tube defect.
What happens to the fetus when it has such a disorder?
In order to understand how a neural tube defect develops in the fetus, you need to at least in general understand what the process of embryogenesis is.
So, the first week of pregnancy ends with the formation of the embryonic nodes. The second is the period of formation of axial organs in the fetus, when extraembryonic parts are actively developing. As already mentioned, the third week is the time when the neural tube is formed from a special plate. The first three weeks are the period of primary neurulation. The secondary one occurs within 4-7 weeks from the moment of conception.
Already during this period of time, disorders, that is, spinal dysraphism, may occur. Pathology of the fetal neural tube, which develops into malformations of the lumbosacral part of the future spine, can occur only during the period of secondary neurulation. It now becomes clear that improper development of the neural tube in the fetus begins in the first weeks of pregnancy, which is why treatment of such diseases occurs in the form of preventing the development of serious defects. Thus, therapy should begin before pregnancy and continue during the first weeks of gestation.
Neural tube defects have their own symptoms
Like any disease or disorder of proper development, defective formation of the neural tube in the fetus has its own symptoms.
Modern medicine includes the following concepts as signs of spinal dysraphism:
- Hidden spinal cleft: such a defect is most often located in the lumbosacral region. It is quite dangerous, since it simply has no clinical symptoms. This pathology is discovered absolutely by accident, for example, after an X-ray of the spine. There are no significant changes in the skin; pigment spots or wen occasionally appear. Such a hidden cleft is nothing more than a poorly closed arch of one of the vertebrae. This disease has a number of consequences, which include bedwetting, significant impairment of correct posture, weakness of the leg muscles, pain in the lumbar region and even deformation of the feet. This is why it is so important to monitor whether the formation of the neural tube in the fetus occurs correctly.
- Open cystic clefts: These are also called true spina bifida. They may appear in the form of partial protrusion of the dura mater. The content of such hernias is cerebrospinal fluid, that is, cerebrospinal fluid. This serious pathological process can spread to two or three vertebrae. Many people who were born with this defect have lived long and happy lives. In such cases, practitioners recommend using surgical intervention only when there is a growth of a true spina bifida. If such a bone defect involves 3-5 vertebrae, then patients will already experience muscle weakness and urinary incontinence. But, unfortunately, the most common violation occurs, which involves 6-8 vertebrae. The skin on such a hernia is too thin, and the sheet of the pial membrane is visible through it. This is a very severe form of the defect, which often ends with rupture of the hernial sac and leakage of cerebrospinal fluid.
- The extreme degree of deformity is considered to be non-fusion of the spine and soft tissues, which is accompanied by defective formation of the spinal cord. Such a defect is practically incompatible with life.
An interesting fact is that the location of such hernias in 90% of cases falls on the lumbar region, and very rarely it is observed in the thoracic or cervical region. This state of affairs is explained by the fact that if a defect develops in the fetus, then the pregnancy most often ends in spontaneous abortion (miscarriage). Such embryos simply die, since their further formation is practically impossible.
Possibilities of echography for diagnosing fetal spinal defects
Spina bifida is a defect in the development of the neural tube, which is a splitting of the spinal canal (spinal dysraphism), often with the formation of spinal cord herniations.
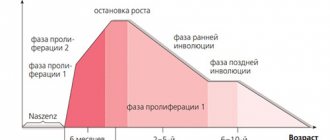
The central nervous system is formed from the ectoderm in the 3rd week of embryonic development. The length of the embryo during this period is only 15 mm. The sheets of ectoderm come together and form the neural groove, and then, coming closer, the neural tube (Fig. 1). A bone ring is formed around it. Normally, closure of the neural tube occurs by the 28th day of gestation. However, when closure is impaired, defects such as anencephaly, encephalocele and spina bifida are formed (Fig. 2).
Rice. 1.
Stages of embryogenesis of the neural tube: transverse schematic section.
a)
Medullary plate.
b, c)
Medullary groove.
d, e)
Neural tube: 1 - horny leaf (epidermis); 2 - neural ridges.
Rice. 2.
Formation of a neural tube defect.
Typical for all types and forms of spinal dysraphism is their posterior location with a defect in the posterior semi-ring of the spinal canal. It is extremely rare (less than 1% of cases) that a cleft forms on the anterolateral surface of the canal, and anterior spinal hernias occur.
The anterior and posterior vertebral clefts can run along the midline and may also be located asymmetrically. In some cases, the gap is located obliquely. If vertebral bifida occurs in the midline, the spinal deformity may be slight or not noticeable at all. However, with an asymmetrical and oblique arrangement of the gap in combination with other anomalies of vertebral development (for example, unilateral microspondylia of half a vertebra, anomaly of the articular processes), severe spinal deformity develops.
Most often (up to 70% of cases) spina bifida is localized in the lumbosacral region, in 21% in the thoracic region and in 9% in other localizations [1].
There are three variants of spina bifida
- Spina bifida occulta.
This option is also called “hidden”, since there is no visible external defect. Hidden spinal clefts are usually localized in the lumbosacral region and, as a rule, do not manifest themselves clinically. They are often an incidental “finding” during an X-ray examination of the spine or MRI. The anatomical essence of spina bifida is incomplete fusion of the vertebral arch. This is the most favorable variant of spina bifida. Sometimes in the area of the defect there are “markers” or skin stigmas in the form of lipomas, cystic and/or solid masses, areas of abnormal hair growth, hyperpigmentation. With closed defects, vertebral anomalies, foot deformities, and an abnormally low conus also occur. The closed variant of spina bifida is not accompanied by Arnold Chiari II syndrome, ventriculomegaly and other intracranial changes [2]. - Meningocele.
A meningocele is a spina bifida with protrusion into a defect in the dura mater, but without involvement of neural structures (Fig. 3). The contents of the hernial sac are the meninges and cerebrospinal fluid; its shape is usually stalk-like with a narrowed stalk. The bone defect usually involves two or three vertebrae. Clinical manifestations of the disease are variable and range from asymptomatic to dysfunction of the pelvic organs, motor and sensory disorders. This variant of spina bifida is rare. - Myelomeningocele.
This is the most severe form of spina bifida, with the involvement of the membranes, spinal cord and its roots in the hernial sac. The bone defect is usually wide and extended, covering from 3 to 6-8 vertebrae. The degree of neurological defect is always severe paraplegia of the lower extremities, sensory disorders, neurogenic bladder and intestinal paresis. It is this form of spina bifida that occurs most often - about 75% of all forms [3-5]. In almost all cases, myelomeningocele is combined with Arnold-Chiari II syndrome. Thus, detection of signs of Arnold-Chiari II malformation in the fetus is a marker of the presence of spina bifida. In addition, in 70-80% of cases, the fetus develops hydrocephalus [5, 6].
Rice. 3.
Diagram of fetal spinal defects.
a)
Meningomyelocele.
b)
Meningocele.
We present clinical observations demonstrating the capabilities of echography in diagnosing fetal spinal defects.
Clinical observation 1
Patient K., 26 years old, came to the clinic at 23 weeks of pregnancy. First pregnancy. The study was carried out on the Accuvix-XQ device (Samsung Medison) using the 3D/4D surface volumetric reconstruction mode. Fetometry indicators fully corresponded to the gestational age. During scanning of the spine in the frontal and sagittal planes, an angular deformity of the spine in the thoracic region, extending about three vertebrae, was revealed. In the transverse scanning plane, no disruption of tissue structures or integrity was detected. 3D/4D reconstruction revealed an asymmetrical divergence of the ribs on the right and left sides of the chest (Fig. 4).
Rice. 4.
Sonographic picture of rib asymmetry in 3D reconstruction mode.
The ribs of the left side were brought closer together, the intercostal spaces were reduced compared to the opposite side (Fig. 5, 6). No other pathology was detected in the fetus. Congenital scoliosis is suspected, the basis of which is the presence of lateral hemivertebrae (hemivertebrae) or lateral wedge-shaped vertebrae. At 26 weeks, the ultrasound picture remained unchanged. When performing three-dimensional echography, a clear image of asymmetry of the costal arches and scoliotic deformity of the spine was obtained.
Rice. 5.
Asymmetry of intercostal spaces in 3D reconstruction mode.
Rice. 6.
Asymmetry of intercostal spaces in 3D reconstruction mode.
At 30 weeks, fetal fetal indicators corresponded to the gestational age. Scoliotic deformity of the spine persisted. Additionally, a meningeal hernia was identified, emanating from the thoracic spine, in the area of the deformed vertebrae. The hernia was a stalk-shaped formation with a narrowed pedicle (Fig. 7, 8). Its end part was expanded in the form of a loop and filled with anechoic contents (cerebrospinal fluid), which was clearly differentiated against the background of “turbid” amniotic fluid (Fig. 9). Thus, the diagnosis was clarified: spina bifida - meningocele.
Rice. 7.
Pregnancy 30 weeks. Stalked form of meningocele.
Rice. 8.
Place of exit of the meninges.
Rice. 9.
Pregnancy 30 weeks. The echogenicity of the cerebrospinal fluid is lower than the echogenicity of the amniotic fluid.
Further observation did not reveal significant dynamics of the detected changes.
After birth, the diagnosis of spina bifida - meningocele was confirmed. The child was successfully operated on and does not have any neurological disorders.
In this case, local angular deformation of the spine in the thoracic region and asymmetry of the ribs were the initial ultrasound signs of the open form of spina bifida - meningocele in the second trimester of pregnancy. The manifestation of the hernia occurred only in the third trimester.
Clinical observation 2
Pregnant M., 21 years old. I first came to the clinic at 20 weeks of pregnancy. The study was carried out on a SonoAce-R7 device (Samsung Medison) using the 3D/4D surface volumetric reconstruction mode. A study of the fetal spine in three planes revealed no bone deformities. A thin-walled cystic formation with anechoic content, stalk-shaped, was found in the thoracic spine (Fig. 10-12). The degree of “transparency” of the contents was higher than amniotic fluid, which made it possible to identify it as cerebrospinal fluid. In the projection of the hernial protrusion there was a loop of the umbilical cord, the differential diagnosis of which was easily carried out using color doppler (Fig. 13).
Rice. 10.
Pregnancy 20 weeks. Meningocele: a typical stalk-shaped cystic formation.
Rice. eleven.
Pregnancy 20 weeks. Meningocele.
Rice. 12.
Meningocele. The sagittal section shows unevenness of the skin in the projection of the cleft.
Rice. 13.
Umbilical cord loop in color flow mode.
The fetus had severe hydrocephalus caused by Aronold-Chiari II syndrome (Fig. 14, 15).
Rice. 14.
Pregnancy 20 weeks. Hydrocephalus.
Rice. 15.
Pregnancy 20 weeks. Lengthening of the cerebral peduncles and herniation of the cerebellum into the foramen magnum in Arnold-Chiari II syndrome.
Considering the typical shape of the hernial protrusion and the absence of elements of nervous tissue, it was assumed that the fetus had a meningocele (Fig. 16). The woman decided to terminate the pregnancy.
Rice. 16.
Pregnancy 20 weeks. Meningocele measuring 37x21 mm.
Clinical observation 3
A 27-year-old pregnant woman came to the clinic at 18 weeks. Echography revealed Arnold-Chiari II syndrome and moderate hydrocephalus (Fig. 17).
Rice. 17.
Pregnancy 18 weeks. Hydrocephalus.
Spina bifida cystica was detected in the sacral spine (Fig. 18).
Rice. 18.
Pregnancy 18 weeks. Spina bifida in the sacral region.
The woman decided to terminate her pregnancy.
Clinical observation 4
A 25-year-old pregnant woman came to the clinic at 18 weeks. Echography revealed a gross kyphotic deformity of the spine in the lumbar region (Fig. 19).
Rice. 19.
Spinal deformity.
In the projection of the deformation, myelomeningocele is determined (Fig. 20).
Rice. 20.
Myelomeningocele.
The detection of typical echographic signs allowed us to establish the diagnosis of myelomeningocele.
The woman decided to terminate her pregnancy.
Conclusion
Diagnosis of open forms of spina bifida is not a difficult task in the second trimester of pregnancy. The detection of changes such as Arnold-Chiari II syndrome and a spinal defect with the formation of a hernial protrusion leaves no doubt about the diagnosis. The only exceptions are those cases when the ultrasound manifestation of the defect is represented only by spinal deformation. Currently, the greatest interest is in identifying this defect in the first trimester of pregnancy. Ultrasound criteria such as the absence of intracranial translucency, smoothness of the brainstem angle, a decrease in biparietal size below the 5th percentile, etc. are studied. Thus, the diagnosis of spina bifida remains an important task in prenatal diagnosis.
Literature
- Amari F., Junkers W., Djalali S., Hartge DR et al. Fetal spina bifida — prenatal course and outcome in 103 cases // J. Ultrasound in Obstetrics & Gynecology. 2009. N 34. P. 82.
- Pugash D., Irwin B., Lim K., Thiessen P., Poskitt K., Cochrane D. Prenatal diagnosis of closed spinal dysraphism // J Ultrasound in Obstetrics & Gynecology. 2006. N 28. P. 547.
- Tortori-Donati P., Rossi A., Cama A. Spinal dys-raphism: a review of neuroradiological features with embryological correlations and proposal for a new classification // Neuroradiology. 2000. N 42. P. 471-491.
- Van den Hof MC, Nicolaides KH, Campbell J., Campbell S. Evaluation of the lemon and banana signs in one hundred thirty fetuses with open spina bifida // Am J Obstet Gynecol. 1990. N 162. P. 322-327.
- Ghi T., Pilu G., Falco P., Segata M., Carletti A., Cocchi G., Santini D., Bonasoni P., Tani G., Rizzo N. Prenatal diagnosis of open and closed spina bifida.Ultrasound Obstet Gynecol. 2006. N. 28. P. 899-903.
- D'Addario V., Rossi AC, Pinto V., Pintucci A., Di Cagno L. Comparison of six sonographic signs in the prenatal diagnosis of spina bifida // J Perinat Med. 2008. N 36. P. 330-334.
Ultrasound scanner RS80
A benchmark for new standards!
Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of advanced ultrasound technologies to solve the most challenging diagnostic problems.
How to diagnose a neural tube defect or pathology?
A neural tube defect can only be seen on ultrasound in the third trimester of pregnancy. But before that there is still a lot of chance to detect such a pathology.
To begin with, as already mentioned, it is necessary to perform a preliminary diagnosis, which is recommended during the planning period for a future pregnancy. You should also visit an obstetrician-gynecologist, urologist and geneticist. If possible, it is worth undergoing tests that will show the level of risk of having a child with a neural tube defect. In addition, it is recommended to read a lot of specialized literature. This will help you understand what the fetal neural tube is, and will also allow you to study all the recommendations of specialists that will be useful to you in the future.
After conception, there is no way to do without a monthly examination by an obstetrician. The second trimester of pregnancy must be accompanied by regular blood tests for the expectant mother. It is already possible to conduct an ultrasound examination of the fetus. Don’t be shy about asking a specialist about your baby’s condition, especially if you are in a group of women with an increased risk of neural tube pathology.
In the third trimester, it is already possible to see through ultrasound a congenital deformity of the fetus, which arose as a result of the incorrect formation of the neural tube. A photo of the embryo in the womb can also be shown to another specialist to confirm the diagnosis.
If at one stage a defect in the formation of the neural tube was confirmed, this is a serious reason to raise the issue of termination of pregnancy. However, first you need to find out the degree of the disorder, because with some of its forms a completely normal life is possible. Today, improper formation of the neural tube, which results in the development of deformities in the fetus, can be corrected through surgery. Additional diagnostics are required after you have been given a similar diagnosis, because termination of pregnancy is the very last option.
Diagnostics
Detection of such defects is carried out in the prenatal period. Biochemical techniques and various methods of intrascopy of the fetus are used. All pregnant women are divided into several risk groups for developing neural tube defects in the fetus. What does this mean? Diagnostic measures in each group differ.
- For women at low risk, examinations by obstetricians and gynecologists are carried out once a month. After the 15th week of pregnancy, the content of fetoprotein in the woman’s blood and amniotic fluid is examined. If its level is significantly reduced, a repeat examination and ultrasound of the fetus is performed. In the third trimester, another ultrasound is performed.
- In high-risk groups, examination by an obstetrician-gynecologist is also required - already several times a month. After week 15, fetoprotein levels are repeatedly examined. Sonographic examination of the fetus is also carried out regularly. If there are difficulties in diagnosis, tomographic methods are indicated.
Ultrasound examination can be carried out in the usual way or with a three-dimensional image. This image allows you to examine the fetus from all sides and more accurately identify pathology.
Diagnostics only establishes the presence of a neural tube defect, but does not determine the degree of its severity. Therefore, the issue of maintaining or terminating a pregnancy is decided jointly by the obstetrician-gynecologist and the woman. After the presence of such a developmental defect is established, a conversation is held with the woman. All possible options for the course of pregnancy and the condition of the fetus are explained to her. The child may be born severely disabled.
Treatment of neural tube defects
Treatment of problems that arose due to the fact that the formation of the neural tube was disrupted can begin immediately after the birth of the child. As soon as doctors eliminate all threats to the baby’s life, that is, restore independent breathing and check the newborn’s body temperature, the surface of the hernia should immediately be treated with disinfectant solutions and covered with sterile napkins. After a conversation with the parents, if they agree to surgery, the newborn is transferred to the neurosurgical department, where all the necessary studies are carried out, because without them the operation will not be successful.
If there is a threat of hernia rupture, excision is performed immediately. Otherwise, you can wait a little until the child gets stronger. This decision is justified by the fact that ruptures are “open gates” for any type of infection. Often after removal of hernias, purulent-inflammatory processes are observed. According to statistics, approximately 78% of young patients experienced such complications. It should be noted that within a day after the operation, the children’s health status returns to normal. However, 5% of children still remain at risk.
It is also important that if a similar operation is performed on a newborn, the integrity of the brain membrane can be completely restored. That is, the child after the operation will develop absolutely normally, and an ordinary full life will await him. It is necessary to understand that preliminary studies before surgery are carried out very quickly. They do only the most necessary tests to save the child and not allow him to remain disabled for life. It is important to take the postoperative period seriously. In order for rehabilitation to proceed easily and without complications, all recommendations of the attending physician must be strictly followed.