Clouding of consciousness: first symptoms
Symptoms of a disorder such as clouding of consciousness may appear gradually over a long period of time or occur unexpectedly. The main symptoms of clouding of consciousness are:
- disorientation;
- hallucinations, as well as psychomotor hyperactivity;
- inability to think clearly;
- unexpected confusion or embarrassment;
- apathy and withdrawal (see also - what is apathy and how to get rid of it);
- memory deterioration or partial sudden loss;
- inability to distinguish between negative and good actions;
- inability to act independently and make simple decisions.
A person in a clouded state is not aware of his personality, as well as his social affiliation. Sometimes only one or more of the symptoms described above appear. Prolonged clouding of consciousness leads to dementia and loss of personal qualities.
Main symptoms preceding loss of consciousness
- Nausea rising in the throat.
- Dull and lingering ringing in the ears.
- Multi-colored specks in the eyes.
- Cold sweat all over the body.
- General feeling of great weakness.
- Severe pallor of the skin.
- Cardiopalmus.
- "Jumping" pulse.
- Decreased pressure.
- Pupil dilation.
As mentioned above, short-term loss of consciousness lasts from several seconds to several minutes, while prolonged fainting can last several hours. And this already has serious consequences and requires medical intervention.
Causes and diseases that cause sudden or chronic clouding of consciousness
Clouding of consciousness occurs for various reasons. For example, it appears temporarily after anesthesia along with severe dizziness and nausea or after a serious injury, carbon monoxide poisoning, after acute intoxication of the body (drug or alcohol), due to overwork, taking certain medications, hypoxia, prolonged insomnia (see also - how to deal with insomnia).
The cause of clouding of consciousness, partial or prolonged, may be the following diseases:
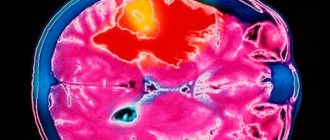
- brain tumors or concussions;
- schizophrenia;
- diabetes;
- sepsis;
- hypothyroidism;
- fever;
- heatstroke (first aid for heatstroke) or severe hypothermia;
- disruption of the heart;
- prolonged depression;
- epileptic seizures;
- severe dehydration of the body;
- senile dementia (dementia);
- Alzheimer's disease;
- renal failure;
- toxic shock syndrome;
- meningitis or encephalitis.
With these diseases or pathological conditions, clouding of consciousness occurs, which is only a symptom of the disease, and it already needs to be treated by a specialist.
How does loss of consciousness occur?
The person becomes ill, he rolls his eyes and loses consciousness, gradually sinking to the floor. It is very rare for a victim to fall as if knocked down. This will indicate the presence of other health problems. In any case, it is better to undergo a comprehensive examination, starting with a neurologist.
Fainting is not a sign of illness. For example, they are observed in completely healthy pregnant women when they see some food product. Therefore, everyone should understand how to behave if someone nearby faints. If you don’t know this and don’t understand the principles of correct behavior, then at the sight of a fainting state you can fall into a panic and, instead of helping, harm the person.
Who suffers from fainting?
So, most often, fainting is caused by a lack of oxygen supply to the brain. This process is sometimes called oxygen starvation. If we look at the statistics of fainting states in people of different groups, we will notice that it is impossible to single out a specific group based on any criterion.
The following are susceptible to fainting:
- men and women;
- people of all age categories.
Professional affiliation also does not determine the leading group in terms of fainting conditions. Sometimes people faint, for example, from fright or blood, as well as stuffiness or the sight of a spider. It is clear that these situations have nothing in common.
Main syndromes of clouded consciousness
Several syndromes of clouded consciousness have been identified - amentia, stupor, delirium, oneiroid, twilight stupor.
Stun
– a pathological condition characterized by the fact that a person seems to be in a dream, has difficulty answering standard and simple questions, gives unclear answers, becomes inactive, often silent and indifferent. But he does not exhibit hallucinations, as well as affective disorders or delusional states.
Oneiric obscuration
- dream-like, delusional-fantastic cloudiness. Fantastic dreams grow in a person’s head, which can be partially combined with the surrounding environment, then the patient can react to people nearby. A person with this type of clouding of consciousness usually has a frozen expression on his face; he may be silent, inactive, and practically motionless. The gaze alternates between amazement or delight, detachment or fear.
Delirium or delirious confusion
is distinguished by many psychological abnormalities. These can be fantastic illusions, vivid hallucinations, visual memories. A person in such a state can actively move, run somewhere, rush, defend. His facial expression is constantly changing.
The doctor can identify not only visual, but also auditory hallucinations, plus olfactory or tactile ones. Patients with delirium may have “lucid” periods of consciousness. Delirious delirium is manifested by muttering and uncoordinated monotonous actions. After this kind of clouding of consciousness disappears, a person may not remember it.
Twilight state of consciousness and its types
Stupefaction (twilight) occurs with hysteria, organic diseases of the central nervous system, epilepsy and traumatic brain injury. This type of disorder of consciousness is called transient, that is, it occurs unexpectedly and passes quickly.
Long-term stupefactions (up to several days) are possible mainly in epileptics. This condition may be accompanied by fear, anxiety, aggression and some other negative emotions.
Twilight disorder of consciousness is characterized by hallucinations and delusions. The visions are frightening. Expressed aggression is directed towards people, animals and inanimate objects. A person suffering from twilight darkness is characterized by amnesia. The patient does not remember what he said and did during his seizures, and does not remember the hallucinations he saw.
Twilight consciousness occurs in several variants:
- Outpatient automatism . This condition is not accompanied by delusions, hallucinations or aggressive behavior. Outwardly, the patient’s behavior is no different from his behavior in his normal state. A person automatically performs all usual actions. The patient may wander aimlessly along the street, following familiar routes.
- Brad . The patient's behavior does not always change. This state is characterized by silence and an absent gaze. The patient may show aggression.
- Oriented twilight stupefaction . The patient retains consciousness in fragments and is able to recognize close people. Delusions and hallucinations may be absent. The patient experiences fear or aggression.
- Hallucinations . The visions that visit the patient during an attack are threatening. Patients see red or blood. Visions may include fictional characters or fantastic creatures that show aggression. The patient begins to defend himself, causing harm even to those closest to him.
At the first signs of twilight conditions, a person must be provided with pre-medical assistance, care and observation. The patient should not be left alone. If consciousness is not completely lost, contact can be maintained with it.
Sometimes familiar faces become the only reference point for someone who has lost touch with reality. You should not wait until the patient completely loses contact with the outside world. He needs urgent transport to the hospital.
What to do if clouding of consciousness occurs
When clouded consciousness appears, it is necessary to identify its cause, which can be either psychological in nature or associated with a physiological disease. Since the person is in an altered state, it is necessary to call for medical help immediately.
In case of acute psychological changes in consciousness, it is important to take the patient to a psychiatric clinic, accompanied by a doctor or nurse. When aggression occurs, doctors use appropriate psychotropic medications.
Treatment methods
For whatever reason a person loses consciousness, the first thing to do is call a doctor. But while the ambulance is on the way, you need to provide first aid to the victim. You need to act quickly and not panic.
What should you do if a person suddenly faints?
- The victim should be laid on his side and his head tilted back slightly.
- If necessary, remove tight clothing and splash cold water on his face.
- In the room, open all the windows and try to bring ammonia to your nose.
- It is advisable to raise the patient's legs or sit him down with his head bowed low.
- If a person has regained consciousness, under no circumstances should you allow him to get up quickly.
If it occurs due to a sharp drop in blood pressure, which is the most common cause, then the victim’s legs can be wrapped in an elastic bandage - this will disperse stagnant blood in the vessels.
In any case, an accurate diagnosis can be made by a doctor who will conduct an examination and prescribe the necessary treatment. The specialists of our center will provide you with qualified assistance!
Diagnosis and proper treatment of clouding of consciousness
To effectively treat clouded consciousness, it is important to determine the causes of its occurrence. A comprehensive examination involves consultations with several specialists: a traumatologist, a neurologist, as well as a psychotherapist, therapist, and toxicologist. If the presence of non-psychological diseases is suspected, an MRI, biochemical blood test, and sometimes EEG, CT, ultrasound of internal organs, and studies of metabolic disorders are prescribed.
Once the main diagnosis has been established, comprehensive immediate treatment is carried out, including not only medications, but also psychological aspects that can prevent the occurrence of confusion.
With long-term clouding of consciousness, proper care for the patient is important, especially for the elderly. Such people cannot be left alone, unattended. Especially if disorientation manifests itself, they can simply get lost and get into trouble. A patient with senile dementia, as well as prolonged clouding of consciousness, should be in the most kind and warm atmosphere possible. It is advisable to hire a nurse for such a sick person.
To prevent the appearance of disorders of consciousness, proper nutrition, healthy sleep, and avoidance of alcohol are necessary. Diabetic patients need to constantly monitor glucose levels, train their memory, and always lead an active lifestyle.
Recommended Actions
If you see a person starting to lose consciousness, try to prevent him from falling and hitting his head.
It is necessary to ensure a sufficient volume of blood flowing to the brain. What instinctive reaction occurs when a person loses consciousness? Of course, I want to help him. And if he is lying down, there is a desire to put something under his head, but this is extremely contraindicated in the condition described. The fact is that when you raise your head, blood flows out of it. Thus, a person needs to be laid so that his head is at least at the level of his body, and maybe lower.
You can raise your legs, and then the flow of blood from the limbs to the head will begin. Many people advise leaving the unconscious person alone, letting him lie down, and he will come to his senses. However, if patting the cheeks does not help, it is best to call an ambulance without leaving things to chance. The victim may need immediate medical attention.
Causes of the condition
Clouding of consciousness occurs suddenly or gradually, can be long-term or short-term, momentary. Why does this condition occur? It can be caused by a number of reasons:
diseases;- injuries;
- taking medications;
- ecology, domestic reasons;
- toxic, drug addiction or alcoholism.
Narcotic, toxic, medicinal drugs and substances can cause extensive intoxication of the body, causing, in addition to symptoms of poisoning, also clouding of consciousness. This symptom is accompanied by delirium caused by delirium tremens. If we talk about diseases, then most often this phenomenon accompanies diseases such as dissociative, mental disorders, Korsakoff's syndrome, electrolyte imbalance, fever, liver failure, Wernicke's encephalopathy, etc.
Important! If you come to see a doctor about clouding of mind (even if temporary), then you cannot hide information about taking medications or substances, since laboratory tests will still reflect their presence in the body, but time for treatment may be lost.
Environmental and household factors mean the strongest influence on the human body of certain conditions - temperatures (heat stroke, hypothermia), substances (hypoxia - lack of oxygen, gradual intoxication with substances found in the environment - water, air, soil, etc.) .
What is noteworthy is that this symptom was observed in older people during hospitalization, that is, during a sharp change in living conditions. But clouding of mind occurs in a number of cases in ordinary situations - insufficient, poor nutrition, insomnia, fatigue. In these cases, when the lifestyle is normalized, the symptom also goes away.
There are a number of diseases in which clouding of consciousness is only part of the overall picture. Among them:
Dementia.- Shock.
- Hypothyroidism.
- Depression.
- Alzheimer's disease.
- Meningitis.
- Hypoglycemia.
- Oncological diseases in the head.
- Encephalitis.
- Schizophrenia.
- Renal/liver failure.
- Attack (heart attack, stroke, epilepsy, etc.).
- Head injuries, concussion.
Anxiety may also be accompanied by this symptom. In this case, the person will not necessarily be sick. But it is also possible to develop mental confusion after a stroke. Dehydration can also be a factor in the development of unhealthy conditions in a person. If changing living conditions does not solve the problem, then the problem lies in a disease or other pathology.
Head in a fog: causes and treatment of this condition
Fog in the head, heaviness, squeezing, tapping in the temples, clouding of consciousness... With such symptoms, people are increasingly turning to the doctor.
As medical practice shows, this condition has many causes. The most common are: astheno-neurotic syndrome, circulatory disorders in the brain and cervical osteochondrosis.
We will talk further about what fog in the head means and why it occurs.
Features of manifestation
Symptoms such as cloudiness, dizziness, heaviness, a feeling as if the head is in a fog, can accompany a person constantly or appear several times a week.
https://www.youtube.com/watch?v=fd7-57QvGuQ
This condition does not always mean that a person has any disease. Often these signs arise due to the influence of certain factors: changes in weather conditions, excessive physical exertion, lack of sleep, mental work, etc.
The main feature of the brain fog symptom is its sudden appearance. So, a person who felt good a minute ago, almost in an instant feels discomfort, fogginess, dizziness, blurred vision, dullness of consciousness.
The problem is that these symptoms can appear in the workplace or while performing an important task. Due to this, a person is deprived of the opportunity to carry out usual activities.
Brain fog is often accompanied by various symptoms:
- increased or decreased blood pressure;
- drowsiness during the day and sleep disturbance at night;
- weakness;
- headache;
- strong heartbeat;
- excessive sweating, etc.
Often this picture is accompanied by a feeling of unreasonable fear, a feeling of lack of air, and the appearance of a ringing in the head. There are many reasons for this condition.
Causes of the symptom
As stated earlier, the causes of brain fog may not always be due to health problems. Thus, when there are disruptions in the hormonal system, fog in the head is almost always observed. During pregnancy, a woman is often accompanied by this condition, as well as irritability and forgetfulness. The same symptoms may occur during menopause.
Other causes of brain fog:
Astheno-neurotic syndrome
If there is no clarity in your head, then most likely we are talking about astheno-neurotic syndrome. This pathology, in addition to brain fog, is accompanied by other symptoms:
- shallow sleep;
- problems falling asleep;
- irritability, suspiciousness, hot temper;
- unreasonable anxiety;
- rapid fatigue;
- drowsiness during the day;
- feeling of a lump in the throat;
- decreased ability to work;
- stiffness of movements;
- memory problems;
- pressing headaches;
- dizziness;
- tremor of the limbs.
The syndrome mainly affects people whose work involves mental activity and increased responsibility. In addition, pathology often affects those who have an unstable psyche.
The main causes of astheno-neurotic syndrome are prolonged stress, prolonged nervous tension, anxiety, chronic lack of sleep, and overwork. In addition, the pathology occurs in people with:
- chronic diseases;
- hypertension;
- vegetative-vascular dystonia;
- acute viral infections;
- poisoning;
- vitamin deficiency;
- bad habits;
- head injuries.
The syndrome develops gradually. At the initial stage of neurosis, a person feels weak in the morning, mild irritability, and anxiety.
Then, in the absence of medical assistance, other symptoms appear in the form of loss of strength, sleep disturbances, memory problems, a feeling of “vatness,” heaviness in the head, fog in the eyes, decreased ability to work, etc.
Then pain in the heart occurs, severe irritability gives way to weakness, appetite disappears, libido (sexual desire) and mood decrease, apathy appears, the patient constantly thinks about his health, and fear of death appears. Subsequent ignoring of these symptoms leads to mental disorders.
Vegetovascular dystonia
VSD is the most common cause of brain fog. Vegetative-vascular dystonia is not a separate disease, but a combination of many symptoms that arise against the background of disturbances in the functioning of the autonomic nervous system, which is responsible for the functioning of all internal organs and systems.
VSD is characterized by the following symptoms:
- fog, heaviness in the head;
- dizziness;
- headache;
- anxiety;
- unreasonable fears;
- nausea, stomach pain;
- tachycardia;
- lack of air;
- tremor of the limbs;
- unsteadiness when walking;
- sleep disorders - insomnia, shallow sleep;
- changes in blood pressure;
- irritability;
- “midges” before the eyes;
- ringing in the ears, etc.
The list of symptoms for VSD can be endless. The main feature of the disease is frequent relapses, manifested in the form of panic attacks.
If you do not take any action - do not take medications, do not strive for changes in lifestyle, do not seek help from doctors (psychotherapist, neurologist) - this can result in the appearance of various phobias and fears.
Insufficient oxygen supply to the brain
If the brain lacks oxygen, this leads to a feeling of brain fog. The process of hypoxia develops due to compression of the vessels through which the blood carries oxygen and all the substances necessary to nourish the organ.
At the same time, in addition to fogginess and “vatness” in the head, a person experiences:
- dizziness;
- weakness;
- severe heaviness in the head;
- decreased ability to work;
- memory problems;
- confusion of consciousness;
- problems with perception of information;
- inhibition of reactions;
- severe weakness, fatigue.
With severe oxygen starvation, a person may lose consciousness.
The causes of this condition may be:
- the presence of cervical osteochondrosis and other diseases of the spine;
- use of drugs and alcoholic beverages;
- hypertension, hypotension;
- previous traumatic brain injuries;
- smoking;
- lack of fresh air;
- limited physical activity;
- runny nose.
If this pathology is not treated, then oxygen-starved brain cells gradually lose their functionality, which ultimately leads to serious complications.
Osteochondrosis of the cervical spine
Fog in the head is the main symptom that accompanies cervical osteochondrosis. The disease is characterized by degenerative-dystrophic changes in the cervical vertebrae.
This process is almost always accompanied by compression of arteries and other vessels in the specified area. This leads to poor circulation and insufficient nutrition of brain cells.
In this regard, a person begins to feel all of the above symptoms, which are accompanied by:
- pain in the neck when bending or turning the head;
- severe heaviness in the head;
- pain in the shoulders, arms;
- a feeling of “dull pain in the head”;
- weakness in the neck;
- stiffness of movement in the shoulder joints.
Osteochondrosis of the cervical spine develops due to poor nutrition, lack of physical activity, and staying in the same position for a long time.
In advanced cases, the neck and shoulders can be completely immobilized.
Frequent consumption of gluten-containing foods
Not only diseases of the spine, neurosis and VSD can cause a feeling of fog, heaviness and “cottoniness” in the head, but also the consumption of foods containing gluten. An allergy to this component causes the production of substances that have a negative effect on the brain.
If people with a gluten allergy eat a lot of buns, bread, semolina, and pasta made with wheat flour, they will gradually develop the following symptoms:
- disruption of the gastrointestinal tract - bloating, constipation followed by diarrhea, pain in the stomach and intestines;
- weakness, fatigue, apathy, lethargy;
- brain fog;
- slow reaction;
- mental confusion;
- depression;
- psychological confusion;
- fog.
To find out if you really have a gluten allergy, you should see a doctor and take an allergy test.
Treatment
If the cloudy head appears due to lack of sleep, and the symptom is temporary, then just rest and get enough sleep. If this symptom occurs regularly, measures should be taken to avoid complications.
First of all, you need to see a doctor and find out the cause of the feeling of fog in your head.
If the source is astheno-neurotic syndrome, then it can be cured using psychotherapeutic methods. But first, you should exclude all provoking factors - stress, lack of sleep, excessive physical and mental stress.
If the influence of these factors is not reduced, then psychotherapy and drug treatment will not have the desired effect and will not eliminate unpleasant symptoms.
Medicines are used in severe cases. General restoratives, sleeping pills, antidepressants, antipsychotics and tranquilizers are considered effective.
If you have symptoms of VSD, you should consult a specialist. The therapist deals with this issue. To relieve symptoms, various medications are used - sedatives, sleeping pills, drugs for dizziness, to normalize blood pressure, etc. In addition to drug therapy, it is recommended to adjust your lifestyle:
- engage in light, non-competitive sports;
- learn to eat right;
- travel outside the city more often or simply go outside, taking long walks;
- eliminate stress factors;
- learn to go to bed and wake up at the same time;
- give up bad habits.
Physiotherapeutic procedures, acupuncture, and massage will help get rid of the fog in the head with VSD.
The symptoms of neurosis will be eliminated by drugs that normalize the activity of the autonomic nervous system, as well as drugs with a sedative effect.
In case of poor blood circulation in the brain, accompanied by fog in the head, medications with vasodilating and nootropic effects are prescribed. Pathology at the initial stage can be treated without drugs - with the help of massage and manual therapy.
Treatment of cervical osteochondrosis is aimed at relieving the inflammatory process and eliminating pain. For this purpose, NSAIDs, nerve blockade, and medications that normalize blood circulation are prescribed.
In addition to drug therapy, physiotherapy, physical therapy, massage, and manual therapy are recommended for people with cervical osteochondrosis.
Diagnostics
If fogginess in the head appears constantly, then this is a reason to urgently consult a doctor. Therapists, neurologists, and psychotherapists deal with this issue.
Before prescribing treatment, the doctor must interview the patient and find out what additional symptoms he has, as well as conduct a diagnosis. Here is a list of mandatory tests needed to find out why fuzzy head syndrome occurs:
- General analysis of urine and blood. Exclude the presence of inflammatory reactions and infectious processes.
- Ultrasound of blood vessels in the cervical spine.
- CT or MRI of the spine and brain. An MRI and CT scan will allow you to exclude malignant processes, determine the condition of blood vessels, identify the presence of chronic diseases of the nervous system, etc.
- Angiography of cerebral vessels.
The patient may also need to consult other specialists.
Symptoms
This condition has a number of its own symptoms. The symptoms are very extensive, but are confined to the head, i.e. brain, and therefore only a doctor can accurately determine clouding of consciousness. The following factors are identified that may arise in this case:
vagueness, vagueness, unclearness of thinking;- disorientation;
- inability to think quickly and clearly;
- confusion, embarrassment;
- memory impairment, partial or complete loss (amnesia);
- dizziness;
- convulsions;
- seizures;
- falling, loss of balance, coordination;
- disturbance in the linguistic system – disorientation of speech;
- fainting, loss of consciousness;
- sweating;
- muscle weakness, difficulty walking;
- mental personality change.
Impaired consciousness is divided into a number of stages, at which the severity of a particular pathology is determined:
- Confusion is expressed in unclear thinking. This worsens the patient’s condition and leads to a noticeable inhibition of decision-making processes. All pathological processes occur in the head, and there are no external, physical manifestations yet or they are insignificant. This is the beginning of the development of an imbalance of consciousness.
- Disorientation is expressed in the inability to understand one’s own relationship to things, places, people, and time. The first stage is disorientation in time, the second in place, and the third is a lack of understanding of one’s personality, when a person does not recognize himself.
Delirium is expressed in confusion and illogical thinking. People are often disoriented. The emotional background constantly changes from extreme to extreme, for example, from fear, anger to joy and happiness. All these conditions are constantly accompanied by a feeling of excitement and anxiety. The patient does not remember what happened a few minutes ago, where he was, and so on.- Lethargy is accompanied by drowsiness when a person is unable to respond to external stimuli, for example, sounds, temperatures, tactile sensations. These pathological processes are already becoming more noticeable, although they also occur in the patient’s head.
- With stupor, there is no reaction to almost all stimuli. The exception is pain.
- Coma is considered the last stage of impaired consciousness. With it, a person is not able to react even to pain.
Types of impaired consciousness
Impaired consciousness is divided into two groups: productive and unproductive. In the first case, the patient experiences hallucinations, deceptions of perception, imaginary objects and objects, which occurs in the case of mental painful conditions. Non-productive disorders of consciousness are the result of severe somatic illnesses, injuries or infections that affect the nervous system, so they are observed not only in psychiatry.
Non-productive disturbances of consciousness (blackout)
Stun
This condition is characterized by the fact that only intense stimuli cause a reaction in the patient (the threshold for responding to external stimuli increases). The patient understands the informational meaning of stimuli, but at the same time, orientation in time and environment is difficult, combined with psychomotor retardation. In addition, mental activity slows down. Verbal contact with the patient is difficult. The person responds with simple phrases, he is indifferent, drowsy, and takes a long time to react to any stimuli.
Light forms of stunning:
— Nubilization. Patients become fussy and excited. Clarity of consciousness fluctuates; a person can be involved in a situation for a short episode, and then absent again. Also characteristic is the lack of criticism of one’s own condition. This is well illustrated by the example of car accident victims who, in a state of shock, fussily help others, not noticing their own injuries.
— Domnolence is a form in which a person falls into a state of prolonged sleep, from which it is difficult to wake him up. When trying to wake the patient, aggression can be provoked. After a short awakening, instantaneous sleep occurs. Somnolence is observed in patients after recovery from an epileptic coma or a series of seizures.
Sopor
Stupor is a more serious condition than stupor. Consciousness is not completely turned off, but the patient does not understand the meaning of the addressed speech. Only elementary manifestations of mental activity are observed, only the most primitive reactions to stimuli are preserved. For example, when receiving an injection, the patient will make a grimace of pain, but will only respond to loud calls by turning his head. Muscle tone is reduced, reflexes are weak, pupillary reaction to light is slow.
Fainting
Fainting occurs when consciousness completely turns off and the patient does not respond to any stimuli (with ischemia - acute oxygen starvation of the cortex).
Coma
Coma is a serious condition characterized by complete suppression of mental activity. There is a deep degree of disturbance of consciousness - complete shutdown of consciousness and shutdown of reflexes (absence of pupillary and corneal reflexes). The muscles completely lose tone, there are no reflexes. The patient does not respond to external stimuli or any irritants.
Productive disturbances of consciousness or confusion
Delirium
This condition appears during intoxication (alcohol, atropine). Delirium can also be caused by infection (typhoid, influenza) or traumatic brain injury (TBI).
Delirium is characterized by loss of orientation in place and time while maintaining it in relation to oneself. Accompanied by bright, lively and moving visual hallucinations (less often auditory). Patients are full of fear, anxiety, fussy, restless.
The appearance of perceptual disturbances is characteristic. The patient experiences hallucinations and may also have illusions.
Hallucinations during delirium are most often visual and tactile, less often auditory. Often the patient sees animals (rats, small animals - zoohallucinations), demons, excessively large or small objects (more often - microhallucinations). Tactile hallucinations are also observed (for example, the presence of small creatures under the skin); the patient sees networks, cobwebs, and wires. A striking example is the thread symptom. A patient with delirium tremens may see an imaginary thread between the doctor's fingers. Different intoxications have their own specific symptoms. Thus, with cocaine delirium, Magnan’s symptom is observed, when the patient experiences tactile hallucinations in the form of the presence/sensation of small foreign bodies or insects under the skin, as well as crystals.
Sometimes images take on a scene-like character, like a movie.
In addition to distorted perception, thinking and memorization are impaired. A person expresses unstable delusional ideas and sees false images of people. After recovery from delirium, fragmentary, torn memories of past events are observed.
The orientation is specific. The patient is aware of his identity, but is lost in place and time. If we talk about emotional changes, then there is affective instability. Fear, overwhelming horror, surprise or sudden aggression, tearfulness dramatically change each other. Sometimes the patient displays a humorous attitude towards current events (“gallows laughter”). The behavior of a person suffering from delirium is also severely disturbed. He is fussy, restless, defending himself from something, running somewhere. There is motor agitation and the patient is difficult to control.
The intensity of delirious disorders increases in the evening and at night, and decreases during the day.
Oneiroid
Delusional, fantastic disturbance of consciousness, similar to a long dream.
Oneiroid is a condition that patients describe as a dream. This is an involuntary influx of pictures of fantastically delusional content, which have a completed plot and replace one another. The patient acts as a spectator. Dual orientation may occur when a person is in two places at the same time. This applies not only to place, but also to time.
Symptoms of oneiroid are polymorphic (varied). The patient can see himself in oneiric scenes, feels an involuntary flow of vivid thoughts and images. The experiences are scene-like in nature. It is noteworthy that the images and psychopathological disorders are within the same plot, that is, they are systematized and have a unique plot, in contrast to delirium.
Personal orientation is sharply disrupted. The patient is not aware of himself, he becomes a participant in events and influences the picture of the fictional world, which does not happen with delirium, where the person plays the role of an observer.
In the literature, two variants of oneiroid are distinguished: depressive (scenes of hell, torment, cataclysms are observed) and expansive (visions take on the character of long journeys, space flights, magical scenes). The patient feels himself in a different world, which may have different affective overtones depending on the oneiroid variants described above. Much more often in practice, expansive oneiroid is observed, in which ecstatic affect is typical, when the patient experiences a feeling of delight and happiness. After emerging from this state, patients sometimes want to return back to oneiric sensations.
Twilight stupefaction
This is a special condition that has an abrupt onset and sudden end. The name of this disorder is due to the fact that when it occurs, the circle of motives, ideas and thoughts narrows, which is reminiscent of a violation of seeing objects in the dark.
Elementary actions are observed, but the integrity of perception suffers. Consistent thinking and normal activities are not possible. Behavior is not determined by all external stimuli, but only by individually captured stimuli. The perception of objective reality is fragmentary, and the responses are distorted. Disorientation is further aggravated by the fact that selective phenomena are mixed with hallucinatory and even fantastic images. The patient’s external movements are often ordered, but not conscious; the patient’s actions are not predictable and therefore especially dangerous. Often during a twilight episode, people act extremely agitated and may do dangerous, antisocial things, become destructive, and self-harm. The personality is disoriented, and after emerging from twilight, complete or fragmentary amnesia is observed with a critical attitude, less often - the persistence of pathological experiences in consciousness for some time with delusional interpretation (residual delirium).
The twilight state is more often observed with epilepsy, sometimes with pathological intoxication and hysteria.
Amentia
Amentia is a disorder of consciousness in which the patient is extremely confused, disoriented in place, time, and self. Thinking is inconsistent, without logical connection, and movements are chaotic. Speech contact is virtually impossible; speech is devoid of grammatical structure. He resembles a person who is frightened, agitated in bed, cannot feed himself, and spits out food when feeding. At the same time, the emotional state is extremely labile, i.e. in a person, sadness turns into joy, passivity into aggression. Hallucinations are fragmentary, they quickly replace each other. The patient may fall into stupor or motor agitation.
Amentia is observed with head injury, severe intoxication, infectious lesions or schizophrenia.
Causes of confusion
The degree of confusion may vary. A person is not necessarily completely detached from reality; in mild cases, a short-term disorder of thinking and orientation is possible. Blackouts in one form or another can happen to anyone, and this does not always indicate brain disease or mental disorder.
Impaired consciousness occurs as a result of insufficiency of neurotransmitters in brain tissue. As a result, the neural conduction of brain impulses changes. There is a dysfunction of the autonomic and central nervous system.
The reasons may be:
- Severe emotional stress, shock (death of a loved one, divorce, shock from being at the scene of a disaster, accident with victims, etc.);
- traumatic brain injury;
- disruption of blood supply to the brain;
- brain hypoxia (oxygen starvation);
- infectious diseases of the brain (meningitis);
- severe dehydration of the body (including the brain);
- diseases that cause degeneration of brain structures (Alzheimer's disease);
- blood sugar levels are too low or too high;
- body temperature more than 40 degrees;
- bladder infections, especially in older people;
- exceeding the dose of medications that affect brain function (including sedatives);
- chronic alcoholism, drug addiction; recovery from binge drinking for alcoholics;
- intoxication.