What is fetal acrania?
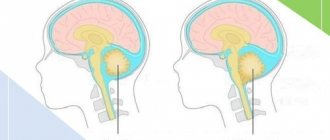
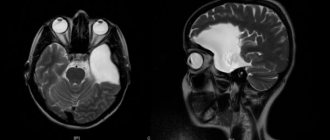
Acrania is a developmental disorder of the central nervous system in the fetus, one of the most common intrauterine developmental pathologies. This anomaly is characterized by the fact that the fetal head contains absolutely no bony vault. To put it more clearly, the fetus lacks the upper part of the skull, the function of which is to cover the brain and protect it from any environmental influences. In addition to this non-life-threatening problem, there is also no skin on the head, which means that the brain is not protected by anything other than brain tissue. The fetal brain itself is underdeveloped and appears as open vessels, connective tissue, and brain tissue that are visible on a misshapen-looking skull.
Pathologies
Spina bifida and problems with the development of the spinal cord are very common. The back part of the brain, which appears as a deformation of the spine or skull, is directly associated with a disease called “notencephaly”. The facial part of the skull is also severely skewed, since this area lacks a huge amount of bone tissue of the skull, and this, in turn, is fraught with strong protrusion of the eyes forward. Among other things, this pathology of fetal development is characterized by an underdeveloped neck, which causes the head to be thrown back so much that it literally lies on the body. In general, acrania is a disease that results from a congenital brain defect. But the pathologies do not end there. Among other things, a sick fetus may have abnormalities in the abdominal cavity, displacement of tissues and organs to the point that they may fall out (ectopia), underdeveloped adrenal glands, prolapse of abdominal organs due to poor development of its wall (eventration) and much more.
Competition “Bio/Mol/Text”-2020/2021
This work was published in the “Academy & Business” category of the “Bio/Mol/Text” competition - 2020/2021.
The general partner of the competition is the annual biotechnology conference BiotechClub, organized by the international innovative biotechnology company BIOCAD.
The sponsor of the competition is SkyGen: a leading distributor of life science products on the Russian market.
Competition sponsor: the largest supplier of equipment, reagents and consumables for biological research and production.
"Book" sponsor of the competition - "Alpina Non-Fiction"
All passionate people have a need to satisfy their curiosity. Some of us are lucky enough to be able to do this during business hours using taxpayer or consumer money. At first glance, such a process with unpredictable results may seem like an inefficient use of resources. But that's not true. Technological breakthroughs only happen when someone takes risks, lets their imagination run wild, and uses resources in unexpected ways. Moreover, if the result of His Majesty’s Experiment is known in advance, then this is no longer an experiment, but a copying of someone else’s idea. Let me note that creative activity is difficult to carry out under orders. “Ivanov, by the 31st I expect five insights from you,” sounds funny, but real. Most scientific discoveries do not provide any direct benefit to society. Fundamental science creates the basis for applied science; the end result is an article in a peer-reviewed scientific journal, that is, an idea with a fixed priority. Applied science rather uses these articles in an attempt to find application for them; the end result is a patent, that is, a copy-protected option for using an idea. Patents can be used by businesses to create commercially available products that satisfy consumer needs and increase their investment. The result is a pyramid: “a heap of ideas → a handful of applications → a pinch of products.” It’s not ideal, but there is nothing more effective - this is the only way ideas become commercially available products [1]. In this post, we will look at one of the successful examples that (slightly) changed the world.
Causes
The main reasons are not directly related to smoking, drinking alcohol, drugs, and so on (although, of course, this can provoke the manifestation of acrania in the fetus, like many other problems relating to the central nervous system), and, unfortunately, this defect can also affect normal parents, especially if they live in an area with highly elevated background radiation. The main causes of the disease are slightly different complications in the health of the parents, which include:
- HIV infection and AIDS;
- Rubella virus in one of the parents or both at once;
- Coxsackie virus;
- Herpes virus;
- Cytomegaly virus.
The fetus can also be affected in women who have been exposed to acute toxic influences, acute hypoxia (lack of oxygen), radiation energy, and those who take medications such as quinine and hydantoin. It is also worth noting that acrania can develop without certain clear reasons against the background of genetic mutations.
How to non-invasively diagnose aneuploidy?
In 1969, cells containing Y chromosomes were discovered in the blood of a pregnant woman [6]. As a result of the birth, a boy was born. Thus, it became clear that fetal cells can be in the blood of a pregnant woman. However, such cells are few in number, making it difficult to develop routine diagnostic tests [7]. Then in 1997, fetal DNA (from the Latin fetus - fetus) was discovered in the blood plasma of pregnant women [8]. I note that plasma is a liquid cell-free fraction of blood in which formed elements, that is, blood cells, are suspended. Thus, as a result of such a minimally invasive procedure as taking the blood of a pregnant woman, the DNA of the fetus can be examined. However, the level of technology development existing at the beginning of the 2000s did not provide for a routine solution for diagnosing aneuploidies [9].
What does high-throughput sequencing have to do with it?
Sometimes, as a result of the creativity of scientists and the transformation of emerging ideas into a commercially available product, the world changes. In 2005, a revolution occurred. 454 Life Sciences began selling the first high-throughput sequencing device [10]. This approach was based on an idea published in 1998 [11]. Then, in competition, the pioneering technology lost to other methods [12]. Nowadays, sequencers manufactured by Illumina and Thermo Fisher Scientific are most often used [13]. These technologies are not perfect - the original nucleic acids serve as a template for creating new DNA fragments. That is, at the preparatory stage, distortions are possible, the contribution of which is difficult to assess. In other words, indirect sequencing occurs - not the original sequences are identified, but derivatives from the original ones. Recently, methods for direct sequencing of nucleic acids have appeared - technologies from Oxford Nanopore [14] and Pacific Biosciences [13] allow sequencing nucleic acids without intermediaries.
But none of this matters. The world has changed - it has become possible to simultaneously sequence many nucleotide sequences, which has reduced the cost of a number of studies by several orders of magnitude. For example, sequencing the human genome using a method described in the late 1970s [15] cost several billion dollars in the late 1990s and early 2000s. Now, obtaining similar data will cost several hundred dollars. Non-invasive diagnosis of aneuploidies has essentially become possible thanks to this technological revolution.
The study of fetal DNA from the cell-free fraction of blood, that is, plasma, has become accessible due to the advent of high-throughput sequencing methods. There are different ways to perform this analysis. The method patented by Natera has entered widespread clinical practice [16]. For the study, cell-free DNA is isolated from the blood plasma of a pregnant woman. Some pieces of this DNA are then amplified and sequenced. In parallel, the same is done with the genomic DNA of mom and dad. The result is high-throughput sequencing data arrays that encrypt information about tens of thousands of single nucleotide polymorphisms (SNPs). This big data is processed using an appropriate algorithm [17].
What is a single nucleotide polymorphism?
Normally, the nucleotide sequences of one human organism are duplicated. We get 23 chromosomes from mom and 23 chromosomes from dad. This means that each position in the genome exists in two variants, or alleles. Moreover, some positions of the genome do not coincide in different people, that is, they are polymorphic. And it happens that one person has different nucleotides on two alleles at the same position. If one nucleotide is not the same, but the neighboring nucleotides surrounding it are the same, then it is a single nucleotide polymorphism (SNP). For example, in Masha, at position 231 of the qwerty gene, nucleotide G (deoxyguanosine-5′-monophosphate) is located on both alleles. And in Petya, in the same position, one allele is G, and the other is C. This means that for Masha and Petya this position is polymorphic. And for one, Petya, by the way, is also polymorphic. Now imagine that we are considering the entire human population - then there will be quite a lot of such SNPs.
The NATERA method considers only the two most common SNP variants. To simplify, let’s denote the first variant of the SNP by the symbol “A”, and the second by the symbol “B”. If you sequence one human organism, then there are three possible combinations of SNPs from two chromosomes: AA, AB and BB. For each SNP, the frequency of occurrence of SNP “A”, that is, fraction “A”, is measured. For the AA combination this value will be 100%, for the AB combination - 50%, and for the BB combination - 0%. Now let's complicate the task - let the sample contain DNA from two different organisms. Then, if in both organisms the SNP is present in the same variant AA, then the frequency of A will be 100%. But it is also possible that in one organism there is a combination of AA (on two chromosomes the same SNP - “A”), and in another - AB (on one chromosome the SNP “A”, and on the second - “B”). Then the total fraction “A” will be less than 100%. This value depends on the ratio between the amount of DNA from different organisms in the sample. If maternal DNA is 99% and fetal DNA is 1%, then the difference will be invisible to the human eye. And if maternal DNA is 50%, and fetal DNA is also 50%, then the frequency of “A” in the mixture will be 75%. And so on - different combinations of variants AA, AB, BB from two different organisms are possible. A similar situation can be illustrated with a graph (Fig. 2 and 3). The SNPs under study are arranged along the abscissa according to their location in the genome; fractions “A” for each SNP are placed along the ordinate. If both organisms contain the normal number of chromosomes, the result will be something similar to Figure 2. The contribution of fetal DNA results in the distribution of points into distinct fingerprint clusters, which can be used to determine the copy number of a chromosome.
Figure 2. Visualization of the results of sequencing of cell-free DNA in the blood plasma of a pregnant woman. The NATERA method considers SNPs for which two nucleotide variants are possible. For simplicity, the first variant of the SNP is designated by the symbol “A”, and the second by the symbol “B”. The proportion of fetal DNA in the sample was 28.1%. All SNPs are located on the x-axis according to their position in the chromosome. The name of the chromosomes is indicated above the graph. Each dot represents one SNP, where the exact position on the Y axis represents the combined "A" fraction of maternal and fetal DNA. The red dots correspond to the combination of AA variants in the mother on two chromosomes, the blue dots correspond to the BB combination, and the green dots correspond to the AB combination. There are no traces of aneuploidy in the sample. There are also no SNPs belonging to the Y chromosome, that is, the fetus is female.
[18]
Now let’s imagine a situation where one of the fetal chromosomes is duplicated. Then you will get something similar to Figure 3.
Figure 3. Visualization of the results of sequencing of cell-free DNA in the blood plasma of a pregnant woman. The proportion of fetal DNA in the sample was 19.2%. The description of this figure is similar to the previous one.
[18]
Figure 3 shows that the “A” frequency distribution pattern for SNPs of the 13th chromosome differs from the “A” fraction distribution pattern for SNPs of the 18th, 21st and X chromosomes. This means that the fetus has three 13th chromosomes. This condition is called Patau syndrome, in which severe birth defects are observed. It should be noted that with a small proportion of fetal DNA in the extracellular DNA of the blood plasma of a pregnant woman, the distribution patterns of fraction “A” for SNPs of different chromosomes are indistinguishable to the human eye in case of aneuploidy in the fetus. Distortions of the distribution of fractions “A” invisible to the eye can be distinguished using automated data processing based on the developed algorithm [18]. Thus, a non-invasive procedure (blood sampling from a pregnant woman) makes it possible to detect aneuploidy in the fetus.
When does the disease begin to appear?
Disturbances in the formation of the central nervous system of the fetus appear in the earliest periods of its development. Acrania develops already 28 days from the moment of conception. One of the most severe malformations of the fetus occurs at the stage of the neural tube, that is, somewhere in the third week of its development in the womb. But such early formation does not at all guarantee its detection in the very first stages of pregnancy.
Basically, the most reliable and accurate diagnosis is made using ultrasound examination after the twelfth week of a woman’s pregnancy. If, during the examination, the brain tissue is clearly visible on the monitor at a time when the main bone tissues should already be formed, then the diagnosis is confirmed.
Development of the nervous system in the first trimester
After fertilization, the egg begins active division, moving through the fallopian tubes. During this time (5-10 days), a multicellular spherical morula is formed, which is embedded in the endometrium of the uterus. From this moment, the development of the fertilized egg and embryo begins.
The morula takes shape, leaves (ectoderm, mesoderm, endoderm) and vital organs of the embryo appear - chorion, amnion, yolk sac. The outer layer of ectoderm subsequently forms the brain, spinal cord, peripheral nerves and nodes.
Within seven days, the disc changes shape to a cylindrical one, where the head and tail sections are distinguished with intense cell division. In the fourth week of embryonic development, the neural tube closes.
Normally, the tube begins to close from the head part and, if this does not happen, the embryo dies. In cases where the tail does not close, the embryo continues to develop, but the innervation of the lower body will be impaired.
Among the main causes of tube pathology, doctors identify:
- lack of B vitamins, especially folic acid;
- insufficient intake of microelements (zinc, iodine, iron);
- exposure to embryotoxic factors;
- genetic abnormalities.
The fifth and sixth weeks of embryogenesis are characterized by intensive cell production, their migration and the formation of the rudiments of the central and peripheral nervous system. The anterior and intermediate sections of the brain appear.
By the end of the second month, all the internal organs of the embryo are formed, the growth of the cerebral hemispheres and the development of its cortex continue. At this time, special devices already detect brain activity and impulse transmission.
In the first trimester of pregnancy, the placental barrier has not yet formed, and the embryo is especially vulnerable to adverse effects. Taking alcohol, drugs, medications based on phenobarbital, increased maternal body temperature, hypoxia, stress and other factors are highly likely to lead to malformations of the central nervous system.
To reduce risks, a woman should give up bad habits, especially watch her diet and avoid stress. It is necessary to include in the diet foods rich in B vitamins, calcium, iron, iodine, and additionally take vitamin E and folic acid.
Obstetricians and gynecologists recommend using vitamin complexes that contain vitamin A with caution; its excess can lead to pathologies in the development of embryonic organs, including the brain. The best option is to consume plant-based foods high in provitamin A beta-carotene. Beta-carotene does not have a teratogenic effect and is safe for the baby.
Considering the restructuring of metabolic processes, it is advisable to optimize diet and lifestyle at the stage of pregnancy planning, 3-6 months before conception.