Muscle weakness and muscle fatigue are among the most common symptoms for which neurological medical attention is sought. There are objective and subjective criteria to determine the presence of a pathological condition. When we talk about weakness, we usually mean a decrease in muscle strength, but patients often complain of general fatigue or difficulty moving in certain areas of the body.
Weakness can be present in individual muscles, affect many groups or the entire body. It occurs suddenly or increases gradually, occurs periodically or persists constantly. In paretic limbs, muscle tone changes, reflexes are quickened or weakened. Depending on the origin and localization of the pathological focus, the clinical picture is supplemented by other symptoms.
Classification
Muscle weakness is caused by a wide range of pathologies. It can be general (widespread) or local. The first implies a state of increased fatigue while maintaining muscle strength. In the second case, a violation of the pathways of nerve impulses from the central nervous system to certain muscles is noted. At the same time, for topical diagnosis it is important to understand the level of damage:
- Central motor neuron:
motor cortex, corticospinal and corticobulbar tracts. - Peripheral motor neuron:
anterior horns of the spinal cord, roots, nerves. - Neuromuscular synapse.
- Muscles.
If central or peripheral motor neurons are involved, paresis is noted with a decrease in muscle strength. In terms of severity, they can be mild, moderate, deep, or take on the character of paralysis (complete lack of movement). Traditionally, paresis is systematized taking into account the location of the lesion and clinical features. In neurology, the following classification is generally accepted:
- Central (spastic).
By eliminating the inhibitory effect of the cortex on the spinal cord, muscle tone and reflexes increase, pathological signs and synkinesis occur. - Peripheral (sluggish).
Damage to the peripheral motor neuron leads to rupture of the reflex arc, which is accompanied by hypotonia and hyporeflexia; upon examination, muscle atrophy and fascicular twitching are noticeable. - Mixed.
A combination of spastic paresis below the level of the lesion due to interruption of the corticospinal tract and peripheral, caused by a pathological process in the region of the anterior cords of the spinal cord.
Separately, psychogenic paresis is distinguished, which occurs without organic causes with complete preservation of the conductive tracts of the brain and spinal cord. Their development is associated with dysfunction of higher nervous activity. The involvement of individual limbs in the process is essential for diagnosis; therefore, in the clinic of nervous diseases, several types of paresis are distinguished:
- Monoparesis.
Weakness is observed in one limb. - Biparesis.
It is divided into hemiparesis, in which the arm and leg are affected on one side, and paraparesis, which involves symmetrical limbs - upper or lower. - Triparesis.
Muscle strength is reduced in three limbs (a combination of hemi- and paraparesis). - Tetraparesis.
Movement disorders affect both arms and legs.
Based on their prevalence, weakness of certain muscles (for example, fingers or facial muscles), entire groups (flexors, extensors) or sections (distal, proximal) are distinguished. It should be understood that the term “paresis” is used not only to describe the work of skeletal muscles, but is also applied to some internal organs (intestines, bladder).
Paresis of the limbs as a symptom of the disease
Paresis of the limbs occurs due to dysfunction of the brain or spinal cord. Those parts of it that are responsible for motor activity. At the same time, the muscles of the arms and legs cease to obey, which does not allow the person to move freely. Very often this condition provokes a stroke.
In the International Classification of Diseases (ICD-10), sometimes such pathology is classified as code R 29.8 - other and unspecified symptoms and signs.
When the leg and foot are paralyzed, it is very difficult to bend the hip, and sensitivity disappears. If paresis of the arms occurs, a decrease in movements becomes noticeable. A person cannot even make a normal handshake.
With prolonged paralysis, the muscles begin to atrophy, and it will become increasingly difficult to restore their functions. This will require special treatment, massage and exercise therapy.
Muscle atrophy with limb paresis
Why does muscle weakness occur?
Causes of weakness in the limbs
When considering the origin of skeletal muscle weakness, it is worth separating the concept of paresis associated with damage to nerve pathways and symptoms caused by defects in synaptic transmission and muscle damage. Often we are talking about blockade or increased destruction of acetylcholine, primary or secondary muscle pathology, reflex syndromes. Among the most well-known causes of weakness are the following:
- Myasthenia.
- Myasthenic syndromes:
Lambert-Eaton associated with slow closure of ion channels, familial infantile myasthenia. - Hereditary paroxysmal myoplegia:
hyper-, hypo- and normokalemic, Andersen-Tawil syndrome. - Infections:
botulism, tick-borne encephalitis. - Endocrine pathology:
hyper- and hypothyroidism, Conn's syndrome, Addison's disease. - Myopathies:
inflammatory (acute myositis, polymyositis, dermatomyositis), metabolic (including storage diseases), mitochondrial. - Muscular dystrophies:
progressive (Duchenne, Becker, Emery-Dreyfus), non-progressive (myotubular myopathy). - Diseases of the musculoskeletal system:
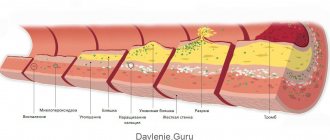
arthrosis, tendonitis, injuries. - Vascular pathology:
obliterating endarteritis, varicose veins of the lower extremities, Takayasu's disease. - Poisoning:
organophosphorus compounds, carbon monoxide, cyanides, aromatic hydrocarbons (toluene, benzene), plants (hemlock), nicotine, cocaine. - Taking medications:
D-penicillamine, antibiotics, antitumor drugs, statins, cortisone, colchicine, chloroquine.
Weakness in the muscles of the whole body is provoked by various systemic diseases and intoxications. It is noted in acute and chronic infections, autoimmune pathology, and malignant tumors. Low motor activity in older people, with immobilization, prolonged bed rest are common causes of widespread limb weakness.
Causes of facial muscle weakness
The facial muscles are innervated by the facial nerve (VII pair). Any pathology that disrupts the conduction of impulses along motor fibers - from the corticonuclear pathway to the peripheral part - can cause muscle weakness. It is also worth considering the direct damage to the muscles themselves. The list of probable pathologies includes the following conditions:
- Neuritis of the facial nerve (Bell's palsy).
- Facioscapulohumeral myodystrophy of Landouzy-Dejerine.
- Degenerative diseases:
progressive bulbar palsy, syringobulbia. - Tumors:
base of the skull (Garcin's syndrome), cerebellopontine angle, temporal bone and middle ear. - Hemorrhages and infarctions of the pons area.
- Congenital anomalies:
Chiari malformation, Klippel-Feil syndrome. - Infections:
herpetic ganglionitis of the geniculate ganglion (Ramsay-Hunt syndrome), polioencephalitis, Lyme disease, syphilis. - Meningitis:
bacterial, tuberculous, fungal. - Systemic pathology:
sarcoidosis, periarteritis nodosa, Behcet's disease. - Consequence of injuries, facial surgery, installation of a cochlear implant.
- The effect of chemotherapy drugs.
The facial nerve is often damaged by inflammatory processes in the ear and parotid salivary glands. Compression or rupture of its fibers is observed in TBI with a fracture of the base of the skull. The risk of facial nerve paresis increases in older people, with a long history of smoking, and the presence of concomitant pathologies (diabetes mellitus, arterial hypertension).
Causes of paresis
The upper or first neuron of the motor pathway begins in the motor cortex of the precentral gyrus, goes as part of the pyramidal tract through the internal capsule and trunk, ending in the anterior horns of the spinal cord. There, the impulse is transmitted to the second motor neuron, the axons of which make up the roots and peripheral nerves. Damage to these structures at any length is accompanied by paresis, which is typical for various pathologies of the nervous system:
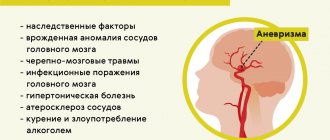
- Strokes:
hemorrhagic, ischemic, subarachnoid hemorrhage. - Tumors and traumatic brain injuries.
- Demyelinating diseases:
leukodystrophies, multiple sclerosis, Devic's opticomyelitis. - Motor neuron diseases:
amyotrophic lateral sclerosis, spinocerebellar and bulbospinal atrophy. - Cerebral palsy.
- Neurodegenerative processes:
Wilson-Konovalov's disease, Shtrumpel's disease, Refsum's disease. - Myelopathy:
compression, spinal cord ischemia, transverse myelitis. - Damage to peripheral nerves:
polyneuropathies (metabolic, toxic, hereditary), tunnel syndromes, plexopathies. - Acute polyradiculoneuritis:
diphtheria, Guillain-Barré syndrome, ascending Landry's palsy. - Infections:
polio, meningococcal meningoencephalitis, rabies. - Vertebrogenic pathology:
intervertebral hernia, osteochondrosis, scoliosis. - Intoxication:
nerve poisons, salts of heavy metals (thallium, lead, arsenic).
Disturbances in spinal conduction are often caused by spinal cord injuries, which entail compression, ischemic damage, and swelling of the nervous tissue. There are also direct wounds - gunshots, bone fragments from fractures. Typically, the cervical spine is susceptible to such damage; the thoracic and lumbar spine are affected much less frequently. In case of concussion of brain tissue, the changes are transient in nature, in other cases they are more persistent.
Metastatic tumors (lung, breast or prostate cancer) are a common cause of compression of the spinal cord; lymphoma, multiple myeloma, and epidural hematomas are less common. If weakness appears in the arms or legs, tuberculous spondylitis, rheumatoid arthritis with subluxation of the atlantoaxial joint, and spinal vascular malformations are excluded.
Prevention
Limb paresis can be prevented. To do this, you need to do physical exercise all your life and want to exercise. This will promote overall health. But it is necessary to understand that complex diseases can cause paralysis of the arms and legs.
Therefore, after receiving injuries or illnesses, you need to devote more time to preventive measures:
- To refuse from bad habits.
- Monitor your blood pressure.
- Consult a doctor promptly if there are any changes in the functioning of the musculoskeletal system.
- Monitor the functioning of the cardiovascular system. This is especially true for older people.
- Have regular medical examinations.
It is impossible to completely insure yourself against paralysis, but there is a real opportunity to minimize such chances.
Diagnostics
When conducting a clinical examination, true muscle weakness with a decrease in strength is distinguished from increased fatigue as a subjective sign. The anamnesis is used to find out information about the intensity and rate of development of the symptom, and the presence of additional signs. During a neurological examination, the doctor determines muscle strength (in points), range of active and passive movements, and reflexes. To determine the cause of muscle weakness, additional studies are prescribed:
- Blood analysis.
If an infection is suspected, a hemogram gives an idea of the leukocyte formula and ESR. Biochemical analysis allows us to identify electrolyte and hormonal disorders, the presence of antibodies to the pathogen. Toxicological examination shows the content of toxic substances in the blood. - Lumbar puncture.
Cerebrospinal fluid is taken for examination to exclude subarachnoid hemorrhages, infectious and inflammatory diseases of the brain and membranes. CSF pressure is assessed in case of volumetric processes (tumors, abscesses, hematomas). - X-ray.
X-ray of the spine is the first test prescribed for spinal injuries. Standard photographs do not show fractures of the odontoid process or the lower cervical segment, which requires special radiographs and the use of other imaging techniques. - Tomography.
In case of damage to the central nervous system, MRI is considered the main method of neuroimaging. The method is highly informative for pathology of the posterior cranial fossa, inflammation of the meninges, and myelopathy. CT scan of the brain is more suitable for patients with basal skull fractures in the acute period of stroke. - Myelography.
This is an X-ray examination of the central canal of the spinal cord. The procedure is performed for herniated intervertebral discs, spinal injuries, and tumors. The technique shows any obstacles to normal liquor dynamics. - Electroneuromyography.
Damage to nerve trunks and fibers requires a functional study with analysis of impulse conduction to the muscles, which allows one to evaluate the speed of signal transmission, the location of damage, and the ability of muscles to contract.
If muscle weakness is accompanied by systemic disorders, the examination plan includes ultrasound of the kidneys and adrenal glands, thyroid and parathyroid glands. For vascular disorders, ultrasound and angiography are performed. The search for a malignant tumor may require radioisotope scintigraphy. Given the variety of causes, a neurologist has to carry out a thorough differential diagnosis with the involvement of related specialists.
Physiotherapy is used in the complex treatment of paresis.
Etiology
Depending on the etiology, there are organic and functional paralysis[1]. Organic ones occur when the nervous system is damaged at different levels by a tumor, injury, infection or some other factor [1]. Functional paralysis is a consequence of a stagnant area of inhibition in the brain, for example, in dissociative (conversion) disorders according to ICD-10 (namely dissociative movement disorders - 44.444.4), previously encountered in so-called hysteria [1] [2]. Functional paralysis can be complete or partial[2], occurs in a traumatic situation and is distinguished by its demonstrative nature. When there are no spectators, they can disappear completely.
Treatment of paresis
Help before diagnosis
Abruptly occurring severe local or general muscle weakness is a reason to seek medical help. In acute conditions associated with a direct threat to life, urgent measures are necessary. Suspected traumatic brain or spinal injuries require immobilization of the cervical spine with a head restraint or collar, and patients with probable spinal injuries are transported on a rigid stretcher.
In case of serious injuries with paresis of the respiratory muscles, hemorrhagic stroke, resuscitation measures are necessary - mechanical ventilation with intubation, chest compressions. At the prehospital stage, blood pressure is stabilized, cerebral edema is combated, vomiting and convulsions are stopped. Undifferentiated treatment of stroke involves the use of neuroprotectors.
Conservative therapy
A decrease in muscle strength requires a comprehensive solution aimed at eliminating the cause of motor dysfunction and restoring lost abilities. The basis of the conservative strategy is drug therapy, selected in accordance with clinical feasibility. Considering the causes and mechanisms of development of weakness, the following drugs may be prescribed:
- Neuroprotectors.
Used for strokes (ischemic, hemorrhagic), consequences of TBI, myelopathies. The main directions of neuroprotection are represented by antioxidant protection, inhibition of local inflammation (cytokine antagonists), improvement of trophism (nootropics, choline, carnitine preparations), blood circulation (nimodipine, vinpocetine). - Immunosuppressants.
Treatment of myasthenia gravis is carried out with immunosuppressants (azathioprine, cyclosporine), immunoglobulins. Interferons, monoclonal antibodies, and glucocorticoids are used to suppress autoimmune reactions in patients with multiple sclerosis. The latter are also used as replacement therapy for Addison's disease, cerebral edema, and radicular syndrome. - Antimicrobial.
Treatment of neuroinfections of bacterial origin requires the use of antibiotics. For tick-borne encephalitis, specific immunoglobulins are indicated; botulism is treated with the administration of antitoxic serum. In addition to etiotropic therapy for acute infections, detoxification agents are prescribed.
Correction of metabolic disorders is required for endocrine pathology, some myopathies, and polyneuropathies. B vitamins, NSAIDs, and cholinesterase inhibitors are actively used. The treatment regimen for vascular pathology includes vasoactive agents (pentoxifylline), venotonics, and antiplatelet agents. Poisoning is treated with active detoxification, including the use of extracorporeal methods.
At the rehabilitation stage, non-drug correction plays a special role. Massage and exercise therapy help restore muscle strength and range of motion. Therapeutic and activating regimens depend on the patient’s condition and the period that has passed since cerebral damage. In the complex treatment of paresis, kinesiotherapy, physiotherapy, and orthopedic correction are used.
Surgery
Surgery is often required to eliminate structural defects that cause paresis. For ischemic stroke, reperfusion techniques are recommended: selective thrombolysis, bypass surgery, endarterectomy. Hemorrhages are removed using puncture-aspiration, stereotactic, and microsurgical methods. In case of compression of the spinal roots, some neuropathies, and tunnel syndromes, decompression operations are necessary.
If conservative therapy for myasthenia gravis is ineffective, it is recommended to remove the thymus gland (thymectomy), which reduces autoimmune aggression. For post-traumatic and postoperative paresis of the facial nerve, reconstructive interventions (suturing, autoplasty) and plastic surgeries (lifting, muscle relocation) are performed to improve the aesthetic result.