Tetanus is a serious infectious disease. Infection occurs as a result of entry of the tetanus pathogen, Clostridium tetani, through the wound surface. The disease is characterized by acute symptoms as a result of intoxication caused by the tetanus neurotoxin – tetanospasmin.
Clostridium tetani spores grow primarily in soil rich in animal and human feces, particularly in rural areas. In Russia, 20-30 cases of tetanus infection are recorded annually.
Specific prevention of tetanus
The most effective measure to prevent the incidence of tetanus is planned specific immunoprophylaxis among the population. Vaccinations provide protection against the disease for more than 96% of vaccinated citizens. Immunization of children and adults is carried out according to the national vaccination calendar.
SEE: NATIONAL VACCINATION CALENDAR FOR 2021
The course of primary immunization with the DTP vaccine consists of three stages
- 1st vaccination – at 3 months of age
- 2nd vaccination – at 4.5 months
- 3rd vaccination – at 6 months
Subsequent revaccination is performed according to the following scheme:
- single revaccination with DPT vaccine – at 1.5 years
- revaccination with ADS-M toxoid – at 6 years of age
- revaccination with ADS-M toxoid – at 14 years of age
- subsequent revaccinations – every 10 years
All completed vaccinations are recorded in citizens’ vaccination certificates.
Forecast.
In general, the mortality rate for tetanus ranges from 40 to 100%. This fluctuation in numbers is associated with the variable value of this indicator in different forms of tetanus. Thus, with the fulminant form, the mortality rate is 100%, with the acute form – 60–80%, with the chronic form, isolated cases of death are observed.
If the incubation period of the disease is less than a week, then the mortality rate reaches 75%, if this period lasts 2-3 weeks - 35-50%, more than a month - 20%.
Emergency prophylaxis of tetanus
Emergency prevention of tetanus is carried out for all kinds of damage to the skin or mucous membranes. Namely, for various wounds and burns, animal bites, damage to the gastrointestinal tract, out-of-hospital births and abortions. Also for severe abscesses and tissue necrosis.
Means for emergency immunoprophylaxis of tetanus: PSHI - antitetanus human immunoglobulin or PSS - antitetanus serum. Emergency measures to prevent the development of tetanus are carried out individually. The degree of risk of infection from the injury and the patient’s documented previous vaccinations are taken into account.
Nature of injury and risk of tetanus infection
Types of emergency tetanus prophylaxis:
- seroprophylaxis PSCHI or PSS
- combined prevention: simultaneous administration of PSCH (or PSS ) and tetanus toxoid
- in previously vaccinated patients, revaccination with tetanus toxoid AS or ADS-M is possible
EMERGENCY PREVENTION SCHEME FOR TETANUS:
Compliance with the established timing of vaccination is the most effective measure to protect the population from this infectious disease.
SEE ALSO:
EMERGENCY AND SPECIFIC PREVENTION OF TETANUS
SANPIN (SP) 3.1.2.3113-13 Prevention of tetanus
PRESENTATION: TACTICS FOR EMERGENCY PREVENTION OF TETANUS
BOOKLET: PREVENTION OF TETANUS
BOOKLET FOR PARENTS: VACCINATIONS - PROTECTION AGAINST INFECTION
REMINDER: WHAT TO DO BEFORE AND AFTER VACCINATION?
Clinic.
In the tetanus clinic, a latent or incubation period is distinguished, which lasts from 1 to 30 days. A characteristic pattern is that the shorter this period, the higher the likelihood of death.
The period of initial manifestations. During this period, unmotivated irritability, fatigue, and profuse sweating are noted. The patient complains of choking in the throat, difficulty swallowing, and often difficulty opening the mouth. Muscle twitching is detected in the wound area.
High period. In this case, convulsive and neurovegetative syndromes become important clinically.
Convulsive syndrome is manifested by contraction of various muscles or muscle groups. There may be clonic convulsions, during which alternating contraction and relaxation occur. Another form is tonic convulsions, in which the contraction phase of muscle fibers predominates.
Depending on which muscles are involved in the spasms, there are different symptoms of tetanus. With tonic contraction of the masticatory muscles, trismus is observed, making it difficult to open the mouth. With convulsive contraction of the facial muscles, a contemptuous facial expression is noted, called a “sardonic” or “devilish smile.”
The slightest light or sound stimulus causes increased convulsions. They quickly spread to the muscles of the neck, back, and entire body. In this case, the body can take a curved position, which is called opisthotonus.
During convulsions, contractions are so strong that bone fractures and muscle tears are possible.
Neurovegetative syndrome is manifested by increased blood pressure, increased heart rate, electrical instability of the heart in the form of extrasystole up to fibrillation and syncope (cardiac arrest). At the end of the disease, there is an increase in body temperature to critical values. From the gastrointestinal tract there may be erosions and ulcers, erosive bleeding, as well as paralytic intestinal obstruction.
In 60–80% of cases, death occurs from pulmonary complications, which are based on a number of factors. In the prodromal period, under the influence of toxins, ultrastructural damage to the vessels of the pulmonary circulation is observed. Subsequently, under the influence of hyperadrenoreactivity, these disorders are aggravated by the development of extremely severe respiratory failure. Complete depletion of respiratory function due to damage to the respiratory center, as well as possible aspiration of vomit during convulsions, leads to the development of pneumonia. When the respiratory muscles (intercostal and diaphragmatic muscles) are involved in the convulsive process, breathing stops.
Situational tasks
1. A 45-year-old man came to the emergency department with complaints of a wound in the area of the back of his right hand. I got injured a week ago. When examining the hand, a wound of 1.5x1.0 cm is noted, its edges are smooth, moderately infiltrated, hyperemic, palpation is painful, there is practically no discharge from the wound, twitching of the muscles of the back of the hand occurs. What is your diagnosis? Further tactics?
2. A patient consulted an ENT doctor with complaints of choking in her throat and difficulty swallowing. Two days ago, while working at the dacha, I received a puncture wound on my left hand. She had not previously sought medical help for this disease. What disease should be suspected? What's your tactic?
3. A sick tractor driver, 28 years old, was transported from the region to the regional hospital by air with complaints of pain in the right foot, twitching of the foot muscles, back pain, profuse sweating, difficulty opening the mouth, and fever. From the anamnesis it was revealed that 5 days ago he stepped on a sharp metal object, did not seek medical help, washed the wound with water and smeared the edges of the wound with tincture of iodine. After 3 days, twitching in the foot, sweating, and high temperature appeared. 5 days after the injury – difficulty opening the mouth. Objectively: the patient’s condition is serious, the skin is moist, pale, body temperature is 38.9°C, pulse is 108 per minute, blood pressure is 120/80 mm Hg, heart sounds are clear. Local status: on the plantar surface of the right foot in the area of the third metatarsal bone there is a wound of 0.5´0.5 cm, the edges are uneven, swollen, a scant amount of pus is released from the wound, an infiltrate of 3´3 cm around the wound, severe pain on palpation. What is your diagnosis? Why was the patient taken to the regional hospital? In which department should this patient be treated? What treatment is indicated in this case? What complications are possible with this disease?
Routes of entry into the body
Human infection occurs as a result of tetanus entering a wound or cut on the patient’s body. Even very minor scratches and wounds are dangerous. But deep wounds resulting from careless handling of sharp objects are extremely dangerous. Having received damage, it is necessary to immediately treat the wound, since tetanus bacteria are found everywhere: soil, dust, manure. Infection with tetanus is dangerous because it leads to spasm of a person’s muscles, especially the respiratory and chewing muscles.
The bacterium Clostridium tetani is the causative agent of this disease. When it enters the human body through a wound on the body, it forms a toxin, and this already causes the symptoms of tetanus in the patient. There is a risk group; newborns, due to the nature of their work, must constantly receive injections.
Reaction to vaccination
The tetanus vaccine has low reactogenicity, so the vaccine is easily tolerated. In some cases, there may be a short-term change in the child’s normal condition, which goes away on its own. When AFSD vaccinations are administered, a reaction is observed in 30% of cases, since it contains more reactogenic components.
Possible reactions:
- formation of a lump - when the vaccine enters the fatty layer, due to the presence of aluminum hydroxide in it, a reserve is formed at the injection site, which forms a lump and dissolves for a long time (up to 1-2 months);
- redness around the injection site;
- pain at the injection site, which can occur if the vaccine is administered incorrectly (goes away in 2-3 days, you can take anti-inflammatory drugs);
- swelling - disappears after complete resorption of the component;
- temperature - under normal conditions it can last no more than 3 days;
- general reactions – fever, lethargy, drowsiness, irritability.
If the temperature persists for more than 3 days, you should consult a doctor.
Sign up for your vaccination on time!
The disease begins acutely - burning, tingling, pain, cramps of the masticatory muscles; in newborns - difficulty sucking and swallowing. In severe cases, the teeth may be so clenched that it is impossible to open the mouth even with a medical spatula.
The first symptoms are followed in turn by:
- cramps of facial muscles - the forehead gathers into wrinkles, the mouth is stretched, the corners are drooping;
- general convulsive syndrome - the patient arches on the bed in the form of an arch, touching it only with the back of the head and heels (opisthotonus);
- convulsions occur from the slightest irritation and continue continuously;
- high probability of death from spasm of the respiratory muscles (diaphragm, glottis), paralysis of the respiratory heart muscle, myocardial infarction, pneumonia, sepsis, pulmonary embolism.
Treatment of the disease takes 1-3 months in hospital and can seriously affect the patient's future health.
All this indicates the urgent need for timely vaccination. MAKE AN APPOINTMENT PRICES
Mechanism of disease
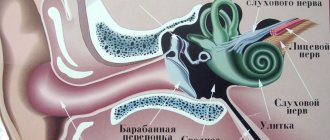
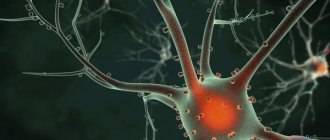
The process of infection with tetanus occurs as follows: through a wound on a person’s body, the causative agent of the disease enters his body. In these wounds, especially if they are significant, vegetative forms multiply; this process occurs simultaneously with the release of toxic substances into the body. Along the nerve fibers, along with the bloodstream, this poison enters the spinal cord and other vital systems of the human body. Moreover, the human body is not able to neutralize this toxin on its own. This causes all the symptoms of this disease.
All these processes cause muscle spasms, convulsions appear, and cardiac activity is significantly weakened. This significantly weakens the immune system, which can lead to secondary bacterial complications. Problems with cardiovascular activity:
- tachycardia;
- ventricular fibrillation;
They intensify due to the fact that with this disease the hyperactivity of the sympathetic nervous system increases. The excitability of the cerebral cortex increases. Damage to the respiratory and vasomotor centers of the vagus nerve is possible, and this leads to a fatal outcome of the disease.
And foreshadowing the question of “is there immunity to tetanus?” it must be said that a person does not develop immunity to this disease. A person who has had tetanus does not acquire immunity from this disease, since an insufficient dose of the toxin enters his body, which can produce antibodies against this disease.
How to behave after vaccination?
After vaccination, it is recommended to follow several basic rules that will help facilitate the period of antibody production in the body;
- if there is a fever, do not bathe the child on the first day, you can wipe it with a damp towel;
- if there is severe local inflammation, do not soap the injection site or rub it with a washcloth;
- do not use cream on the injection site;
- refuse to visit the sauna, swimming pool, or beach with your child for 3 days;
- follow a light diet for 3-4 days.