What is fetal hydrocephalus
Hydrocephalus is a pathological accumulation of transudate.
The condition is characterized by increased intracranial pressure. The disease develops due to exposure to an infectious pathogen or a number of third-party causes.
The disease is formed as follows:
- Excessive amounts of fluid drain from the spinal cord area;
- it begins to gradually accumulate in the brain.
Dropsy in pregnant women can occur due to the abnormal structure of the embryo at the stage of conception.
Pathology has several forms:
- primary;
- secondary.
The first type is a disease caused by congenital defects or genetic mutations. The secondary form develops as a result of exposure to infection.
Fetal hydrocephalus can be closed or open. Closed - when there is an obstacle to the drainage of fluid from the head.
Open - cerebrospinal fluid is not absorbed into the bloodstream, and its circulation in the brain is not impaired.
In addition to the acute and chronic course, doctors distinguish external, internal and mixed types of the disease.
Features of dropsy of the brain
Water on the baby's brain is called hydrocephalus. In this condition, there is an accumulation of cerebrospinal fluid in the fetal brain. The accumulated fluid puts physical pressure on the brain, the result of which can be mental retardation and problems with physical development. According to statistics, per 1000 children, 1 child is born with this pathology. You can count on the effectiveness of therapeutic methods only if they are used early.
The main sign indicating the presence of cerebral hydrocele is an overly large baby's head, and this disproportion is noticed after birth and during the subsequent nine-month period. The diagnosis is confirmed by performing brain scans, ultrasound, MRI and CT. The sooner treatment is started - in the first few months after the baby is born - the fewer complications await him in the future.
Therapy involves surgery, during which a shunt is performed to remove cerebrospinal fluid.
Causes
Hydrocephalus of the brain in the fetus is formed due to the negative impact of numerous factors.
More often, the main causes are infectious lesions in the body of the expectant mother.
A number of diseases are common causes of the formation of water in a child’s head:
- Sexually transmitted infections. These include chlamydia and syphilis. When an unborn child is infected, the central nervous system and brain are damaged.
- TORCH infections. Herpes, rubella, and toxoplasmosis are most dangerous during the 1st trimester, since in the early stages of pregnancy all organs and systems are formed. Violations are dangerous not only for the unborn child, but also for the woman.
- Congenital developmental anomalies. Chiari syndrome, artresia of the Magendie and Luschka fissures provoke damage to the baby’s internal organs and his brain.
Damage to the baby’s skull bones during childbirth poses a particular danger.
Fetal hydrocephalus can occur:
- as a result of maternal irradiation during the treatment of cancer tumors;
- prolonged stay in places with high levels of radiation.
The development of the disease is negatively affected by the presence of bad habits and prolonged use of medications.
Pregnancy and childbirth
After the diagnosis is confirmed, the woman is sent to the Center for Surveillance and Surveillance. Non-immune hydrops fetalis is a high-risk pathology that requires high-quality equipment and qualified specialists.
First of all, the compatibility of the diagnosed anomalies with life is determined. The woman must be explained what possible consequences for the child in the future. Non-immune hydrops can provoke serious abnormalities in the development of the fetus, which will cause a significant decrease in the quality of life. If it is not possible to find out the cause of the disease and it is impossible to prescribe effective treatment, then termination of pregnancy is recommended. If a decision is made to keep the child, additional examinations are carried out, the results of which help to decide what in this particular case would be more correct - premature delivery or prolongation of pregnancy. The choice is complicated by the fact that non-immune hydrocele is prone to spontaneous remission.
The decision to give birth is made based on the woman’s condition and the degree of maturity of the baby’s lungs. Before delivery, an ultrasound examination is performed to assess the presence of ascites and effusion. This will prepare you for possible aspiration of fluid. In most cases, a caesarean section is recommended, since with natural childbirth there is a risk of asphyxia.
Symptoms
Failures in development do not affect the mother’s well-being in any way.
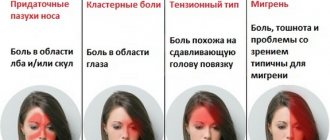
Pathology can be suspected only by increased activity and sudden freezing of the child. Signs of the onset of illness in a baby are:
- maternal drowsiness;
- her emotional stress;
- hypertension;
- headaches turning into migraines.
Hydrocephalus of the fetus during gestation is determined only by ultrasound diagnostics.
The main manifestation of the pathology is an overly large head of the child with a tendency to increase. This is very clearly visible on the monitor screen and photographs.
A situation is considered dangerous when the baby in utero suffers serious damage to the brain. They are caused by strong intracranial pressure.
During intrauterine development, many babies begin to suffer from seizures, cerebral palsy, and epileptic seizures.
Clinical manifestations of the disease in newborns are:
- anxiety, irritability, tearfulness, increased drowsiness;
- lack of appetite;
- increased muscle tone;
- the pupil is located close to the lower eyelid;
- vomiting, constant regurgitation;
- rapid decrease in body weight;
- convulsions.
With hydrocephalus, symptoms appear gradually. The disease is characterized by the occurrence of acute phases, respiratory failure occurs - a condition that threatens the baby’s life.
If a child has a seizure, immediate medical attention is required.
Consequences for mother and baby
The consequences for the mother are a complicated form of toxicosis in the last weeks of pregnancy.
A reduced level of protein in the blood is detected. Childbirth is difficult due to the abnormal position of the fetus, and this is caused by the increased size of its head.
If an increased accumulation of tansudate is detected in a child in utero, the mother is offered to terminate the pregnancy.
The highest mortality rate for children with this disease is the first 3 months after birth.
When a newborn develops water in the head and the prescribed treatment is ineffective, the following complications are observed:
- gray matter atrophy;
- the appearance of a “cleft lip”;
- Down syndrome;
- decreased level of concentration;
- development of autism;
- impaired coordination of movements;
- memory disorder;
- speech problems;
- visual impairment, up to the formation of blindness.
This causes problems with adaptation, communication, and subsequent education in kindergarten and school.
Life expectancy with hydrocephalus depends on early diagnosis and timely treatment.
Resuscitation in the postpartum period
Intensive care should begin in the delivery room and includes the following actions by neonatologists and resuscitators:
- it is necessary to prepare fresh frozen plasma and red blood cells in advance;
- due to possible swelling of the airways, it is necessary to have ETTs of all sizes in the delivery room, since the breathing method using a mask and bag is ineffective in this case;
- it is necessary to prepare drainages that may be needed to carry out various procedures and remove excess fluid;
- you need to be prepared for an urgent blood transfusion;
- calcium and glucose correction is required;
- a catheter is inserted into the child's umbilical artery;
- They are treated with antibiotics, and, if necessary, treatment for concomitant infectious diseases is performed.
Diagnostics
For accurate diagnosis and diagnosis, doctors use the ultrasound method.
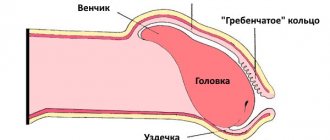
During an ultrasound of fetal hydrocephalus, the head of the unborn baby is measured in a transverse position. The main manifestations of pathology during scanning include the width of the lateral ventricles. Normally, this figure should be no more than 10 millimeters.
Diagnostic measures are carried out starting from the 17th week of gestation. Repeated scanning is carried out at 20-22 weeks. Often the disease is detected at 26 weeks.
Another informative way to diagnose edema in the fetus is echography.
Is it possible to cure the disease and treatment?
There are medications that can reduce the volume of accumulated transudate and reduce intracranial pressure.
Drug therapy is prescribed for compensated types of pathology. Effective medications for improving the condition of a baby with hydrocephalus are presented in the table.
| Name of the drug | Description | Mode of application |
| Diakarb | The product has diuretic properties, removes excess fluid from the body, and releases potassium. | Used to treat children from 4 months of age at a dose of 50 mg twice a day. |
| Furosemide | Powerful diuretic. Thanks to this property, it is possible to reduce intracranial pressure and normalize the general condition of the patient. | Prescribed from 1 to 3 mg. The dosage is calculated individually based on the body weight of the newborn. In the form of injections from 1 to 1.5 mg per kilogram of body. |
| Mannitol | Diuretic drug. The action of which is to increase the osmotic pressure in the renal tubules. | The product is available in powder form. Before use, it is dissolved in sterile water and administered intravenously |
The information provided in the table is for informational purposes only, so you should consult your doctor before using medications.
Surgical methods of treatment in children
Today it is practiced to use intrauterine treatment of hydrocephalus.
Thanks to a puncture of the anterior abdominal wall of the expectant mother's abdomen, doctors remove fluid from the peri-cerebral space. The procedure is done once. Another effective way to pump fluid out of a baby’s head before birth is bypass surgery. The entire system will remain inside the baby's head until the moment of birth.
Neuroendoscopic operations
A new effective, but at the same time expensive method of surgical treatment of internal hydrocephalus of the fetus. The duration of the operation is no more than 20 minutes.
A special medical device, a neuroendoscope with a built-in small camera, shows the place where the catheter is inserted. It is necessary to quickly remove accumulated cerebrospinal fluid. The doctor makes an additional hole to effectively remove transudate from the enlarged areas of the ventricles of the brain.
Bypass operations
The most effective way to treat true hydrops, but it is carried out only after birth. During the operation, shunts - silicone tubes - are inserted.
They drain excess fluid from the ventricles of the brain into the abdominal region. A special valve regulates the flow volume. The ICP stabilizes and the cerebrospinal fluid does not flow back into the brain cavity.
Several similar procedures are performed throughout the child's life. The tubes can become clogged and break, which leads to mechanical damage and disruption of their operation. Planned surgical interventions are prescribed due to age-related changes in the baby’s body.
Non-immune hydrops fetalis: main causes
- Santo S., Mansour S., Thilaganathan B. Prenatal diagnosis of non-immune hydrops fetalis: what do we tell the parents? Prenat. Diagn. 2011; 31(2):186–95. doi: 10.1002/pd.2677
- Mary EN, Suneet PC, Jodi SD Society for Maternal-Fetal Medicine (SMFM) Clinical Guideline#7:nonimmune hydrops fetalis. Am J Obstet Gynecol. 2015; 212(2):127-39. https://dx.doi.org/10.1016/j.ajog.2014.12.018
- Lee AJ, Bethune M., Hiscock RJ Placental thickness in the second trimester: a pilot study to determine the normal range. J. Ultrasound Med. 2012; 31: 213-8. DOI: 10.7863/jum.2012.31.2.213
- Im S.S., Rizos N., Joutsi P., et al. Nonimmunologic hydrops fetalis. Am J Obstet Gynecol. 1984; 5:566–9. DOI: 10.1016/0002-9378(84)90749-x
- Ota S., Sahara J., Mabuchi A., et al. Perinatal and one-year outcomes of non-immune hydrops fetalis by etiology and age at diagnosis. J. Obstet. Gynecol. Res. 2015; 42(4): 385–91. DOI: 10.1111/jog.12922
- Bockeria E.L., Bespalova E.D., Suratova O.G. Fetal organic tachyarrhythmias: treatment experience. Annals of Arrhythmology. 2011; 2:36–44.[Bokeria EL, Bespalova ED, Suratova OG Fetal organic tachyarrhythmias: treatment experience. Annals of arrhythmology. 2011; 2: 36–44. (in Russ.).
- Bespalova E.D., Bockeria E.L. Perinatal cardiac screening. Methodological recommendations for neonatologists, pediatricians, obstetricians-gynecologists, functional diagnostics doctors. Questions of practical pediatrics. 2010; 5 (1): 60-62.
- Kearney, H. M., et al., American College of Medical Genetics standards and guidelines for interpretation and reporting of postnatal constitutional copy number variants. Genet Med. 2011; 13(7): 680-5.
- Désilets V., De Bie I., Audibert F. No. 363-investigation and management of non-immune fetal hydrops. J. Obstet. Gynaecol. Can. 2018; 40(8): 1077-90. doi:10.1016/j.jogc.2017.12.011
- Bellini C., Donarini G., Paladini D. et al. Etiology of non-immune hydrops fetalis: An update. Am. J. Med. Genet. Part A. 2015; 167(5):1082–8. doi:10.1002/ajmg.a.36988.
- Hartge DR, Weichert J., Gembicki M., Krapp M. Confirmation of etiology in fetal hydrops by sonographic evaluation of fluid allocation patterns. Eur. J. Obstet. Gynecol. 2015; 195:128–32. doi: 10.1016/j.ejogrb.2015.09.006
- Laterre M., Bernard P., Vikkula M., Sznajer Y. Improved diagnosis in non-immune hydrops fetalis using a standardized algorithm. J. Obstet. Gynecol. 2017; 16(2):119–26. doi:10.1002/pd.5243
Received 04/16/2019
Accepted for publication 04/19/2019
Forecast
The prognosis depends on the volume of cerebrospinal fluid accumulation in the brain and the presence of associated abnormalities.
The consequences of hydrops fetalis will be insignificant if:
- the ventricles are slightly enlarged (up to 15 mm);
- no other defects were identified;
- timely treatment was carried out.
A newborn has a high chance of avoiding abnormalities and leading a normal life.
If the ventricular cavities are enlarged above 15 mm, the volume of cerebrospinal fluid increases rapidly. Multiple failures of internal organs are possible.
Treatment of pathology
In case of detection of congenital pathologies (including hydrops fetalis), incompatible with further life activity, detected in the first and second trimester, the woman is offered termination of pregnancy. In case of refusal, monitoring of the fetus continues in anticipation of the timing allowing the use of prenatal therapy. Treatment involves cordocentesis and blood transfusion through the umbilical cord, which can be repeated several weeks later if necessary.
In the presence of feto-fetal transfusion of twins, laser coagulation of the vessels that unite the embryos is prescribed. If it is impossible to carry out prenatal treatment, the degree of risk of premature labor is assessed in relation to antenatal death for the fetus, early permission from the fetus is prescribed, for which drugs are used that accelerate the maturation of its lungs. In certain cases, it may be necessary to administer cardiac glycosides to the parent to normalize the child’s cardiac activity.
After childbirth and resuscitation measures, including artificial ventilation and intubation of the child, the fluid accumulated in the pericardial sac is removed using a puncture. A pleural puncture and laparocentesis are provided.
Prevention
To reduce the risk of intrauterine hydrocephalus in your baby, you need to prepare for pregnancy. All chronic infections must be eliminated. At the same time, take a course of vitamins to strengthen the immune system.
It is necessary to eat right and engage in moderate physical activity. If possible, avoid large crowds of people during viral colds.
The formation of hydrocephalus in newborns in many cases is caused by infection of the mother during pregnancy, leading to disruption of the ventricular system of the brain. Timely detection of abnormalities and subsequent therapy provide a high chance for a child to live a full life.