Neuropathy of the extremities in diabetes is the general name for a group of pathological conditions characterized by damage to the nerve fibers of the arms or legs. Most often, neuropathy is associated with a pinched nerve due to injury.
The result of such damage can be accompanied by symptoms of varying severity: from mild pain, tingling in the fingers to loss of sensitivity, atrophy of the innervated muscles, and loss of limb functionality. What is it, who treats it and how to treat it?
Statistical data
According to WHO, neuritis affects from 2 to 8% of the world's population. In old age, the disease is more common because it is accompanied by general neurological disorders, weakness of the musculoskeletal system, and slow tissue regeneration processes.
Single nerve lesions are called mononeuropathy . In accordance with ICD-10, the disease was assigned codes G56 - mononeuropathy of the upper extremities and, accordingly, G57 - mononeuropathy of the lower extremities.
Another type of disease is polyneuropathy . As the etymology of the name suggests (“many + nerves + disease”), this is multiple damage to the peripheral nerves.
Polyneuropathy is characterized by a relatively severe course, which is primarily due to the difficulty of rehabilitation during the convalescence period: due to the fact that different nerves activate different muscle groups, the limb is partially or completely immobilized, so recovery must begin with long-term passive exercise therapy. According to the disease classifier, polyneuropathy belongs to classes G60-G64.
Causes
Important ! 70% of neuropathies are associated with injuries to nerve fibers resulting from blows (bruises of the knee and elbow in the immediate vicinity of the tibial and ulnar nerves are especially dangerous), dislocations, bone fractures (often nerve lines run along bone tissue), rupture of ligaments and tendons.
Other common reasons:
- Compression . Caused by vertebrogenic factors: compression due to osteochondrosis, intervertebral hernia, scoliosis, arthritis; also occurring when there is excess pressure on the nerve after applying a cast, when wearing tight shoes, kneeling for a long time, sleeping or sitting in a crooked position, etc.
- Iatrogenic . Provoked by medical errors: pinched nerve when repositioning bones, anesthetizing a limb in the wrong position, hitting a nerve when placing an intramuscular injection.
Developing due to diseases:
- Diabetes . Metabolism is disrupted and the myelin sheath of nerves is destroyed due to lack of nutrition. In this case, the legs usually suffer.
- Vitamin deficiency . Deficiency of vitamins B1, B3, B4, B8 leads to loss of nerve conduction and destruction of nerve fiber. Often causes polyneuropathy.
- Guillain-Barre syndrome (GBS). An autoimmune disease accompanied by aflexia, limb paresis and autonomic disorders. Most often occurs after enteritis, vaccination or immunodeficiency.
- Oncological tumors that grow and block nerve transmission. Typically, this phenomenon occurs in oncology of internal organs with pinching of the spinal stem nerves.
- HIV, drug addiction, diphtheria , herpes and other infectious diseases that have a devastating effect on the central and peripheral nervous system.
- Genetic diseases : varieties of Charcot-Marie-Tooth disease, Dejerine-Sotta disease, other congenital diseases.
- Toxicosis . Associated with carbon monoxide poisoning, poisons, and chemicals. In a mild form it occurs in alcoholism.
Pregnancy . At 6-8 and 20-28 weeks of gestation, a woman experiences a significant decrease in immunity. It occurs as planned and is necessary to prevent an autoimmune reaction to the fetus, which is perceived by the defense system as a foreign organism. If the immune system malfunctions and there is no systemic control, excessively secreted antibodies can cause harm to both the developing child and the nervous system of the mother’s body.
A fairly rare cause of neuropathy is internal bleeding.
Types of pathology and symptoms
The main types of neuropathy:
- Sensory.
- Motor.
- Autonomous.
Sensory
Manifests itself in the form of sensory disturbances: pain, burning, tingling, numbness of the limbs.
Motor
Associated with impaired muscle excitability and subsequent atrophy of the limb up to complete dysfunction. In this case, sensory pathologies do not occur (in rare cases, there is a lack of sensitivity to vibration).
Attention ! Motor neuropathy is accompanied by gradually developing muscle weakness and decreased muscle mass. A feature of motor neuropathy is symmetrical damage to the limbs.
The etiology of this type of neuropathy is usually associated with hereditary diseases and genetic mutations. There are 6 types of motor neuropathy:
- Congenital . Caused by defects in the TRPV4 gene. Primary manifestations are observed from birth, and the disease progresses later.
- Type 2A . Associated with defects in the HSPB8 gene. It is one of the types of peroneal amyotrophy. Affects older children. This type is characterized by a consistent increase in hand damage: muscle weakening (even to atrophy), tactile insensibility.
- Type 2D . It occurs due to structural disturbances of the FBXO38 gene, located on chromosome No. 5. It debuts in adolescence with weakness of the legs, cramps of the lower extremities, and later spreads to the muscles of the arms.
- Distal (symmetrical) neuropathy type 5. The most common type associated with defects in the BSCL2 gene (chromosome No. 11). It manifests itself in adolescence and adulthood in the form of weakness, trembling of the hands. At a late stage it covers the lower extremities.
- Spinal neuropathy type 1 . Occurs due to a failure in the formation of the IGHMBP2 gene. It manifests itself even in the prenatal period in the form of degeneration of the arm muscles. Subsequently, it can affect the smooth muscles of the respiratory system and even cause death.
- Type AX . Caused by a gene mutation on the X chromosome. It affects exclusively males in early childhood, causing motor damage to all extremities.
Motor neuropathy is extremely rare (0.004% of cases). The only existing treatment is supportive medications and a vitamin complex. Exercise therapy is contraindicated, because accelerates tissue degeneration.
Autonomous
More than 90% of patients with diabetes suffer from diabetic neuropathy (DN), which affects the autonomic and peripheral nervous system due to metabolic disorders.
DN occurs in two forms:
- Focal – affects individual areas of the body.
- Diffuse - causes progressive disruption of the functioning of various nerve fibers.
One of the forms of diffuse neuropathy is autonomic, in which dysfunction of internal organs develops with corresponding symptoms:
- Gastrointestinal tract : dyspepsia, stool disorders, increased gas formation, epigastric pain, deterioration of peristalsis, nocturnal diarrhea (with the involvement of nerve fibers responsible for intestinal function).
The gastrointestinal tract is particularly sensitive to neuropathy due to the high vulnerability of the enteric nervous system , the number of nerve cells of which is comparable to their number in the brain.
- Genitourinary system : involuntary urination due to weakening of the bladder, secondary bacterial infections.
- Genital organs : in men – lack of erection while sexual desires persist; in women - a reduction in vaginal secretion during intercourse.
- Cardiovascular system : tachycardia, heart rhythm failure, angina pectoris.
- Skin : dry hands and feet, increased or decreased sweating.
General disorders are also noted: vertigo, loss of consciousness, asthenia.
Features of lower extremity neuropathy
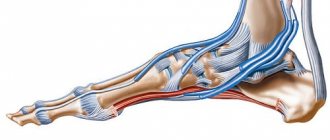
For reference . With neuritis of the legs, mainly 3 nerve canals are affected.
Sciatic nerve
The longest and largest (1 cm in diameter) nerve trunk of the body, which begins in the 4th vertebra and, passing through the opening in the pelvic bone, descends to the popliteal fossa, where it divides into the fibular and magnofibular branches. Compression can occur in the pelvis, in the area of the piriformis muscle, or on the thigh.
Sciatic neuritis is the second most common among neuropathies of the lower extremities (incidence is 0.025%, mainly in people from 40 to 50 years old). Another feature of this disease is that it is not symmetrical - only one limb is affected.
The sciatic nerve activates the muscles that flex the knee joint , so the disease is characterized by the following symptoms:
- Intense immobilizing pain on the back of the thigh , radiating to the lower leg and foot.
- Walking with a straight leg, which occurs due to difficulties in bending the knee (paresis of the biceps and semitendinosus muscles simultaneously with increased tone of the quadriceps muscle).
- Thickening of the stratum corneum of the skin on the heel , blue discoloration of the foot, impaired sweating.
- Deterioration of vibration sensitivity.
Femoral nerve
Originating from the roots of vertebrae 2-4, this nerve trunk passes under the inguinal ligament to the front surface of the thigh, then along the lower leg, foot, and ends in the big toe.
The main functions of the femoral nerve: innervation of the muscles responsible for hip flexion, lower back, knee extension.
The disease may cause both sensory and motor disturbances:
- Weakening of the knee extensor, resulting in the inability to walk up stairs or run.
- Impaired sensory perception, tactile sensitivity, as well as paresthesia along the nerve.
With neuritis of the femoral nerve, the knee reflex is preserved.
Peroneal nerve
The superficial branch of the peroneal nerve is extremely sensitive to mechanical stress. The most characteristic symptoms of the lesion: “horse gait”, weakened supination, foot drop.
Features of neuropathy of the upper extremities
Nervous pathologies of the hands cover 3 nerve trunks.
Radial nerve
Manifestations of the disease : drooping weak hand, poorly bending elbow, numbness and paresthesia in the fingers.
Elbow
Important ! A disease of traumatic origin. Its characteristic symptoms: atrophy of the hand muscles, pain in the elbow joint, weakened fingers.
Podkryltsovy
The axillary (axillary) nerve is a branch of the trunk of the brachial plexus. It passes under the shoulder joint and lies on the lateral side of the humerus before dividing into two branches: anterior and posterior. Its main function is the innervation of the teres minor and deltoid muscles.
Damage to the axillary nerve is almost always caused by severe trauma: a shoulder fracture or deep wound . Athletes involved in traumatic sports (wrestlers, climbers, etc.) regularly encounter this disease. Much less often the influence is exerted by everyday factors: compression by a crutch, pinching during sleep, etc.
Symptoms of injury can vary greatly depending on the severity of the injury:
- Mild or significant limitation of shoulder mobility due to paresis of the deltoid muscle. In severe cases, limb paralysis occurs.
- Loss of sensory sensation on the back and lateral part of the arm.
- Shoulder laxity.
- Deltoid dysfunction.
The treatment prognosis is favorable. If conservative therapy and exercise therapy do not produce results, resection of scar adhesions is used, and sometimes nerve fiber replacement is used.
Forms of neuropathy depending on the prevalence of symptoms
The classification of polyneuropathy according to ICD 10 is officially recognized, but it does not take into account the individual characteristics of the course of the disease and does not determine treatment tactics. Depending on the predominance of clinical manifestations of diseases, the following forms of polyneuropathies are distinguished:
- sensory – signs of involvement of sensory nerves in the process (numbness, burning, pain) predominate;
- motor – signs of damage to motor fibers prevail (muscle weakness, decrease in muscle volume);
- sensorimotor – symptoms of damage to motor and sensory fibers are simultaneously present;
- autonomic – there are signs of involvement of the autonomic nerves in the process: dry skin, rapid heartbeat, tendency to constipation;
- mixed - neurologists determine signs of damage to all types of nerves.
Foot lesion
Foot pathology with neuritis is never primary. It is associated with pinching of the tibial nerve, which innervates the muscles of the lower leg, flexors and extensors of the foot.
When the patellar section of the common tibial nerve is damaged, the most severe consequences for the foot occur : weakening and sagging, up to complete immobilization.
The gait of a patient with such a lesion is characteristic: he raises his leg high, resting first on the toe, then on the entire foot (“horse gait”). The patient cannot stand on his toes. Progression of the disease can lead to disability and loss of ability to work.
The pathology of the foot is less pronounced when the deep branch of the peroneal nerve is damaged . In this case, moderate weakening of the ankle occurs in combination with sensory disorders of the fingers.
In case of injury to the lateral subcutaneous portion of the peroneal nerve, the main symptoms are limited rotational movement of the foot, burning, aching night pain, and impaired vibration perception.
One of the complications of diabetes is the so-called diabetic foot . This is a syndrome in which the skin on the legs becomes covered with poorly healing purulent ulcers with associated secondary infections. In severe cases, the disease progresses to gangrene and leads to amputation of the leg.
For somatic diseases
Diabetic polyneuropathy (ICD10 code G63.2.) is one of the most common and studied forms of somatic polyneuropathies. One of the manifestations of the disease is autonomic dysfunction, which has the following symptoms:
- orthostatic arterial hypotension (decrease in blood pressure when changing body position from horizontal to vertical);
- physiological fluctuations in heart rate;
- disorders of gastric and intestinal motility;
- bladder dysfunction;
- changes in sodium transport in the kidneys, diabetic edema, arrhythmias;
- erectile disfunction;
- skin changes, impaired sweating.
With alcoholic polyneuropathy, paresthesia in the distal limbs and pain in the calf muscles are noted. One of the early characteristic symptoms of the disease is pain, which intensifies with pressure on the nerve trunks and compression of the muscles. Later, weakness and paralysis of all extremities develop, which are more pronounced in the legs, with predominant damage to the extensors of the foot. Atrophy of paretic muscles develops rapidly, periosteal and tendon reflexes are strengthened.
In the later stages of development of the pathological process, muscle tone and muscle-joint sensation decrease, and the following symptoms develop:
- surface sensitivity disorder of the “gloves and socks” type;
- ataxia (instability) in combination with vasomotor, trophic, secretory disorders;
- hyperhidrosis (increased skin moisture);
- swelling and pallor of the distal extremities, decreased local temperature.
Neuropathy of the hands
Like foot pathology, hand diseases are secondary and are caused by a number of neuropathic syndromes:
- Radial neuritis . Leads to motor impairment of the hand—when the arm is raised, it sags. The disease is also accompanied by sensory symptoms such as loss of sensitivity in the fingers.
- Ulnar nerve neuritis . It is characterized by paresis of the flexors and extensors of the fingers, deterioration of fine motor skills of the hands.
- Median nerve neuritis . Consequences: numbness to complete loss of sensitivity in the hands, pain in the fingers, muscle atrophy.
Attention ! Also, hand dysfunction may be associated with certain types of polyneuropathy.
Post-traumatic neuropathy
The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
Pathology such as neuropathy occurs quite often. It manifests itself as severe nerve damage. In post-traumatic neuropathy, damage occurs due to cuts, bruises and fractures. Despite the fact that the nerve itself was not damaged as a result of direct impact, scar processes occur in the area of wound healing, which compress the nerves. As a rule, most often this pathology is characterized by the elbow, median and radial nerves.
In the canal itself, the nerve can be compressed directly by the thickened wall of the canal, which often occurs against the background of arthrosis of the bone wall of the canal, deforming arthrosis of the muscles, or after a fracture. This disorder is characterized by symptoms such as muscle atrophy, numbness, or decreased sensation. Many patients sometimes complain of very unpleasant sensations in their fingers, which usually worsen at night. The grip strength of the hand also decreases, paresthesia and hyperesthesia change, and noticeable swelling of the hand is noted.
First of all, to make a diagnosis, a visual examination will be required to identify areas of increased or decreased sensitivity. It is also necessary to determine the presence of Tinel syndrome and impairments in existing discriminative sensitivity, which is the ability to distinguish and perceive the same stimuli when applied to the skin.
Along with this, during the examination it is necessary to identify muscle atrophy or increased numbness during flexion. It should be noted that more often such motor disorders appear somewhat later in the case of sensory disorders. Subsequently, the first examination and collection of the necessary medical history are followed by the necessary instrumental examination. Electroneuromyography, which determines the exact passage of an impulse along a nerve, is considered the most effective method in modern diagnostics.
In addition, in most cases, ultrasonography and ultrasound examination are performed for clear visualization. The optimal diagnostic method is magnetic resonance imaging, which helps to get a complete picture of the size, type and location of the specific localization of the disorder. Then, based on the data obtained, the specialist, if necessary, selects the type of surgical treatment for post-traumatic neuropathy.
How to get rid of post-traumatic neuropathy?
It has been proven that successful treatment of this disorder directly depends on the duration and type of damage. It is advisable to treat significant damage to a specific nerve trunk on any forearm (radial, ulnar and median nerves) as soon as possible through modern restoration of anatomical integrity. In this case, it is indicated first of all to perform neurolysis, which is a simple surgical operation aimed only at freeing a certain nerve from strong compression by scar tissue.
It should be noted that it is necessary to contact specialists for post-traumatic neuropathy as early as possible so that the entire treatment process goes smoothly and a minimum of complications arise. When more than two months have passed since the onset of development of the existing lesion, the specific surgical intervention is more extensive.
The likelihood of developing dangerous neurogenic contracture of the hand depends directly on the period of time elapsed after the injury. Irreversible changes occur, due to which the nerve practically ceases to properly innervate certain muscles. In this case, all kinds of orthopedic operations are prescribed, during which the necessary transposition of tendons and muscles is carried out. Rapid restoration of lost innervation of the necessary muscles is also a fairly popular method of surgical intervention.
Additional treatment during a certain postoperative period includes immobilization of the operated limb in the correct physiological position. In addition, it is sometimes advisable to fixate in a forced position, when the tension on the nerve is minimal.
Regardless of the cause of the lesion, in the process of treating post-traumatic neuropathy, the necessary drug therapy is also used. In addition, a suitable complex of vitamin preparations is prescribed. Treatment is always accompanied by immobilization of the specific operated limb. This period is up to three weeks so that the scars in the operated area appear minimally. Along with this, immobilization is also important to reduce the risk of possible suture ruptures in the further postoperative period.
Adequate physical therapy is also necessary. Its purpose is to ensure mandatory prevention of the dangerous development of contractures in a given operated limb. Physiotherapy is also indicated, which is mainly aimed at quickly reducing the formation of existing scar tissue.
Author of the article:
Mochalov Pavel Alexandrovich |
Doctor of Medical Sciences therapist Education: Moscow Medical Institute named after. I. M. Sechenov, specialty - “General Medicine” in 1991, in 1993 “Occupational diseases”, in 1996 “Therapy”. Our authors
Treatment methods
In some cases, treatment comes down to eliminating mechanical pinching of the nerve: removing plaster, replacing unsuitable crutches, narrow shoes. Conservative treatment (medicines and special exercises) is more often used . If these measures are not effective, then they resort to the help of a neurosurgeon.
Conservative
A neurologist may prescribe drug therapy to a patient, including:
- Analgesics . A wide range of nonsteroidal anti-inflammatory drugs (NSAIDs): Diclofenac, Ibuprofen, Meloxicam, etc. NSAIDs not only block pain, which is very important for the prevention of muscle atrophy, but relieve swelling and inflammation of the nerve fiber, accelerating recovery. It is important to be careful and strictly limit the dosage and duration of treatment due to the serious side effects of these drugs.
- Vasodolating drugs such as Trental, Cavinton, etc. They have a vasodilating effect, thin the blood, improve blood circulation, and accelerate the regeneration of damaged tissues.
- Nerve stimulants : Neuromidin, Proserin, Ipidacrine. Accelerate the conduction of nerve impulses, tone the smooth muscles of the skeleton.
- Antioxidants . Thiogamma, Berlition and other drugs that improve muscle conduction.
Antioxidants are similar in type of action to B vitamins, but do not replace them.
Vitamins
Vital elements that nourish the nervous system are B vitamins: thiamine, nicotinic acid, cyanocobalamin, choline, inositol, etc.
These substances stimulate the secretion of hormones and hemoglobin, provide energy supply to tissues, and have an analgesic effect..
Therefore, drugs such as Milgama, Neurorubin, Multivit, Vitrum are indispensable during the period of active treatment or at the rehabilitation stage.
Physiotherapy
Physiotherapeutic procedures combine well with drug therapy and significantly speed up recovery. For neuropathy, the doctor may prescribe the following physical procedures:
- Electrophoresis . Thanks to the dispersion of tiny particles under the influence of an electric field, electrophoresis conducts drugs deep under the epidermal layer. Analgesics, antispasmodics (Analgin, Baralgin), vitamins, Prozerin and many other drugs are used for electrophoresis.
- Magnetotherapy . The magnetic field has a beneficial effect on blood circulation and the conduction of nerve signals.
- Ultrasound therapy (UT) . Exposure to ultra-high frequency vibrations (800-3000 kHz) improves metabolism at the cellular level and accelerates the restoration of damaged tissues.
- Amplipulse therapy . A sinusoidal current with a frequency of 5-10 kHz penetrates well through the skin, activates nerve fibers, and also stops inflammation and has an analgesic effect.
Reference . Neuropathy of the extremities is a disease that is fraught with dangerous consequences, including disability, and therefore requires competent diagnosis and prompt, adequate treatment.
To avoid neuropathy of everyday origin, follow simple everyday rules:
- Shoes should not be tight on the foot..
- Posture should be straight when sitting, standing, and when walking.
- You need to sleep on a hard bed with a properly selected pillow.
- Sufficient physical activity keeps muscles toned.
- The diet should be balanced, including a sufficient amount of grains, greens, nuts and other foods rich in B vitamins.
If you notice any symptoms that even remotely resemble neuropathy, consult a neurologist for advice.
Diabetic polyneuropathy ICD-10 code, symptoms, causes and treatment
› Treatment
This type of disease occurs in most cases due to dysfunction of the endocrine glands, as a result of a deficiency of necessary hormones, or when the functions of other internal human organs are impaired. The following types are distinguished:
- Diabetic polyneuropathy can begin acutely, progress slowly or quite rapidly. It first appears as pain and loss of sensation in the limbs.
- Polyneuropathy associated with paraproteinemia and dysproteinemia occurs mainly in older people and is associated with diseases such as multiple myeloma and macroglobulinemia. Clinical manifestations are expressed in pain and paresis of the lower and upper extremities.
- Polyneuropathy also develops in diffuse connective tissue diseases: rheumatoid arthritis, systemic lupus erythematosus, scleroderma.
- Hepatic polyneuropathy is a consequence of diabetes and alcoholism and has similar clinical manifestations.
- Neurological disorders in gastrointestinal diseases are associated with pathology of the digestive organs, leading to vitamin deficiencies. Celiac disease can provoke polyneuropathy, which is expressed in psychomotor impairment, epilepsy, visual disturbances, and ataxia.
General clinical picture of polyneuropathies
motor sensory Sensitivity disorders can manifest themselves as the following symptoms:
- hypoesthesia ( decreased sensitivity
); - anesthesia ( lack of sensitivity
); - hyperesthesia ( increased sensitivity
); - hyperalgesia ( increased pain sensitivity
); - hypalgesia ( decreased pain sensitivity
); - paresthesia ( spontaneous sensations of pressure, tingling, current flow, goose bumps and others
); - neuralgia ( pain in the area of nerve innervation
).
sensitive areflexia , disturbance of gait and coordination of movements, sensation of pain when exposed to stimuli that usually do not cause it
distant ones , more often in the evening and at night. Motor manifestations of polyneuropathy include the following:
- muscle weakness ( usually tetraparesis or lower paraparesis
); - muscle hypotonia ( reduced degree of muscle tension or resistance to movement
); - atrophy ( wasting or loss of vitality
) of muscles; - tremor ( shaking
); - neuromyotonia ( a state of constant muscle tension or spasm
); - fasciculations ( uncontrollable short-term muscle contractions visible through the skin
); - muscle spasms.
impotence The main clinical manifestations of autonomic neuropathy are:
- orthostatic hypotension ( decrease in blood pressure as a result of a change in body position from horizontal to vertical
); - heart rhythm disturbance;
- disruption of physiological daily fluctuations in blood pressure;
- postural tachycardia ( an increase in heart rate when standing up and a decrease when returning to a horizontal position
); - latent myocardial ischemia ( myocardial damage as a result of a decrease or cessation of blood supply to the heart muscle
); - increased risk of sudden death;
- dysfunction of the esophagus and stomach;
- intestinal dysfunction ( constipation or diarrhea
); - damage to the gallbladder ( stagnation of bile, cholecystitis
); - disturbance of urination ( difficulty in emptying the bladder, weakening of the urinary stream, change in the frequency of urination, urinary retention
); - erectile dysfunction ( inability to obtain or maintain an erection, retrograde ejaculation
); - sweating disorders;
- disruption of the innervation of the pupils.
Dysmetabolic polyneuropathies
diabetes mellitus renal failure
Diabetic polyneuropathy
glucose
https://youtu.
be/rHc_ElQZ-RY"> loss of pain sensitivity of the femoral, sciatic, ulnar, oculomotor, trigeminal, abducens
itchy blood sugar levels diet
600 mg intravenously or orally 100 mg of each substance orally according to the scheme 100/100/1 mg intramuscularly
ibuprofen
orally 400 - 800 mg 2 - 4 times a day
naproxen
250 - 500 mg 2 times a day
antidepressants amitriptyline
10 - 150 mg orally 900 – 3600 mg orally
carbamazepine
200 – 800 mg orally
acupuncture treatment method treatment by bathing in mineral waters
gymnasticsmassagephysiotherapy
Uremic polyneuropathy
creatinine rate of blood passing through the kidneys
glomerulonephritispyelonephritis
polycystic disease, Fanconi syndrome, Alport syndrome paralysis of all four limbs
visiondialysis
Features of treatment of the disease
Toxic polyneuropathy, the treatment of which primarily comes down to eliminating the causes of its occurrence, should be considered comprehensively.
Depending on the type of disease and the severity of its course, the following medications are prescribed:
- "Tramadol" and "Analgin" - for severe pain.
- "Methylprednisolone" - for particularly severe cases of the disease.
- “Pentoxifylline”, “Vazonit”, “Trental” - to increase blood flow in the vessels of nerve fibers.
- B vitamins.
- "Piracetam" and "Mildronate" - to enhance the absorption of nutrients by tissues.
- electrical stimulation of the nervous system;
- massotherapy;
- magnetic stimulation of the nervous system;
- indirect effects on organs;
- hemodialysis, blood purification.
- Exercise therapy.
It is up to the doctor to decide which method of treating polyneuropathy is most appropriate in a particular case. It is absolutely impossible to ignore the symptoms of the disease. Acute polyneuropathy can become chronic, which threatens loss of sensation in the limbs, muscle atrophy and complete immobility.
Diabetic polyneuropathy of the lower extremities according to ICD-10
This diagnosis is most often heard by patients who suffer from diabetes.
This disease affects the body when the peripheral system and its fibers are significantly disrupted. It can be triggered by a variety of factors.