Migraine is a very ancient and common disease; the symptoms and treatment of migraine are mentioned in many historical sources. Very prominent people suffered from this insidious disease, such as Tchaikovsky, Julius Caesar, Charles Darwin, Isaac Newton, Sigmund Freud, Chekhov and others.
Migraine is considered a hereditary, genetic disease that occurs in people of working age (What is migraine). Although the disease is not fatal, however, during attacks a person becomes incapacitated, which negatively affects various factors of his life - it affects work, family, and attitude towards himself and life. How to treat migraine for a person with frequent attacks that worsen the quality of life?
While the financial costs of diagnosing and treating migraines throughout life are truly enormous, they can be compared with the costs of diseases of the cardiovascular system. Therefore, it is very important for the attending physician to find effective methods of treating migraine, taking into account the individual characteristics of a particular patient, to carry out the optimal selection of high-quality, modern and safe medications to relieve migraine attacks in each specific case.
What does migraine with aura mean?
Migraine with aura is a disorder characterized by recurrent episodes of reversible local neurological symptoms (aura), usually increasing over 5-20 minutes and lasting no more than 60 minutes.
“Aura” is a term by which doctors mean the following:
- Visual impairment
. These can be lines, lights, spots, flickering. In severe cases, loss of vision. All manifestations are reversible. - Sensory perception disorders
. It seems that goosebumps are crawling all over the body, the person feels tingling, and there may be areas of numbness. All this is also reversible. - Speech disorders
, which also go away along with the attack.
In 73% of migraine attacks with aura, the headache begins not after the end of the aura, but during the aura itself and can be accompanied by other migraine symptoms - nausea (51%), photophobia (88%) and phonophobia (73%) i Morozova O.G. Migraine: new international criteria for diagnosis and principles of therapy based on evidence-based medicine and our own clinical experience / O.G. Morozova // International Neurological Journal. — 2021. — No. 3 (81). — pp. 131-138. . It happens that a panic migraine develops. Its complications are fear, anxiety, etc.
Migraines with and without aura are the same. A person usually feels a throbbing pain in one side of the head. Often it is concentrated in the eyeball. The pain intensifies with movement, sound and light stimuli. It can last from 4 hours to 3 days. At this time, it is impossible to lead a normal lifestyle. A person wants to be left alone in a dark and cool room, freeze, hide under the blanket. Typically, patients describe the pain as “bursting,” “splitting,” “about to burst,” “every sound like a hammer on the head.” And even after an attack, the consequences persist. The person is apathetic, tired and overwhelmed. It takes more than one day to recover.
Migraine symptoms
Doctors have found that women more often suffer from migraine attacks (7 times a month, men 6 times), the attacks last longer (in women 7.5 hours, in men 6.5). In women, the most common cause of an attack is changes in the weather - atmospheric pressure, air temperature, in men - physical stress. During an attack, women are hypersensitive to odors and experience nausea, while men are more likely to report depression and light sensitivity.
- Sometimes before a migraine attack there are precursors or a prodrome, they are expressed by weakness, inability to concentrate, and there is also a postdrome - general weakness, yawning and pallor of the skin immediately after the attack.
- With migraine, the symptom that distinguishes it from other headaches is a throbbing, pressing pain that affects only one half of the head, and it most often begins from the temple, spreading to the forehead and eyes.
- Sometimes migraine pain is localized in the occipital region, then moving to the entire half of the head.
- Periodically, the sides of localization change; once an attack occurs on the left side, another on the right.
- A distinctive feature of this disease is that at least one of the symptoms of migraine will necessarily accompany the attack - nausea, with or without vomiting, and sensitivity to sound or photophobia.
- Increased headaches are caused by sudden movements, during normal walking, or when climbing stairs.
- Migraine is quite rare in children; it is accompanied by drowsiness and usually goes away after sleep.
- Most often, women suffer from migraines, since in a third of all migraine attacks in women, the migraine provocateur is menstruation. If a migraine lasts 2 days from the beginning of menstruation, it is a menstrual migraine, which occurs in 10% of cases.
- Also, the use of HRT (hormonal drugs for menopause, non-hormonal drugs for menopause) and the use of oral contraceptives - hormonal contraceptives - increases the frequency of attacks and the intensity of pain in 80% of cases.
Other symptoms of migraine that may not appear include redness or, conversely, paleness of the face, increased fatigue, weakness, depression, irritability or anxiety. During an attack, the patient is in a state of increased sensitivity to everything - to noise, light, movement and everything that happens around him; most often he withdraws and tries to retire to a dark, quiet place, the desire to take a horizontal position is especially strong.
The pain of a migraine literally has nothing to compare with, it is so painful, debilitating and most often long-lasting. The intensity and frequency of attacks is very individual, for some they bother them once every six months, for others 2-4 times a month, the pain can be mild or very strong, with frequent vomiting. When moving, the temporal artery tenses, pulsates, and the headache intensifies.
Any unilateral headaches, both constant and recurring, but not characteristic of migraine, require prompt examination to exclude possible organic brain damage!
Differences from migraine without aura
Migraine without aura is called “classic”. Approximately 80% of patients suffer from it. A migraine without an aura manifests itself as throbbing pain at one point. It is not preceded by any visual, auditory or sensory impairment. Sometimes people don’t even realize that it’s a migraine, but think that they just have a headache. For this reason, patients do not go to the doctor, which is fraught with consequences.
You have migraine without aura if the following symptoms are present:
- 5 episodes of pain.
- The attacks last from 4 to 72 hours if you do not take medication.
- The pain throbs and is concentrated on one side of the head. The forehead, neck, and then the face or back of the head may hurt.
- With any physical activity the pain gets worse.
- There may be nausea, fear of light, sounds, voices.
Symptoms
Chronic migraine is characterized by a sudden attack of headache - in just a few seconds, barely noticeable discomfort in one part of the skull spreads to all its parts. A person loses the ability to navigate in external space and control himself.
The nature of the pain has its own characteristics:
- felt at one point, rarely diffuse;
- people describe the discomfort as a pulsation, a squeezing hoop;
- The duration of the episode is from 2-5 minutes to 2-3 days.
Against the background of the main symptom of migraine, other manifestations of pathology are observed:
- at the peak of pain, vomiting appears, which does not improve the patient’s well-being;
- photophobia – sunlight provokes lacrimation and pain in the eyes;
- inadequate reaction to loud sounds - they increase discomfort inside the skull;
- consciousness - as a rule, remains clear, but sometimes it can become confused, the perception of surrounding events changes;
- sense organs - a person can see hallucinations, his sense of smell and skin sensitivity are distorted.
What are the characteristics of migraine with aura?
About 20% of patients experience an aura. But only a few say that it occurs with every attack. The most common symptom of an aura is visual disturbances. Less commonly – sensory organ disorders (tingling, numbness, goosebumps). Aura symptoms are divided into positive and negative. In the first case, something is felt, and in the second, the fields of vision disappear or the hands go numb. Another property of the aura is dynamism. That is, a gradual increase in symptoms, and then their gradual decline. Usually the aura is replaced by a headache, but sometimes the aura appears on its own.
Migraine with aura is characterized by the following symptoms:
- Two episodes of migraine without aura.
- The presence of an aura for 1 hour or more before pain occurs. In this case, the following neurological symptoms appear - one or more:
- visual disturbances – photophobia, blinking, black spots in the field of vision, flickering arches, lines, zigzags, incorrect perception of objects in the field of vision;
- sound disorders, mainly intolerance to any sounds;
- speech problems;
- sensory disturbances – tingling, burning, numbness, etc.;
- impairment of motor abilities, such as sudden weakening of muscles on one side of the body.
Migraine treatment
Treatment of migraine involves 2 main directions - stopping an attack that has already developed, and preventing the occurrence of attacks in the future.
Stopping an attack. Only a neurologist can prescribe any pain relief during a migraine attack; it depends on the intensity and duration. If the attack is of moderate or mild severity and lasts no more than 2 days, then the doctor prescribes simple analgesics, possibly combined.
- NSAIDs (ibuprofen), paracetamol (contraindicated in kidney and liver pathologies), acetylsalicylic acid (cannot be taken if you are prone to bleeding or have gastrointestinal diseases)
- Combination drugs containing codeine, paracetamol, phenobarbetal and metamizole sodium
- If the intensity of the pain is high, the duration of attacks is more than 2 days, then Triptans for migraine are prescribed (list of all modern triptans, prices, how to take them correctly). They are available in suppositories, solutions, sprays, and infections.
- Non-selective agonists - Ergotamine, etc.
- Auxiliary psychotropic drugs - domperidone, metoclopramide, chlorpromazine.
Triptans are drugs developed 20 years ago and are derivatives of serotonin. They act in several directions at once:
- They have a pronounced analgesic effect, reducing the sensitivity of the trigeminal nerve.
- Triptans act selectively on blood vessels, reducing painful pulsation only in the brain, without affecting the rest of the body's vascular system.
- They act only on special producing substances (receptors) that provoke the appearance of pain, their number is reduced and the pain goes away.
For the classic version of migraine with aura, Papazol taken in the first minutes can help. For some, a hot bath helps, for others, exposure to cold, for others, a pressure chamber alleviates the condition.
Treatment of an acute migraine attack
| NSAIDs + conventional painkillers + antiemetics | in 60% of cases attacks cannot be stopped |
| Naratriptan 2.5 mg | Few side effects, fewer relapses |
| Zolmitriptan 2.5 mg | Fast acting triptan |
| Sumatriptan 50 or 100 mg | The effect manifests itself in 70-80% of patients, after 4 hours it gives effect |
| Sumatriptan, spray, 20 mg | Has a very fast effect |
| Ergotamine | It has mostly been replaced by triptans |
| Sumatriptan subcutaneous, 6 mg | Very effective for severe attacks with vomiting |
Migraine prevention
| b-blockers may cause fatigue and should not be used by persons with bronchial asthma or heart failure |
| Sodium valproate 200 mg | Weight gain and increased drowsiness in 15% of patients limit their use |
| Methysergide 1-2 mg | A common side effect is abdominal pain, rarely fibrosis. |
| Amitriptyline or dothiepine at night 25 mg | Have an analgesic effect if an attack is triggered by stress |
| Aspirin | The effect and dosage are not approved or established, so use is limited |
| Pizotifen 1.5-3.0 mg | It also increases weight, which is contraindicated for many patients; drowsiness is relieved by increasing the dose, gradually over the course of a month. |
General rules for migraines
To reduce the intensity of pain, you should follow some simple rules:
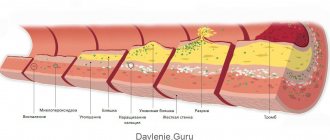
- Giving up bad habits - alcohol and nicotine have a destructive effect on the entire body, including the vascular system.
- Refusal of artificial stimulants - stimulants such as energy drinks (can lead to the death of adolescents), coffee, intense training lead to a large expenditure of energy, which, if prone to migraines, provokes attacks.
- Normalize your sleep and rest schedule; it is during sleep that energy reserves are replenished, especially before 3 am. Scientists have found that after 3 a.m. energy consumption resumes, and staying up late can lead to exhaustion.
- Diet - it is known that processed foods, fast food, pickled, smoked, spicy foods, food additives, flavorings and preservatives clog blood vessels so much that this leads not only to poor circulation and provokes migraine attacks, but also increases the risk of developing atherosclerosis and stroke , heart attack.
- Weak dim lighting, decreased mental activity, frequent exposure to fresh air, light physical work on the street, silence - all this reduces the risk of developing an attack.
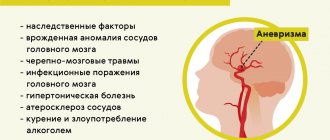
Causes of migraine
The mechanisms of migraine development are not fully understood. A predisposing factor in the development of the disease is hereditarily determined dysfunction of vasomotor regulation. Approximately 70% of migraine patients have close relatives with a history of migraine-like headaches i Morozova O.G. Migraine: modern ideas about classification, diagnosis, therapy and prevention (part I) / O.G. Morozova // Emergency Medicine. - 2012. - No. 4 (43). — P. 32-41. .
There are two groups of factors that influence the course of migraine: those that worsen the course of migraine as a whole and those that provoke an attack.
Factors that worsen the course of migraine . In a patient with migraine, factors such as emotional stress, frequent consumption of alcoholic beverages, and other environmental influences can cause a long-term (over several months or years) worsening of the disease in the form of an increase in the frequency and/or intensity of attacks.
In patients with migraine, precipitating factors increase the likelihood of attacks; their effects usually appear within less than 48 hours. Despite the fact that migraine triggers have been well studied in a number of epidemiological studies (for example, the influence of menstruation i Koreshkina M.I. Modern aspects of diagnosis and treatment of migraine / M.I. Koreshkina // Neurology, neuropsychiatry, psychosomatics. - 2013. - P. 92-96.) and clinical (the effect of aspartame, chocolate, etc.) studies, in each individual case it is not always easy to establish a direct causal relationship between the provocateur and a migraine attack.
Factors provoking migraine paroxysms (migraine triggers) i Morozova O.G. Migraine: modern ideas about classification, diagnosis, therapy and prevention (part I) / O.G. Morozova // Emergency Medicine. - 2012. - No. 4 (43). — P. 32-41. :
- dietary: hunger, irregular nutrition, some foods (chocolate, cheese, nuts, alcohol (red wine), creams, yogurt, chicken liver, avocado, citrus fruits, bananas, concentrated soups, fried pork, sausages, pizza, coffee, cola, tea);
- hormonal: menstruation, ovulation, estrogen replacement therapy, oral contraceptives;
- psychological: emotional stress, anxiety,
- depression, fatigue;
- weather changes;
- exercise stress;
- lack or excess of night sleep;
- stuffiness, odors (smell of perfume);
- visual stimuli (flickering or bright light);
- cold;
- noise;
- staying on top.
Main causes
The exact causes of migraine in men, migraine in children, and migraine in women are still unknown.
However, the factors contributing to its occurrence have been well studied:
- change of environment, sudden change in climate, weather conditions;
- a diet generously flavored with alcoholic beverages (and red wine in particular), various sweeteners present in all current carbonated drinks, nuts, smoked products, confectionery and other products where caffeine, cocoa and chocolate are present in large quantities;
- insomnia, interruptions in sleep patterns, frequent night work, psycho-emotional stress;
- various stressful situations that contribute to sharp jumps in the content of adrenaline and other hormones in the blood;
- taking certain medications and, in particular, self-medication with certain vasodilators, H2-histamine receptor blockers, as well as drugs based on 3,4,5-trimethoxybenzoate methyl reserpate:
- heredity;
- early traumatic brain injury.
Types and symptoms of migraine auras
Let's look at the main types of auras and how they manifest themselves.
Visual or ophthalmological
This aura is called “classical”. With it, visual images appear - flashes of light, curved or straight lines, flickering objects, white or golden figures, spherical images, etc.
Symptoms develop over 5-30 minutes. Positive ones can be replaced by negative ones. The duration of the aura can reach 1 hour. The image usually appears in the center of the visual field. It gradually increases and moves to the periphery. A scotoma remains behind him
– dark, “blind” area. During the aura or within an hour after its appearance, pain occurs. When the attack ends, any disturbances go away without consequences.
Retinal
With such an aura, scotomas or blindness in one eye occur. Symptoms persist for up to 1 hour. The headache comes after scotomas in about an hour, but can also occur before them. This is a rare type of aura. There is an assumption that the symptoms appear due to spasm of the central retinal artery. In most patients, retinal migraine attacks alternate with migraine attacks with or without classic aura.
Auditory
Auditory auras are hallucinations with sound. Ringing in the ears may occur, and patients sometimes hear music or voices. Doctors associate this aura with epileptic activity in the cerebral cortex, in its temporal region.
Speech
It manifests itself as a speech disorder because it affects the speech centers of the brain. Before an attack of pain, for a few minutes, no more, it is difficult or impossible for a person to speak. He can rearrange syllables in words, letters, repeat the same thing. At the same time, the consciousness is absolutely pure.
Vestibular
This is an aura in the form of movement disorders - dizziness. A fairly common phenomenon that can be hidden or obvious. In the second case, a person “sicks” even with small loads. In the first, violations can only be detected within the framework of an examination. According to the ICD, 2 forms of vestibular migraine are distinguished:
- Basilar
- occurs rarely, mainly in teenage girls. The attack begins with visual disturbances, followed by dizziness, tinnitus, sensory disturbances, etc. Then, in 25% of cases, confusion occurs. Neurological symptoms persist for 20-30 minutes, then pain in the back of the head occurs. Without treatment, throbbing pain may persist for 2-3 days. - Paroxysmal dizziness of younger children
(benign). Occurs in children 1-4 years old. It manifests itself as short – from a few seconds to a few minutes – attacks of dizziness. The child loses stability, becomes anxious, and vomits. He may turn pale and sweat profusely. No headache. Attacks may recur over several months or years.
Vegetative
Often such auras are manifested by a feeling of heat, chills, cold, trembling; the face and neck may turn red or pale. Goosebumps may appear, and hairs may even rise on the skin. During an attack, the size of the pupil may change, and asymmetrically. Usually such an attack is part of a complex attack, and not an independent phenomenon.
MIGRAINE AND Dizziness
What is the basis of a migraine aura? What is headless migraine? What is meant by the term “linear migraine”?
According to epidemiological studies, migraine affects 5 to 16% of the population in developed countries. The disease most often occurs in women aged 35-40 years [2, 9, 10]. It is characteristic that its prevalence among the adult population of European and American countries tends to increase [10]. Over the past decade, ideas about migraine have undergone significant changes, due to the rapid growth of scientific research in the field of genetics, pathogenesis and treatment of this disease. Despite the complexity of the pathogenesis of the disease, most doctors recognize that the main victims during a migraine attack are the blood vessels of the brain. The vascular theory proposed back in the late 30s by Wolff [15] considers migraine as a suddenly developing generalized “disruption” of vasomotor regulation, which is manifested by lability of cerebral and peripheral vascular tone. From this point of view, aura during migraine is caused by local spasm of cerebral vessels and the development of cerebral ischemia with the appearance of various focal neurological symptoms (scotoma, hemianopsia, hemihypersthesia, dizziness, etc.). An attack of headache is a consequence of excessive vasodilation of intracranial and extracranial cerebral vessels, and periodic stretching of the vascular wall leads to the activation of pain receptors and gives the headache a pulsating character.
Almost 70% of migraine patients complain of dizziness of various types, occurring both during a migraine attack and in the inter-attack period of the disease, and 50% show symptoms of labyrinthine pain and disturbances in vestibular tests [1, 7, 12]. Cochleovestibular symptoms are most pronounced in the basilar form of migraine, which occurs mainly in adolescents and young women. In most cases, a headache attack is preceded by systemic dizziness, ataxia, nystagmus and tinnitus, which can last from several minutes to an hour. In severe attacks, bilateral blindness, alternating hemiparesis or tetraparesis, oculomotor disorders, diplopia, and vomiting may develop. The peculiarity of basilar migraine is that the neurological symptoms of aura can persist in the phase of headache, which suddenly appears in the occipital region, has a strong pulsating nature and can be accompanied by a short-term loss of consciousness. It is believed that the focal neurological symptoms of aura in basilar migraine are based on deterioration of blood circulation in the vertebrobasilar arteries [2, 3, 7, 13, 14]. Severe variants of basilar migraine should be considered as a complicated form of migraine. Observation of such patients shows that with age, basilar migraine transforms into less severe forms of the disease [2, 3].
Vestibular disorders of a peripheral and central nature are observed not only in basilar, but also in vestibular, ophthalmic, hemiplegic, aphasic and other forms of migraine with aura. In addition, dizziness often occurs during migraine attacks without aura [5, 11, 12]. Of particular interest are cases of so-called decapitated migraine, or according to the international classification of migraine aura without headache [6]. An attack of this form of migraine is characterized by the presence of local, most often visual and vestibular, disorders without subsequent headache. Dizziness can be peripheral or central in nature and accompanied by pyramidal and sensory symptoms. The diagnosis of this form of migraine is probabilistic and requires the exclusion of organic brain diseases, which can manifest as vestibular and cochlear symptoms. Correct diagnosis of migraine aura without headache is helped by hereditary history, age, cyclical nature of attacks, cases of migraine headache, complete regression of symptoms after an attack, further transformation of decapitated migraine into one of the typical forms of migraine with or without aura, as well as the absence of changes in laboratory and instrumental examination.
In childhood, the clinical picture of migraine is quite specific and, along with typical attacks, can manifest itself in the form of so-called migraine equivalents, or according to the modern classification of headaches, periodic syndromes of childhood, which can be precursors of migraine or associated with it [6]. The most common equivalent of migraine in children is recurrent benign paroxysmal vertigo. This syndrome is characterized by the occurrence, against a background of complete health, of short-term attacks of imbalance, systemic dizziness, anxiety, spontaneous nystagmus and vomiting [1, 2]. A neurological examination and additional instrumental studies do not reveal pathological changes in the nervous system or labyrinth in children. With age, attacks acquire the typical features of migraine with headache.
During the interictal period of the disease, 50% of patients with migraine with aura and 46% of patients with migraine without aura exhibit neurological and otological symptoms, indicating the non-random nature of the combination of migraine and vestibular disorders. It has been established that in patients with migraine, benign paroxysmal vertigo, Meniere's disease and vestibular dysfunctions, identified in the study of spontaneous and evoked vestibular reactions, are significantly more common than in the control group [1, 5, 8, 12]. A number of authors express the opinion that there is a hereditary and pathogenetic connection between Meniere’s syndrome, paroxysmal benign vertigo in children and adults, and migraine [5, 11, 12]. Babiyak V.I. and colleagues (1996) believe that Meniere’s disease can, with certain assumptions, be classified as a special case of migraine, namely “labyrinthine migraine” with the phenomena of its “glaucoma” [1].
Dizziness and ataxia are very common symptoms of an attack of so-called cervical migraine (Barré-Lieu syndrome, posterior cervical sympathetic syndrome). For the first time, M. J. Barre (1925) described the symptom complex of headache, visual, auditory and vestibular disorders in patients with osteochondrosis and spondylosis of the cervical spine [3, 7]. The similarity of the clinical picture of posterior cervical sympathetic syndrome with migraine allowed V. Bartschi-Roshen to call it cervical migraine [3]. An attack of cervical migraine can be triggered by a sharp turn of the head or long-term tension in the muscles of the neck and back of the head. Dull, bursting, less often pulsating pain appears in the cervical-occipital region, and then spreads to the entire half of the head and the orbital region. When describing the distribution of headaches, patients figuratively move their palm from the back of the head to the forehead, a gesture that Bartschi-Roschen compared to “removing a helmet.” The side of hemicranial irradiation of pain usually corresponds to the side of cervico-occipital pain. Headache is accompanied by dizziness, noise and ringing in the ears, blurred vision, and sometimes fainting. The duration of the attack can range from 30 seconds to several hours. According to most authors, an attack of cervical migraine occurs as a result of irritation of the sympathetic plexus of the vertebral artery by osteophytes of the uncovertebral joints in individuals with degenerative changes in the cervical spine [2, 3, 7]. In some cases, the pain syndrome is not pronounced, and the symptoms of circulatory disorders in the vertebrobasilar region come to the fore - cochleovestibular, visual and other focal symptoms. Diagnosis of cervical migraine is based on a thorough study of the profile of the headache, the factors that provoke its occurrence, data from a neurological examination and additional X-ray diagnostic methods for examining the cervical spine and craniovertebral region. Differential diagnosis with true migraine is not difficult in most cases.
Treatment of vestibular disorders in patients with migraine is an integral part of a complex of therapeutic measures carried out for this disease, and can be carried out both during an attack and prophylactically during the interictal period of the disease. The main principles of migraine treatment are modification of the lifestyle of patients in order to eliminate the causes that provoke attacks of the disease, and drug therapy. It is assumed that the deterioration of the labyrinthine and cerebral circulation is the main cause of the appearance of “peripheral” and “central” dizziness in migraine [1, 2, 3, 8, 12]. It is believed that if a medicine is able to improve blood circulation in the basin of the vertebrobasilar arteries and their branches, without affecting blood circulation in the basins of other vessels, then it can be used to treat dizziness and related disorders [5, 13, 14] . Today, antihistamines and anticholinergics, diuretics, tranquilizers, barbiturates, calcium channel blockers, and tricyclic antidepressants are offered. This list can be expanded to include b-blockers, anticonvulsants, antigen-converting enzyme inhibitors, dopamine D2 receptor antagonists, phenothiazine derivatives, etc. [1, 4, 8, 13, 14]. Among them, it is difficult to name a drug of first choice for the treatment of dizziness, since their effectiveness in this pathology was discovered “accidentally” during clinical use, and the mechanisms of their vertigolytic action are unknown. Until now, there has been no complete understanding of the properties of a drug suitable for the treatment of dizziness. The research of Takeda and his colleagues (1993) [13] brought some clarity to this issue. The results of their experimental work allowed us to take a new look at the processes of the pathogenesis of dizziness and showed the special role of histamine in the functioning of the vestibular pathways and the regulation of vascular tone in the vertebrobasilar region. The important role of H1 and H3 histamine receptors in providing neurogenic and vascular mechanisms of the vertigolytic action of a number of drugs has been elucidated [4, 13, 14]. It was found that the clinical effect of one of the most effective drugs for the treatment of dizziness, betagestin (Betaserc), is based on a selective improvement in regional circulation in the labyrinth and basilar artery basin without a significant effect on systemic blood pressure. The neuronal mechanism of action of betagestin is associated with the normalization of neuromediation processes in histaminergic neurons of the vestibular nuclei, which determine the central mechanisms of dizziness [4, 14].
Thus, the modern approach to the treatment of vestibular disorders in migraine involves the use of a complex of non-drug and pharmacological interventions aimed at both stopping an already developed attack of migraine and dizziness, and at their prevention. There is no doubt about the need to include the most effective vertigolytic drugs in the treatment regimen for patients suffering from migraine and dizziness.
Literature
- Babiyak V. I., Lantsov A. A., Bazarov V. G. Clinical vestibulology. St. Petersburg: Hippocrates, 1996. 336 p.
- Vein A. M., Kolosova O. A., Yakovlev N. A., Slyusar T. A. Migraine. M., 1995. 180 p.
- Shtok V.N. Headache. M.: Medicine, 1987. 304 p.
- Aanta E. Treatment of acute vestibular vertigo // Acta Otolaryngol (Stockh). 1991. Suppl 479. P. 44-47.
- Cass SP, Ankerstjerne K., Balaban C., Yetister S., Aydogan B. Migraine-related vestibulopathy // Ann Otol Rhinol Laryngol. 1997. No. 106 (3). P. 182-189.
- Classification and Diagnostic Criteria for Headache Disorders, Cranial Neuralgias and Facial Pain, International Headache Society, Cephalalgia. Vol. 8. Suppl. 7. 1988.
- Goadsby PJ Pathophysiology of Migraine: A disease of the Brain // Headache / Goadsby PJ, Silberstein SD (eds). Butterworth-Heinemann. 1997. P. 5-25.
- Gordon CR, Kuritsky A., Doweck I., Spitzer O., Shupak A., Hering R. Verstibulo-ocular reflex in migraine patients: the effect of sodium valproate // Headache 1993. No. 33 (3). P. 29-32.
- Rasmussen BK Epidemiology of migraine // Towards Migraine 2000 / F. Clifford Rose (ed.) Elsevier Science. 1996. P. 1-15.
- Steward WF, Lipton RB Migraine Epidemiology in the United States // Headache Classification and Epidemiology / J. Olesen, ed. New York: Raven Press, 1994. pp. 239-247.
- Split W., Lukomski M. Evaluation of the vestibular system in patients with migraine // Neurol Neurochir Pol. 1988. No. 22 (5). P. 383-386.
- Szirmai A. Vestibular disorders in patients with migraine // Eur Arch Otorhinolaryngol Suppl. 1997. No. 1. S. 55-7.
- Takeda N., Morita M., Hesagawa S., Horii A., Kubo T., Matsunaga T. Neuropharmacology of motion sickness and emesis. Acta Otolaryngol (Stockh), 1993. Suppl 501. P. 10-15.
- Timmerman H. Pharmacotherapy of vertigo: any news to be expected? // Acta Otolaryngol (Stockh). 1994. Suppl 513. P. 28-32.
- Wolff HG Headache and Other Pain. New York: Oxford University Press. 1963.
Diagnosis of migraine with aura
The diagnosis is made by a neurologist, and it is he who should be contacted with such a problem as soon as possible. The doctor must rule out cysts, tumors, encephalitis and vascular pathologies that cause similar symptoms. Therefore, a neurological examination, CT or MRI of the brain is performed, and the patient is sent for a consultation with an ophthalmologist for examination and determination of visual fields.
An EEG (electroencephalography) is required, which provides information about the functional activity and characteristics of the brain biorhythm of a particular patient. Based on the EEG results, the doctor then selects medications for therapy.
How to diagnose
A certain difficulty in the case of men is the timely diagnosis of migraine, since it is based on the complaints expressed by the patient. In order to correctly identify the problem, a doctor must have a wide range of knowledge on this topic.
Among the examinations offered are the following:
- brain screening;
- ultrasound examination of the vessels of the neck and head;
- roencephalogry.
There are signs that help a specialized specialist exclude the disease:
- compressive pain syndrome;
- mild headache;
- localization on both sides;
- discomfort is not increased by physical activities.
Features of migraine manifestations in children and pregnant women
In childhood, the peculiarity of an attack is its short duration, from 30 minutes to several hours, and bilateral pain. It becomes one-sided in adolescence. Most often, children experience pain in the temples, forehead, and periorbital area. The nature of the pain is also not the same as in adults. The pain is squeezing, pounding, slightly throbbing. Children describe the latter extremely rarely.
It is difficult for a child to talk about his feelings, so the intensity of pain is assessed using VAS - a visual analogue scale with points from 0 to 10. Scales with emoticons can be used - from smiling to crying.
During pregnancy, migraines can occur even in those who have not previously suffered from them. In 25% of cases it is migraine with aura. It is much more difficult to tolerate, and there is almost nothing to eliminate the pain due to the delicate position. The approved drugs - No-Shpa, Citramon or Paracetamol - do not help. During pregnancy, aura most often manifests itself as photophobia, withdrawal, intolerance to sounds and strong odors, very severe nausea and the urge to vomit. The main causes of pain during pregnancy:
- consumption of “dangerous” foods – cheese, chocolate, citrus fruits;
- lack of water in the body;
- constant lack of sleep because the stomach makes it very uncomfortable to sleep;
- stress, frequent worries;
- large weight gain;
- violation of metabolic processes.
Stages of attack development
The manifestation of migraine in each patient may have its own characteristics, but the standard attack includes 4 stages. All of them have a time interval between themselves, during which the patient feels well.
Stages of attack development:
- Harbingers. Occurs in almost every second patient. They can appear several hours, minutes or even days before the attack. Most often they are expressed in increased irritability, loss of appetite, fatigue or, conversely, hyperactivity;
- Aura. Characteristic only for 25-30% of patients. In most cases, it is visual in nature: flashes, spots, flickering. Cloudiness or blurred vision may be noted. Some patients have a sensitive aura. They feel goose bumps, numbness, tingling in the limbs, and sometimes in the face. The aura lasts on average 20-30 minutes;
- Headache. This is the most unpleasant part of the attack. The pain can have varying degrees of severity, but most often it is intense and throbbing. It gets worse from physical movements and irritants such as bright light, loud sound, strong smell. Duration varies from several hours to several days. Often accompanied by nausea and vomiting;
- Permission. At this stage, the body recovers from pain. The patient experiences symptoms similar to the warning signs: fatigue, irritability, poor appetite.
In some cases, there may be a lack of certain stages.
Electroencephalography allows you to clarify the diagnosis
How to treat migraine with aura and how to relieve pain effectively and quickly
Since it is almost impossible to avoid an attack if there is a trigger, you need to know ways to improve the condition, because migraine is not a death sentence.
The final diagnosis is made by a neurologist. He will tell you what to do, how to treat the disease, how to increase the intervals between attacks.
Treatment for migraines is based on eliminating the pain and making it happen as little as possible or go away altogether. NSAIDs or specific medications, most often triptans, may be used. Intravenous infusion therapy is also used to treat migraines. The effectiveness of pain relief is directly proportional to the time of taking the drugs. You can stop an attack when it has just begun. Unfortunately, many people miss this moment with the thought “what if it doesn’t hurt.” However, at the peak of an attack, the tablets have almost no effect, because with migraine gastrostasis in the intestines, the absorption of any substances is very difficult.
Alternative ways to alleviate the condition are physical activity, exercise therapy, physiotherapy, and psychotherapy. Massage of the collar area is especially useful, because muscle spasm in this area can provoke an attack. Recently, migraines have been successfully treated with injections of botulinum toxin type A. The injections make remission last longer, and in some cases relieve pain for a very long time.
Treatment of migraines using traditional medicine
Many traditional medicine methods can provide relief from pain.
Ginger root
Ginger has the ability to block prostaglandins, thereby reducing the severity of pain. The same principle applies to most NSPVs. Ginger tea is prepared at home. Ginger root is crushed, then added to boiling water and simmered for 10 minutes over low heat. Next, the tea is filtered and drunk plain or with lemon and honey.
Chamomile
Has an anti-inflammatory and calming effect. You need to take two tablespoons of chamomile in a glass of water and cook the mixture for 5 minutes over low heat. Next, you need to strain the broth and drink it plain or with lemon and honey.
Lavender
Lavender oil is used for inhalation. The solution is prepared as follows: a teaspoon of oil is diluted in three glasses of boiling water. Breathe over the resulting solution for 15 minutes. Lavender oil can be mixed with peppermint oil and apply the mixture to the temples, gently massaging it a little. It is best to combine massage and inhalation.
Treatment options
Treatment of migraine in men is prescribed in accordance with the cause of the disease (if one is identified) and the stage at which the disease is currently located (the period of exacerbation or the period between attacks).
The main areas of treatment are:
- Medications are used to relieve pain, vomiting and other clinical symptoms. The doctor knows how to treat the type of migraine that the patient suffers from. Most often, sedatives are used, in case of nausea - antiemetics, and to relieve pain - anesthetics.
- Between attacks, physiotherapeutic treatment can be prescribed, during which the patient’s body is exposed to magnetic fields and low-frequency electric current. These procedures have a beneficial effect on the state of the cardiovascular system and prevent congestion in the body as a whole.
- Diet. Since the causes of migraines can also lie in the diet, the attending physician identifies unwanted foods that should be excluded from the patient’s menu. In particular, meat dishes, as well as all sweet and cocoa-containing confectionery products, should be excluded from the diet for an indefinite period. Drinking alcohol is also contraindicated. The emphasis in the diet is on fish and dairy products, as well as dishes prepared from fresh vegetables.
- Physical therapy classes. Often, a morning jog and various sets of physical exercises help the patient get rid of nervous tension, which can trigger the development of a migraine attack.
- Acupuncture. Acupuncture is a common way to prevent migraines.
To relieve symptoms during an exacerbation, the following are practiced:
- cold compresses on the head;
- warm baths;
- darkening the room, in the silence of which the patient will have a better opportunity to fall asleep;
- massage of the back of the head and cervical spine.
Taken together, all these measures in most cases help to stop a migraine attack in a man or at least relieve the pain.
But what will really be effective is an entirely comprehensive approach.
What happens if migraine is left untreated?
Migraine is not a harmless disease. The disease is identified by the World Health Organization as a risk factor for cerebral strokes. Numerous epidemiological studies have revealed correlations between migraine and stroke, especially in young women suffering from migraine with aura i Ashina M. Vascular changes have a primary role im migraine / M. Ashina // Cephalalgia. - 2012. - 32. - 5. - P. 428-430. . Migraine is associated with a 16-fold increase in the risk of stroke in pregnancy and the overall risk of cardiovascular events in women. Migraine can be a risk factor not only for stroke, but also for “silent” heart attacks and damage to the white matter of the brain. These changes most often occur in women suffering from migraine with aura, and are associated with severe and frequent migraine attacks i Hadjikhani N. Mechanism of migraine aura revealed by functional MRI in the visual cortex / N. Hadjikhani // Proc. Natl. Acad. Sci USA. - 2001. - 98. - P. 4687-4692. .
You shouldn’t treat the attacks as “survived and are fine”, you need to see a doctor and get treatment.
Time of onset of migraine attacks
Until recently, issues of the representation and severity of pain syndromes in the sleep-wake cycle and their impact on the quality of life were practically not considered. In recent years, the most large-scale studies in this direction have been carried out in the USA. According to a mass telephone survey (1997-1998) of the population over 18 years of age, it was shown that about 94 million people had complaints of night pain. It was later shown that back pain (64%) and headaches (56%) dominated among them.
It is known that the vast majority of migraine patients experience attacks during active wakefulness. Some patients, along with daytime attacks, also have night attacks. Migraine attacks that occur during night sleep are more typical for older patients; There is evidence of the possible effectiveness of lithium preparations for nocturnal migraine.
The features of waking migraine and sleep migraine were first considered in the work of our employee L.A. Bobeyko (1994), however, the compared groups were not completely “polar”: they included patients with predominantly (and not exclusively) nocturnal and daytime migraine attacks. It was shown that sleep migraine is characterized by a polymorphism of psycho-vegetative disorders, the predominance of left-sided attacks, sleep disturbances in the periods between attacks, and the presence of autonomic disorders during sleep, which was regarded as a prerequisite for the development of a sleep attack.
Migraine prevention
Prevention involves taking the medicine daily for a certain period of time. Which one is prescribed by a neurologist individually. This medicine will act not on the symptoms, but on the cause of the disease, preventing attacks from developing. However, drug prevention is not indicated for everyone. It is prescribed if:
- number of attacks – up to 8 per month or 2 per week;
- Even specific anti-migraine medications - Zomig, Relpax and other triptans - hardly help the patient;
- Triptans and analgesics cannot be taken due to contraindications;
- The patient has hemiplegic migraine, a rare hereditary disease that leads to stroke.
Migraine - what is it
Migraine is a serious neurological disease caused by changes in the functioning of the brain. In the international classification of diseases it is mentioned as an independent disease (code/code IBC 10 - G43). But this is only a scientific definition of the disease, and in order to truly understand what is behind it, to understand the seriousness of the disease, you need to learn about the main thing: what causes a severe headache and how it affects the brain.
The main symptom of a migraine is throbbing pain, usually on only one side of the head (usually the right). As a rule, during an attack, the patient feels sick, his perception of light and sounds is impaired, it is difficult for him to move and speak, and in some cases he even hallucinates. Hopes that the attack will go away on its own are rarely justified. Without the right medication, daily pain can recur throughout the week. But what causes the pulsation in the head of migraine sufferers: a spasm, an inflammatory process, or something else?
Experts often associate the onset of a migraine attack with the activity of the hormone serotonin. There is even a so-called serotonin theory of migraine. In our bodies, this hormone has a special function: it helps regulate the sensitivity of the nervous system. In other words, it prevents and alleviates pain. If hormone levels decrease, certain parts of the brain become hypersensitive, including the trigeminal nerve. As a result, neuropeptides are released, which cause spasm and excessive dilation of brain vessels, which in turn further irritate pain receptors. That is, migraine pain is caused by inflamed and dilated blood vessels in the brain.
Migraine is an extremely common disease. The total number of people with throbbing pain exceeds the number of people suffering from diabetes, asthma or coronary artery disease. According to the latest estimates by WHO experts, there are more than 127 million people living in the world with chronic migraine. By the way, this is one of the oldest diseases known to man. Descriptions of the signs of the disease (and in some cases even methods of treatment) are found in the texts of the Babylonians, Sumerians, Egyptian papyri, and the writings of Herodotus, Hippocrates, Paracelsus and other ancient healers. It is interesting that in the most ancient times, evil spirits were called the cause of severe headaches, and to treat the patient they often resorted to craniotomy. Nowadays, doctors use less radical methods, although some of them include surgical ones.
Some types of migraine are hereditary, although in most cases the tendency to the disease is transmitted through the female line. According to American researchers, approximately 10% of school-age children suffer from regular migraine attacks. In most cases, attacks in children begin at 5-6 years of age, although there is also the so-called infant migraine. Recently, more and more researchers have expressed the opinion that, in fact, colic in newborns is not a problem with the functioning of the stomach, but a real attack of abdominal infant migraine. But still, more often, the first attacks in girls occur during puberty (at about 13-14 years old), less often in older girls (closer to 20 years old), and in boys migraine usually begins at 8-10 years old. There are exceptions. For example, in some women the disease begins only after the first birth, during breastfeeding. The peak development of the disease in both sexes occurs at approximately 20-30 years of age, and after 40 years of age, the frequency of attacks decreases. In women, attacks usually end after menopause. By the way, researchers have calculated that among women suffering from painful headaches there are approximately 3 times more women than men, but in men the attacks are more severe.
It is also interesting that the tendency to migraine is largely determined by a person’s character. It is believed that headaches more often plague strong, active, ambitious, perfectionist individuals, that is, those who try to achieve success in life at any cost. Maybe that’s why in all centuries migraine was considered a disease of aristocrats and the powerful? They say that Julius Caesar, Alexander the Great, Peter I, Elizabeth I, Napoleon, Beethoven, Chopin, Tchaikovsky, Nobel, Pascal, Chekhov, Nietzsche, Heine and many others suffered from this disease. Among modern celebrities, headaches complicate the life of tennis player Serena Williams, actors Whoopi Goldberg, Lisa Kudrow, Marcia Cross, Ben Affleck, singers Janet Jackson and Sting. And this is only a small fraction of those who had to learn to live with migraine attacks.
Migraine classification ICD-10
Migraine is coded G43: Diseases of the nervous system => Episodic and paroxysmal disorders => Migraine.
| Code | Disease |
| G43.0 | Migraine without aura (simple) |
| G43.1 | Migraine with aura (classic) |
| G43.2 | Migrainous status |
| G43.3 | Complicated migraine |
| G43.8 | Other migraine |
| G43.9 | Migraine, unspecified |
Diagnostics
The patient's headache has characteristic features that immediately suggest a migraine. For diagnosis, the doctor uses the following methods:
- collecting complaints and medical history to determine the nature of the pain; special attention is paid to: the time of onset and end of the attack;
- provoking factors;
- nature of pain;
- the absence or presence of an aura, its symptoms;
- well-being after an attack;
If necessary, additional examinations and consultations with specialists are prescribed. The diagnosis of migraine is made by exclusion when no other causes of headache have been identified.
Make an appointment
Sources:
- Ashina M. Vascular changes have a primary role in migraine / M. Ashina // Cephalalgia. - 2012. - 32. - 5. - P. 428-430.
- Hadjikhani N. Mechanism of migraine aura revealed by functional MRI in the visual cortex / N. Hadjikhani // Proc. Natl. Acad. Sci USA. - 2001. - 98. - P. 4687-4692.
- Esin O.R. Migraine: Basic principles of treatment and prevention / O.R. Esin [et al.] // Clinician. - 2011. - No. 4. - P. 10-16.
- Koreshkina M.I. Modern aspects of diagnosis and treatment of migraine / M.I. Koreshkina // Neurology, neuropsychiatry, psychosomatics. - 2013. - pp. 92-96.
- Morozova O.G. Migraine: new international criteria for diagnosis and principles of therapy based on evidence-based medicine and our own clinical experience / O.G. Morozova // International Neurological Journal. — 2021. — No. 3 (81). — pp. 131-138.
- Morozova O.G. Migraine: modern ideas about classification, diagnosis, therapy and prevention (part I) / O.G. Morozova // Emergency Medicine. - 2012. - No. 4 (43). — P. 32-41.
Prevention
Prevention of migraine attacks is not only properly selected drug therapy, but also correction of the patient’s lifestyle. Doctors recommend:
- normalize sleep: for the normal functioning of the body, at least 8 hours of night sleep every day are required;
- minimize the consumption of foods that can cause an attack, especially chocolate, spices, and alcoholic beverages;
- eliminate smoking;
- adhere to a balanced diet with a mandatory breakfast and intervals between meals of no more than 5 hours;
- observe the drinking regime and consume at least 1.5-2 liters of clean water per day; in hot weather this amount can reach 2.5-3 liters;
- establish a work and rest schedule, avoid mental and physical fatigue;
- reduce stress levels as much as possible;
- make a habit of light or moderate physical activity: swimming, walking, cycling, yoga, Pilates;
- promptly identify and treat chronic diseases, especially osteochondrosis of the cervical spine, atherosclerosis and other pathologies that contribute to the deterioration of blood flow in the brain.
Regular health resort treatment of a restorative nature and tourist trips without extreme changes in climate and time zones have a good effect.