502
Diabetic neuropathy or diabetic neuropathy is the medical term for nerve damage caused by high blood sugar levels. Most often, diabetic neuropathy of the lower extremities occurs in patients with diabetes mellitus, the treatment of which must be carried out under the proper supervision of the attending endocrinologist.
Diabetic neuropathy is one of the most common chronic complications of diabetes. It is observed both in patients with type 1 diabetes and in patients with type 2 diabetes. When we talk about diabetic neuropathy, we mean peripheral neuropathy.
Diabetic neuropathy is one of the most common complications of diabetes mellitus and affects more than half of patients with this disease. High blood glucose levels over many years (hyperglycemia) contribute to the development of this complication.
Diabetic neuropathy can interfere with the perception of pain.
Neuropathy can lead to many painful symptoms and damage to various organs. Therefore, maintaining proper diabetes control and maintaining HbA1c levels within acceptable limits is extremely important to prevent this disease.
Causes
There are a huge number of reasons for the development of leg neuritis and in order to identify them, it is necessary to undergo research. Inflammation of the nerve endings occurs and this leads to pinched nerves.
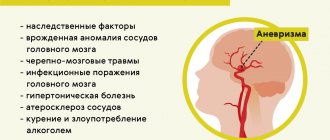
Neuropathy of the lower extremities has the following causes:
- The disease can be inherited.
- The girl suffered from infectious and viral diseases during pregnancy. Poisoning of the body with various chemicals.
- Problems during childbirth may result in infant asphyxia, which leads to the development of neuritis.
- Frequent colds in childhood.
- Brain contusions in a child.
- Various serious pathologies that the patient has suffered from before.
- Drinking alcoholic beverages on a regular basis.
- Side effects of medications such as: antibiotics, antitumor drugs.
- Diabetes mellitus leads to the development of neuropathy, so nerve endings are damaged.
- Infectious diseases such as HIV or diphtheria.
- Various bruises and injuries.
- Neoplasms.
- Hypothermia.
- Lack of vitamins and minerals.
- Pathologies associated with the spine.
Most often, lower extremity neuropathy develops in the upper leg at the thigh. The inflammatory process may begin from the feet and the signs may not be noticeable, since there is no pain. Impairment of blood flow and performance of the limbs does not occur immediately, but over time.
In order to prevent the disease from developing, it is necessary to undergo regular preventive examinations. If you are bothered by even slight pain, you should immediately go to the doctor. If the disease is neglected, complications cannot be avoided.
Symptoms
The inflammatory process in neuropathy of the lower extremities does not occur immediately. At first, pain and circulatory problems do not occur. The disease can affect any area of the legs. It may be in the hip, knee joint, or in the foot, finger, or shin. Signs may appear in the form of numbness, pain, and muscle weakness.
With neuritis of the legs, the following symptoms occur:
- If the pathology affects the lumbosacral region, then a pain syndrome occurs that radiates to the lower extremities and lower back. Muscle weakness in the pelvic area and impaired movement may be a concern. Stiffness and poor sensitivity in the legs are often observed.
- If the sciatic nerve is affected, the pain will be dull and shooting in nature. The pain may radiate to the buttock, lower leg, or thigh. The patient may feel that the skin has become less sensitive. The pain syndrome may intensify when trying to sit down or while lying in bed to raise a limb.
- If the femoral nerve is affected, it may be difficult to bend and straighten the leg. Muscle atrophy and loss of mobility in the knees often occur.
- If the peroneal nerve is affected, it is difficult for the patient to step on the heel. The patient begins to limp and his gait is impaired.
- When the tibial nerve is damaged, it is difficult for the patient to stand on tiptoes and there is no reflex in the Achilles tendon. Most often, stiffness in the movements of the fingers and feet may be observed.
The first manifestations of leg neuritis depend on which nerve node is affected. If damage occurs, most often the patient may experience a loss of sensitivity and a feeling of squeezing.
Therapy is carried out only by a doctor, since it is not recommended to treat the pathology on your own. If you start the disease, irreversible consequences will develop. In order to avoid complications, it is necessary to consult a doctor in a timely manner and not self-diagnose.
Symptoms of neuropathy
The clinical picture of the disease can be very different and affect any place in the body. Depending on the nature of the lesion, neuropathy is divided into:
- sensory – impaired sensitivity of the affected organ. The patient may feel numbness of the limbs, tingling, crawling without causing irritation, burning, pain, unsteadiness of gait;
- peripheral - a violation of the conduction of impulses from the central nervous system to organs that are connected to the affected nerve fibers. Accompanied by tingling and tingling at the site of the damaged nerve, numbness of the limbs, decreased sensitivity to pain and temperature changes. Expressed by burning pain, loss of balance, loss of coordination;
- motor – defective motor activity. With this form, a decrease in sensitivity is not observed. The patient unintentionally makes uncontrolled movements of the limbs, muscle reflexes partially disappear, and muscle weakness gradually begins to appear. Accompanied by pain and, at the initial stage, convulsions;
- autonomous - affects internal organs. It is considered the most dangerous, because As the disease progresses, the functioning of certain organs and systems is disrupted. The function of swallowing, urination, and defecation may be impaired.
The disease manifests itself in different ways, the most characteristic symptoms are:
- impaired sensitivity of the damaged area;
- pain syndrome of varying severity and intensity;
- muscle weakness;
- spasms and cramps;
- difficult movements.
Diagnostics
If neuropathy of the lower extremities is detected in time, this will help to cure neuritis of the legs quickly and without consequences. First of all, a comprehensive examination is carried out and only then treatment is prescribed. The specialist first conducts a general examination and clarifies what symptoms are bothering the patient. Tests knee joint reflexes and refers for diagnostics.
A cerebrospinal fluid analysis may be prescribed; this makes it possible to find out the antibodies that appear in neuropathy. Highly specialized studies are needed to identify various malignant tumors, diseases of the blood, heart and vascular system.
To confirm an accurate diagnosis, a specialist may prescribe a computed tomography scan. This procedure will help the doctor obtain information about the condition of internal organs, muscles and bones. Magnetic resonance imaging is used to determine the size of muscle tissue, as well as what exactly can put pressure on nerve endings.
Electromyography is performed using a needle inserted into a muscle to measure the electrical activity of muscle fibers. This method makes it possible to find out the condition of the nerve nodes and the cause of muscle damage. A nerve biopsy is also performed; nerve tissue is taken from the patient. The procedure is rarely prescribed, as it can further worsen the patient's condition.
If you consult a doctor on time, this will help avoid a number of serious consequences. If the symptoms are ignored, this can lead to problems with extension and flexion of the knee joint. The disease can develop into chronic pain. It often happens that the patient partially loses sensation in the lower leg and foot.
Therefore, at the first slight pain in the lower extremities, you should visit a medical facility. The specialist will conduct a thorough examination and refer you for a comprehensive study.
What is neuralgia?
Muscular neuralgia is a condition in which peripheral nerves are affected. Inflamed tissue in the interosseous spaces begins to compress the nerve, causing the person to feel severe pain. Very often, neuralgia is localized between the ribs on the back or in the lumbar region (neuralgia of the back).
Classification of the disease
Neuralgia (as a general disease) has several types. In modern medicine, it is divided into primary (also called typical, idiopathic and essential) and secondary (also called symptomatic).
In addition to division by origin, there is a classification in terms of localization of muscle spasm.
In this case, neuralgia is divided into :
- trigeminal neuralgia;
- occipital (and facial) neuralgia;
- intercostal neuralgia (one of the most common);
- neuralgia of the external cutaneous nerve of the thigh.
Clinical picture of neuralgia of the back
Pain in the back muscles is the most common in patients. This disease affects people with low immunity. It was once believed that neuralgia was the lot of older people, but in the modern world there is a sharp “rejuvenation” of this disease .
Symptoms almost always appear in acute form , so it is simply impossible not to notice them. The back begins to hurt, and the pain is quite sharp, acute, burning. Symptoms often begin to appear after a person has experienced stress.
Painful sensations occur in paroxysms, as if you were “shocked by an electric shock . Typical pain sensations may become stronger or disappear abruptly, while atypical pain sensations are constant and affect large areas of nerves.
Typically, neuralgia of the back begins with a slight muscle spasm. For example, during heavy physical activity or sudden movements. Also, very often a spasm occurs during awakening from sleep (when sleep took place in an uncomfortable position).
In addition to these reasons, you can also name drafts (the nerve can get cold), sneezing or a strong cough, or a very deep breath.
An attack of neuralgic disease is accompanied by high sweating, muscle tremors and anemia (hyperemia) of the skin.
Prevalence and significance of the disease
Neuralgia in various forms (including neuralgia of the back) is a very common disease . It affects both middle-aged and elderly people, as well as young people, and even children. There can be many reasons for the appearance of severe muscle pain, ranging from a sedentary lifestyle to a decrease in immunity.
Despite the prevalence of the disease, it is difficult to treat in advanced cases, so at the first symptoms it is better to consult a specialist and start treatment. This way you can prevent sudden sharp pain and cope with the problem with a minimum of discomfort.
Video: “How to recognize neuralgia?”
Treatment
- Treatment for lower extremity neuropathy is primarily aimed at controlling symptoms. If the disease was triggered due to diabetes, then for treatment it will be necessary to normalize the blood sugar level. Neuritis of the legs may be due to the use of medications. As a rule, you need to stop taking the medications and the symptoms of the disease will disappear.
- For neuropathy, you need to add foods that contain vitamin B to your diet. It is best to take a course of medications that contain vitamin B12 supplements. Physical therapy can help improve muscle elasticity and joint flexibility. If it is necessary to protect the leg and for its proper functioning, a specialist may prescribe a special splint.
- Orthopedic devices will make it possible to train atrophied muscles in order to avoid disturbances in movement. Treatment should be aimed at learning to relax. Do some physical activity, go for walks more often, do yoga. Massage treatments and acupuncture can help relieve symptoms of neuropathy.
If an exacerbation of the pathology occurs, the patient must be treated in a hospital. You may even need to get your breathing and swallowing back to normal. For this, an oxygen mask and intravenous nutrition are used. Your doctor may also prescribe painkillers to treat leg neuropathy. If the drugs do not bring any results, then antidepressants will most likely be used.
- Physical activity must be present even if the patient cannot walk without the help of crutches. It is best to have special handrails installed in the bathroom or stairs at home, this will help prevent falls. If compression of the nerve ending occurs, surgical intervention is necessary. In this case, only surgery will help eliminate the disease.
- Regular walking gives positive results in treatment. You need to try to go outside more often and do the necessary exercises. It is best for the attending physician to know exactly what kind of physical activity will be done. This will help improve blood supply and nutrition to damaged nerve fibers. Regular walking normalizes blood glucose levels.
- Warm foot baths help relax muscles and relieve pain. To do this, pour hot water into a basin and add sea salt there. The liquid should be no more than forty degrees. Lower your feet into the basin and hold it until you feel the water cooling down.
- You need to completely give up alcoholic beverages, because alcohol is toxic to nerve endings. Typically, neuropathy can develop due to alcoholism.
- To do this, it will be necessary to completely eliminate alcohol, and the patient’s condition will immediately improve. In any case, it is best to limit alcohol, this will help avoid not only neuropathy, but also other diseases.
- Natural evening primrose oil is good for therapy. You can buy it in tablet form, but first of all you need to consult your doctor.
- It has been proven that the medicine contains fatty acids that will improve the patient’s condition. If you follow all the specialist’s recommendations, this will speed up the recovery process. If minor manifestations of leg neuropathy become noticeable, you should immediately consult a doctor.
Also read about neuropathy of the peroneal or radial nerve. As well as the risk of middle nerve neurogia.
Most often, the pathology develops due to diabetes mellitus and various injuries. In order to avoid consequences, it is necessary to visit a medical facility in a timely manner. The doctor will first order you to undergo a comprehensive examination. Then he will make an accurate diagnosis and prescribe treatment. We must not forget that the earlier therapy is started, the fewer complications there will be.
Treatment through the skin
There are about two million sweat glands on the surface of the human body.
Within two minutes after sweating, these glands can absorb any wetting solution. It will enter the tissue fluid, lymph. Up to 10 ml of liquid can be absorbed in this way.
Subscribe to our INSTAGRAM account!
This ability of the human body was established by the Kyiv scientist P.P. Slynko. The scientist called his discovery the phenomenon of postpermeability of the skin. The therapeutic effect of compresses is based precisely on this effect.
For these purposes, semi-alcohol compresses are used from tinctures of calendula, eucalyptus, St. John's wort or thyme .
You can prepare a tincture for a compress at home.
- 15-20 g of dry raw materials are poured with 100 ml of alcohol (or vodka) half diluted with water and left for 10-14 days in a dark place at room temperature.
- Then filter and store in the refrigerator. In the cold, the tincture does not lose its medicinal qualities throughout the year.
Application:
1. Multilayer gauze soaked in tincture is applied to the projections of the main nerve trunks, covered with waxed (waxed) paper or plastic film.
2. Thermal insulation (cotton wool or flannel) is applied on top. Each subsequent layer should be larger in area than the previous one in order to prevent premature drying of the compress.
3. Then the layer cake made from gauze, film and flannel (cotton) soaked in tincture is fixed with a bandage. Without being too zealous - after all, this is a compress, not a tourniquet that prevents blood circulation.
4. Compresses are applied daily, for 20-30 minutes, for 10-12 days.
Attention! In case of significant skin irritation, you should refrain from applying compresses. The same should be done in case of skin damage, dermatitis, pyoderma.
You can also resort to non-alcoholic compresses , but then you need to have on hand fresh juice of black radish (dilute with water before use), burdock root (dilute with water), horseradish or red beets.
All other components of the compress - multilayer gauze, film, heat-insulating layer, fixing bandage - are exactly the same as for alcohol compresses. I also apply them daily for 20-30 minutes for 10-12 days. The contraindications are also identical.