Learn more about diseases starting with the letter “B”: Basilar impression, Basilar migraine, Beriberi, Bettolepsy, Amyotrophic lateral sclerosis, Alzheimer's disease, Wilson's disease, Hallerwarden-Spatz disease, Hamstorp disease, Hippel-Lindau disease, Canavan disease, Creutzfeldt disease -Jacoba, Lafora's disease, Machado-Joseph disease, Moya-moya disease, Morton's disease, Parkinson's disease, Pick's disease, Refsum's disease, Fahr's disease.
Description and causes of the disease
Bettolepsy is characterized as a disorder of consciousness that occurs as a result of severe coughing attacks. The degree of impairment has varying levels of severity, and can manifest itself as a slight fainting state, or a complete loss of the latter with accompanying signs of loss of control over one’s own body. According to medical statistics, the disease is extremely rare and occurs in patients suffering from primary heart and lung failure. The risk group includes men who have crossed the 45-year age threshold. Less commonly, pathology occurs in women. Of all observed states of altered consciousness, bettolepsy accounts for only 2%.
The cause of the abnormal manifestation is sudden or prolonged oxygen starvation of the brain structures, complicated by cough syndrome. Pathology develops against the background of the following main ailments:
Diseases of the respiratory system. With insufficient lung functionality, constant stagnation of the pulmonary circulation occurs, leading to the development of failure of the cardiovascular system and lungs. The severe stage leads to gradual dysfunction of areas of the cerebral cortex, which leads to such manifestations as systematic fainting with accompanying seizures.- Thrombosis of the respiratory canals as a result of foreign elements, infectious and inflammatory processes. With severe coughing attacks, further brain hypoxia occurs, which leads to fainting.
- Degeneration of brain tissue due to destruction of the vascular network, post-traumatic condition, etc.
- Pinching or compression of the peripheral nerves responsible for cardiac activity. Episodes of slow heart rate (bradycardia) lead to a sharp reduction in blood flow to the brain, which also leads to partial or complete loss of consciousness.
There are also external factors that contribute to the development of the disease:
- smoking;
- drug use;
- excess body weight;
- frequent consumption of alcoholic beverages.
The significance of cough syndrome as a provoking factor is that during attacks there is a sharp increase in internal pressure inside the sternum and peritoneal area, which leads to a decrease in blood flow to the heart. Cardiac output loses intensity, blood slowly enters the skull, which leads to fainting symptoms.
Doctors classify three degrees of pathology:
- Short-term disorder. Fainting lasts a few seconds, does not lead to critical consequences, does not require medical attention, and goes away on its own.
- Minor fainting at the peak of cough syndrome. Lasts on average up to ten seconds.
- Prolonged fainting. Symptoms such as severe cramps, defecation and urination often occur. Brain structures are severely damaged and permanent damage occurs, leading to subsequent cognitive impairment.
True causes and provoking factors
Hypoxia—oxygen starvation of tissues, in this particular case of the brain, is caused by any relatively long-term condition accompanied by:
- or a mechanical obstruction to breathing - the flow of oxygen;
- or caused by a lack of oxygen in the blood for another reason (defect of red blood cells in some anemias, for example).
In the variant of bettolepsy, these two factors in the development of hypoxia are combined. This is a mechanical obstruction of the airways damaged by acute or chronic pathology, and a prolonged period of circulation of oxygen-poor blood.
Time measured in minutes. Time that may be sufficient for the onset of irreversible changes in the brain.
Let us add to this basis what developed by the age of 40-50, but at an earlier age, coughing fainting does not develop - atherosclerotic degeneration of blood vessels, which in itself is the cause of chronic hypoxia. As well as associated episodes of excessive blood pressure. And also arrhythmia - momentary or permanent.
It is worth adding two more strokes to the canvas, adding the following to the causes of bettolepsy:
- endocrine pathology in the form of diabetes mellitus;
- chronic allergies to everything, which developed, among other things, as a result of excessive addiction to taking medications.
When there is excess glucose in the blood, as well as when aggressive substances appear in it, either released during an allergic reaction or necessary to extinguish it, the biochemical composition of the blood and its properties change in the same way as with mechanical suffocation due to respiratory tract pathology.
Anyone who has all these treasures of dubious value has an unusually high risk of developing cough epilepsy.
But... not everyone faints with a cough! And only 2% of adults experience various types of paroxysmal conditions! And children never suffer from this disease (with the exception of cases where whooping cough serves as a background).
Why?
For the development of cough fainting, one more condition is necessary - the presence of pathological impulses from reflexogenic zones:
- respiratory system;
- larynx (in particular, the areas of activity of the superior laryngeal nerve);
- carotid sinus, jugular veins, aorta;
- venous sinuses of the brain.
The reaction from the pressoreceptors located in these reflexogenic zones is a necessary link that closes the fatal chain - pathological impulses from them lead to an increase in the activity of the vagus nerve, contribute to the onset of bradycardia and the manifestation of a dangerous condition - Morgagni-Adams-Stokes syndrome.
The hand of fate, or who inevitably gets sick
Accordingly, the causes of the development of bettolepsy include conditions with phenomena of increased intrathoracic pressure, as well as cerebral hypoxia, leading to disorders in the activity of the nervous system. Other provoking disorders, diseases and conditions:
- diseases of the respiratory system in the form of bronchial asthma, chronic bronchitis with an asthmatic component and outcome in pulmonary emphysema, fibrous-cavernous form of pulmonary tuberculosis, laryngitis, whooping cough;
- status that occurs during aspiration of small objects into the larynx, trachea;
- neuralgia of the superior laryngeal nerve;
- pathology of the cerebral arteries and veins in the form of vascular anomalies, compression of the vertebral arteries by osteochondrosis or atherosclerotic deposits;
- household chronic poisoning – drug addiction and alcoholism.
Factors that provoke cough fainting should also include some habits and features of life in the form of:
- wearing tight-fitting clothing;
- habits of quickly changing posture (with sudden jumping up after prolonged sitting);
- "passive smoking";
- tendency to anxious and suspicious, “psychically suffocating” states.
Why you might lose consciousness:
Signs of a pathological condition
Symptoms often vary not only between different patients, but also within the same person during different seizures. There are many options for the course of an attack. Some symptoms are replaced by others, complement each other in different variations:
the starting point is a strong cough, sneezing, laughter, heavy physical activity that forces you to strain;- slight dizziness;
- noise in ears;
- swelling of the cervical and frontal veins;
- darkening of the eyes;
- numbness of the skin on the face.
The development of fainting is not associated with the previous position of the body; in any case, the patient falls. A person can come to his senses on his own; this does not require emergency medical care. The duration of the anomaly varies from a couple of seconds to five minutes. Accompanying signs are slight or intense cramps of the limbs, cyanosis of the epidermis, lips and peripheral parts of the body, and increased sweating is observed. In severe cases, urinary incontinence and uncontrolled bowel movements occur. If the brain structures have lesions, coughing fainting becomes the impetus for a subsequent epileptic seizure.
After the patient comes to his senses, there may be complaints of short-term loss of hearing, memory, headache, and weakness. After some time, the described symptoms disappear. If there are no aggravating disturbances during an attack, there is no need to worry about changes in mental functions.
Bettolepsy symptoms and treatment with folk remedies
08.04.2019
Bettolepsy is a neurological disorder. It is characterized by impaired consciousness during a severe coughing attack. Bettolepsy refers to cough syncope (syncope is a short-term loss of consciousness). Most often, the disorder occurs in men over 40 years of age.
Causes
Cough syncope occurs due to disorders of the internal organs:
- Pulmonary diseases: bronchial asthma, cor pulmonale, tuberculosis and emphysema. With pulmonary diseases, blood stagnates in the pulmonary circulation, which causes cardiopulmonary failure.
- Diseases and pathological conditions of the upper respiratory tract: whooping cough, foreign bodies entering the bronchi. During attacks, oxygen does not reach the lungs. Hypoxia of the brain occurs, the person loses consciousness.
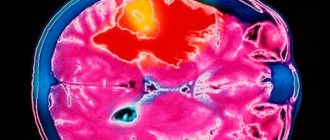
- Brain pathologies: dyscirculatory encephalopathy, arteriovenous malformations, previous traumatic brain injuries, increased intracranial pressure.
- Peripheral nervous system disorders. When the laryngeal nerve is inflamed, the vagus nerve is activated due to the generation of a large number of electrical impulses. The number of heart contractions decreases and cardiac output decreases. The brain receives less blood and the person loses consciousness.
These risk factors increase the likelihood of developing betolepsy:
- smoking;
- sedentary lifestyle;
- diet without vegetables and fruits;
- alcoholism, drug addiction.
The exact pathophysiological mechanisms are unknown. However, the hemodynamic theory has the most supporters. To understand the mechanism of development of cough syncope, you need to understand the mechanism of cough. It consists of three acts:
The first act is inspiratory. Characterized by closure of the larynx. The second act is compression: the muscles of the chest and abdomen contract, the diaphragm is fixed in a static position. The third act is expiratory: high pressure is created, which pushes air out at high speed with the larynx open.
In the second and third phases, intrathoracic pressure increases. With a normal cough, the pressure increases from 40 to 100 mm Hg. During syncopal cough, the pressure tends to 200-300 mm Hg. Due to such indicators, intra-abdominal pressure increases.
This results in decreased blood flow to the heart. As a result, the amount of blood ejected by the heart decreases and systolic blood pressure decreases. Blood flow to the brain decreases. In neurons – hypoxia and ischemia.
Due to lack of oxygen to the cortex, a person loses consciousness.
There are continuous and intermittent coughs. In the first option, a coughing attack occurs that lasts several seconds. Between acts of coughing, a person cannot inhale air. Because of this, the number of impulses to baroreceptors decreases, and the resistance of peripheral vessels reflexively increases.
With an intermittent cough, a person inhales air before each coughing act. This irritates the baroreceptors and decreases peripheral resistance.
These mechanisms lead to difficulty in venous outflow from the brain. Intracranial pressure increases. The minute volume of blood circulation in the cerebral arteries decreases. The bleeding may stop completely. Due to hypoxia, syncope occurs.
Symptoms
The clinical picture of bettolepsy is considered from 4 positions:
- The pathology is often observed in mature and elderly men who smoke and are obese. Often combined with bronchopulmonary diseases.
- Loss of consciousness is most often caused by chronic paroxysmal cough. Coughing is accompanied by strong contraction of the muscles of the chest and abdomen.
- Syncope can develop in any body position: lying, standing or sitting. Usually a person loses consciousness after 5 seconds of continuous coughing. Loss of consciousness is preceded by dizziness and decreased visual accuracy.
- Syncope due to continuous coughing lasts up to 10 seconds, in rare cases, loss of consciousness lasts 3 minutes. Syncope may be accompanied by cramps and heavy sweating. Some patients experience involuntary urination or defecation.
Diagnosis and treatment
To diagnose bettolepsy, it is usually enough for a doctor to study the history of life and illness, since the symptoms of syncopal cough are specific - they are difficult to confuse with signs of another disease. To clarify the diagnosis, doctors prescribe vagal tests, electroencephalography, and assessment of the functioning of the bronchi and lungs.
A person with an attack of bettolepsy needs first aid. A patient in syncope needs to ensure blood flow to the brain. To do this, lay the person on his back, raise his legs and lower his head. It is also recommended to open the window and relieve the upper body: unbutton your shirt, take off your tie.
To eliminate bettolepsy, you need to cure the underlying disease that causes attacks of suffocating cough. The patient also needs to quit smoking, lose excess weight and engage in physical activity.
Bettolepsy cannot be treated with folk remedies, since the underlying disease can progress and more often cause fainting.
Didn't find a suitable answer? Find a doctor and ask him a question!
Source: https://sortmozg.com/psihicheskie-rasstrojstva/bettolepsiya
How to identify the disease?
To determine the root cause of the disease being studied, a complete diagnostic examination is required, including measures such as:
Consultations with specialized doctors - therapist, cardiologist, neurologist. Specialists examine the history of the disease in detail, study the signs, consider the constitution of the body, age category, etc.- Vagal testing with pressure on the carotid sinus.
- Electrocardiogram of the heart. Designed to identify disorders in the cardiovascular system. In some cases, stress testing and a study of daily heart function are required.
- EEG. During the examination, abnormal impulses emanating from various areas of the brain are captured. If affected areas are present in the organ, this may be the cause of convulsive manifestations during the activity of the syndrome.
- Study of the state of functionality of the respiratory system. It is carried out using instrumental techniques - endoscopy, radiography, computer or magnetic resonance scanning. These methods make it possible to identify the presence of chronic diseases of the respiratory organs and the presence of foreign objects in the airways.
Cough until you lose consciousness what to do
A cough always causes a lot of discomfort and forces us to look for ways to eliminate it. A sore throat, weakness, chest or throat pain are not all the problems that are caused by this unpleasant symptom of many diseases.
But sometimes a cough can be accompanied by dangerous conditions such as confusion or fainting. This pathology is called “bettolepsy” (or cough-brain syndrome, cough fainting).
It has nothing to do with epilepsy, but can sometimes be accompanied by tonic seizures.
Cases of bettolepsy are quite rare and are observed in no more than 2% of patients with various types of paroxysmal conditions. More often, this syndrome is observed in older men suffering from chronic diseases of the respiratory system.
At a younger age, cough fainting is observed very rarely and is associated with insufficiency of the mechanisms responsible for maintaining postural tone, or increased sensitivity of the carotid sinus.
In children, bettolepsy can develop against the background of whooping cough.
In this article we will introduce you to the causes, symptoms and methods of diagnosing and treating this pathology. This information will be useful for you, and you will be able to consult a doctor in time if you suspect the onset of bettolepsy in yourself or your loved ones.
Bettolepsy is a disorder of consciousness that develops at the peak of an intense coughing attack and is sometimes accompanied by tonic convulsions.
It is more often observed with cor pulmonale or venous stasis and is associated with pathological impulses that arise in the superior laryngeal nerve, reflexogenic zones of the respiratory system, carotid sinus receptors, cerebral venous sinuses, jugular veins or the aorta.
As a result, the pathogenesis of cough-brain syndrome, accompanied by increased intrathoracic pressure and brain hypoxia, leads to disturbances in the functioning of the nervous system, which are expressed in short-term loss of consciousness, headaches, amnesia or convulsions.
The following factors can cause the development of bettolepsy:
- pathologies of the respiratory system: bronchial asthma, chronic bronchitis, emphysema, fibrous-cavernous form of pulmonary tuberculosis, laryngitis, whooping cough, etc.;
- aspiration of small objects into the trachea or larynx;
- neuralgia of the superior laryngeal nerve;
- pathological changes in cerebral vessels: vascular anomalies, compression of the vertebral arteries during osteochondrosis, atherosclerosis of the vertebral arteries, etc.;
- alcoholism.
The cause of the development of cough-brain syndrome and the initial condition of the patient largely determine the severity of symptoms, the course and outcome of bettolepsy. For example, with chronic cerebral circulatory failure due to hypertension or atherosclerosis, an attack of coughing syncope can cause structural damage to brain tissue and lasting consequences.
The clinical picture of bettolepsy is variable in severity not only in different patients, but also in one patient during different attacks.
Typically, an attack of coughing syncope is accompanied by the following symptoms:
- a coughing attack occurs while standing or sitting, while eating or immediately after eating;
- cough can be triggered by strong odors, cold air, excessive laughter, frequent sneezing, defecation, heavy lifting, or tobacco smoke;
- against the background of a cough, the patient’s face turns red and then turns blue, veins swell in the neck;
- sometimes a harbinger of an attack can be mild dizziness that occurs against a background of coughing;
- in the first minute of a cough attack, signs of fainting appear or loss of consciousness occurs, accompanied by a fall of the patient and cyanosis of the skin;
- after fainting, the skin becomes pale and the cough stops;
- the duration of fainting is several seconds or minutes;
- after this, the patient quickly returns to consciousness and recovers from the seizure (usually without medical assistance).
In some cases, an attack of coughing syncope is accompanied by convulsions, which are usually limited to one part of the body (for example, twitching in the limbs). Tongue biting is not observed during convulsions caused by bettolepsy. In rare cases, a seizure may lead to urinary or fecal incontinence.
During an episode of bettolepsy, the patient may sometimes experience the following symptoms:
- amnesia;
- headache;
- pain in the neck area.
Some experts identify the following variants of cough-brain syndrome:
- A seizure develops at the peak of coughing and is accompanied by sudden deep fainting and a fall of the patient.
- The seizure is accompanied by convulsions and, sometimes, involuntary bowel movements or urination.
- The seizures initially occur as in bettolepsy, and then are replaced by petit epileptic seizures, which can develop independently of the cough.
- Seizures of bettolepsy in patients with organic brain pathologies, accompanied by severe autonomic disorders.
- Seizures of bettolepsy in patients with a history of typical epilepsy.
Which doctor should I contact?
If a patient is concerned about episodes of loss of consciousness due to a cough attack or any other pathology, he should be examined by a neurologist. Additionally, a consultation and examination with a pulmonologist or cardiologist may be prescribed.
What is bettolepsy, how is it treated and what are its consequences?
Despite the opinion of many, bettolepsy (cough-brain syndrome, cough fainting) has nothing in common with epilepsy, it is worth paying attention to this part of the word: -lepsy translated from ancient Greek means “grasp” or “tightness”.
But doesn’t the brain have to fight, unclenching the tight embrace of hypoxia? A deadly embrace in a fight to the death where lives are at stake? And in both cases?
Therefore, before repeating what others have said, you should think at least twice.
Remedial measures
If an abnormal condition occurs, surrounding observers should help the patient by placing him in a natural position on his back. The lower limbs should be elevated, thereby allowing arterial blood to flow to the head. The airways should be cleared and the buttons on the neck should be undone. If possible, the air around should be fresh.
Medical manipulations are reduced to reducing blood stagnation in the brain. Correct treatment of cardiovascular diseases is carried out. Cardiotonics, drugs aimed at narrowing vascular channels, and substances that improve the patency of the bronchial passages are prescribed individually. In case of prolonged bradycardia (decreased heart rate), an atropic drug is used. In case of a complex course of the underlying disease, hospitalization is required for subsequent treatment.
What is the danger of bettolepsy: symptoms, treatment, complications
All people, without exception, cough. Some people get scared at the first cough and start taking antibiotics, while others, on the contrary, do not pay attention to the symptom for a long time.
But few of them know that a strong cough can lead to unpleasant consequences: from loss of consciousness to pathological changes in the brain. This type of attack is called bettolepsy.
Its manifestations should never be ignored; it is important to consult a doctor as soon as possible.
Why does an attack occur?
The origin of bettolepsy is related to:
- with incorrect impulses that come from the nerves to the cough center;
- with pathological perception of information in the reflex zones of the respiratory tract.
This leads to disturbances in the autonomic nervous system and excitation of the tenth pair of cranial nerves (vagus), causing severe bradycardia.
During intense coughing, hyperventilation of the lungs occurs and intrathoracic pressure increases. Because of this, cerebral circulation is disrupted and various disorders occur: short-term loss of consciousness, convulsions, amnesia, severe headache.
Read about the causes of sudden loss of consciousness and first aid for the victim.
How cerebral vasoconstriction manifests itself: symptoms and complications of severe vascular spasm.
There is only one provoking factor – cough. But there can be many risks:
- diseases of the lungs and bronchi - tuberculosis, asthma, emphysema, chronic bronchitis, whooping cough;
- foreign body entering the respiratory tract;
- inflammation of the laryngeal nerve;
- pathologies of cerebral vessels - atherosclerosis, compression of the arteries due to osteochondrosis;
- alcohol and tobacco abuse;
- diseases of the cardiovascular system - cor pulmonale, venous stagnation of blood;
- unhealthy diet, unhealthy lifestyle.
It is extremely important to know the cause of the development of bettolepsy, since the severity of the attack and treatment largely depend on this.
How does bettolepsy manifest?
The severity of bettolepsy symptoms may vary not only between different patients, but also within the same patient at different times. The disease attacks mainly older men; it can develop in children due to a cough, the cause of which is whooping cough. There are several variants of a cough-brain attack:
- The attack occurs at the peak of a strong cough. The patient loses consciousness and falls.
- Bettolepsy develops into epileptic seizures. They can already occur without a cough.
- Attacks that are accompanied by profound disturbances in the autonomic nervous system. Most often they occur in people with brain pathologies.
- Loss of consciousness is accompanied by convulsions, involuntary urination and defecation.
- History of seizures in patients with epilepsy.
Sometimes you can recognize the onset of bettolepsy and prevent the patient from falling:
- the face acquires a red and then bluish tint;
- lips become purple;
- the neck veins swell and pulsate greatly;
- the patient complains of dizziness.
Usually, loss of consciousness occurs before the end of the first minute of the attack, the patient stops coughing, falls and suddenly turns pale. If the patient does not have severe concomitant diseases, then consciousness resumes after a few minutes or even seconds. Most often, such patients do not require medical care.
After bettolepsy, memory disorders (amnesia), unpleasant, painful sensations in the neck, and headaches occur. Since an attack does not develop without an intense cough, it is important to know the factors that cause coughing:
- strong, prolonged laughter;
- inhalation of cold or hot air;
- sneeze;
- cigarette smoke or other irritating odors;
- smoking;
- lifting something heavy;
- the act of defecation during constipation.
How to diagnose the disease
If similar symptoms are detected, the patient should consult a family doctor or neurologist. To make a diagnosis, you need to carefully collect anamnesis, study the medical history and draw up the correct examination plan. It is important to differentiate bettolepsy from similar diseases, for example, epilepsy.
To determine brain-cough syndrome, the following examination methods are used:
- Holter monitoring – recording of a cardiogram during the day. Allows you to evaluate the work of the heart in the body’s usual conditions, as well as the reaction to various situations. Helps determine the cause of loss of consciousness.
- Tracheobronchoscopy is an endoscopic examination of the respiratory tract. The condition of the mucous membrane, the presence of foreign bodies, and the diameter of the bronchial lumens are determined.
- Valsalva maneuver - helps to assess the state of the autonomic nervous system. The patient should exhale all the air, then inhale deeply and exhale again, holding the breath for at least 15 seconds.
- ECG.
- ECHO-KG.
To make a diagnosis, hospitalization in an inpatient department is not always necessary. Most often, the patient comes for examinations. The exception is severe cough fainting with severe convulsions. In this case, the patient may be referred to a specialized epileptology center to clarify the disease.
How to treat bettolepsy
Treatment for bettolepsy, like most other diseases, is aimed at getting rid of the cause of the attacks. Therefore, it is prescribed individually after a thorough examination. After an attack, symptomatic therapy is carried out using:
- ammonia;
- cardiotonic drugs;
- saturating the body with oxygen;
- vasoconstrictor medications;
- for severe bradycardia - atropine.
Find out what apoplexy is: causes, symptoms, help, treatment.
Read why oxygen starvation of the brain leads to loss of consciousness. Diagnosis, treatment and consequences of hypoxia.
Everything about epileptic damage to the nervous system: causes, classification of epilepsy, symptoms.
Consequences of the disease
Bettolepsy is a fairly rare phenomenon. This diagnosis is made in approximately 2% of patients who present with similar complaints. Usually attacks do not lead to serious consequences. But this is not a reason to ignore the symptoms and not see a doctor. Since sometimes disturbances in the brain can occur, and with mild seizures, the patient can simply suffer from a fall.
The prognosis is generally favorable. Most often, it is enough to cure the provoking disease, and if this is not possible, then avoid severe coughing attacks. To do this, use antitussive drugs or, for example, breathing exercises.
(5 5,00 of 5) Loading...
Source: https://golmozg.ru/zabolevanie/bettolepsiya.html
Forecast and preventive recommendations
As an independent disease, bettolepsy does not pose a threat to the patient’s life. However, if its signs appear, you should immediately contact a medical specialist. The doctor will plan and carry out timely treatment of the underlying disease. It is important to monitor your body weight and eat right, as obesity is one of the risk factors.
At the first signs of the development of the disease, you must constantly monitor your condition, avoid a strong cough (it occurs not only with acute respiratory viral infections, but also with strong odors, changes in temperature, going out into the cold), rest on time, do not stand for a long time, and do not overexert yourself and do not make sudden head movements.
Etiopathogenesis
Bettolepsy manifests itself against the background of hypoxia of brain tissue, both acute and chronic. Its immediate cause is a sharp worsening of an existing oxygen deficiency, provoked by a cough attack.
This condition manifests itself in the following pathologies:
- Chronic lung diseases, which include emphysema, asthma, cor pulmonale, tuberculosis. With these diseases, congestion in the pulmonary circulation is observed, and pulmonary heart failure then progresses. In case of decompensation, encephalopathy with a tendency to bettolepsy is provoked.
- Obstruction of the airways as a result of aspiration of foreign bodies, whooping cough, acute laryngitis . The condition is accompanied by brain hypoxia and prolonged coughing attacks, causing respiratory attacks.
- Cerebrovascular disorders : vascular malformations, compression of extracranial and intracranial veins, consequences of traumatic brain injuries, pathologies of intra- and extracranial arteries. Because of this, venous hyperemia of the brain develops, which can be accompanied by cough syncope.
- Lesions of the peripheral parts of the nervous system . Neuralgia of the superior laryngeal nerve due to pathological impulses leads to activation of the center of the vagus nerve, which causes bradycardia. Cardiac output decreases, cerebral ischemia and fainting occur.
The list of risk factors that are important in the progression of attacks of bettolepsy should include excess body weight, smoking, alcohol abuse, and drug use.
All bad habits have a negative impact on the brain!
The pathogenesis of this condition is not thoroughly understood. Most often, paroxysms that occur at the height of a coughing attack have no common features with epilepsy. The mechanism of changes is most fully described by the hemodynamic theory.
There are three phases of cough: inspiratory, compressive, expiratory. In the second and third phases, there is a sharp increase in intrathoracic and intra-abdominal pressure, which reduces blood flow to the heart.
Because of this, cardiac output decreases and cerebrospinal fluid pressure in the spinal cord and brain changes. Due to a sharp increase in intrathoracic pressure, it increases in the peripheral vessels and chambers of the heart, which provokes venous stagnation, and then betolepsy develops.
Another mechanism for the development of the condition is also possible: as a result of stimulation of the vagus nerve receptors, pathological impulses are transmitted from the reflexogenic areas of the airways and jugular veins. Because of this, the functionality of the reticular formation changes, and this causes vasodepressor reactions, severe bradycardia and disturbances of consciousness.
Bettolepsy
Bettolepsy
is a transient disturbance of consciousness that occurs at the peak of a coughing attack. The syndrome is manifested by cough syncope: short-term twilight consciousness, fainting or deep loss of consciousness, sometimes accompanied by convulsions, involuntary urination and defecation.
Methods for diagnosing bettolepsy include questioning, examination of the patient, functional tests, instrumental studies (electrocardiography, electroencephalography, bronchoscopy).
Treatment involves symptomatic therapy that alleviates the patient’s condition and is aimed at eliminating the manifestations of the underlying disease.
The term “bettolepsy” was first proposed by the Soviet neurologist M.I. Kholodenko in 1941 for the interpretation of paroxysms that occur at the height of coughing attacks. The pathology is observed quite rarely, accounting for no more than 2% of cases of all types of paroxysmal conditions.
Bettolepsy can occur under the names “cough-brain syndrome”, “cough syncope”, “laryngeal vertigo”, “respiratory seizure”, “cough syncope”. It is more often observed in persons with symptoms of pulmonary heart failure.
Mostly men aged 45 years and older are affected.
Bettolepsy
The condition occurs against the background of acute or chronic hypoxia of brain tissue. Its immediate cause is a sharp worsening of an already existing lack of oxygen caused by coughing paroxysm. Pathology can manifest itself in the following diseases:
- Chronic pulmonary pathologies
(cor pulmonale, asthma, tuberculosis, emphysema). With these diseases, stagnation occurs in the pulmonary circulation, and pulmonary heart failure subsequently develops. In a decompensated course, the development of encephalopathy with a tendency to convulsive fainting is possible. - Airway obstruction
(aspiration of foreign bodies, whooping cough, acute laryngitis). Accompanied by acute cerebral hypoxia and prolonged bouts of severe coughing, which cause episodes of cough syncope. - Cerebrovascular disorders
. Changes in cerebral vessels (vascular malformations, compression of intracranial and extracranial veins, consequences of head injury) cause venous hyperemia of the brain, which can be accompanied by fainting attacks. Disturbances in the blood supply to the brain due to pathology of extra- and intracranial arteries (cerebral atherosclerosis, vertebral artery syndrome) threaten the development of a number of vestibular disorders, including loss of consciousness. - Lesions of peripheral nerves
. With neuralgia of the superior laryngeal nerve, pathological impulses lead to activation of the vagus nerve center and bradycardia. The volume of cardiac output sharply decreases, cerebral ischemia and fainting occur.
Risk factors for the development of attacks of impaired consciousness are smoking, drug addiction, and excess weight. When intoxicated with alcohol and drugs, changes occur in the brain, its membranes and cerebrospinal fluid, leading to disruption of the respiratory and cardiovascular systems.
The pathogenesis of bettolepsy is not fully understood. Typically, paroxysmal conditions that occur at the height of the cough reflex have nothing to do with epilepsy. The hemodynamic theory explains most fully the changes that occur during coughing. There are three phases of cough: inspiratory, compressive and expiratory.
In the compressive and expiratory phases, intrathoracic and intra-abdominal pressure increases sharply, resulting in a decrease in blood flow to the heart. This leads to a decrease in cardiac output and changes in cerebrospinal fluid pressure in the brain and spinal cord.
As a result of a sharp increase in intrathoracic pressure, it increases in the peripheral arteries, veins and chambers of the heart, which leads to venous stagnation and causes bettolepsy.
There are other development mechanisms: stimulation of vagus nerve receptors, transmission of pathological impulses from reflexogenic areas of the respiratory tract and jugular veins. This kind of influence leads to changes in the functioning of the reticular formation, which is fraught with vasodepressor reactions and severe bradycardia with impaired consciousness.
Bettolepsy syndrome has not been fully studied. Despite the high prevalence of diseases and conditions accompanied by cough, this symptom complex is rare. Its course can be grouped according to clinical manifestations:
- Brief twilight disorder of consciousness
. Usually lasts a few seconds and does not require emergency treatment. In this case, the underlying disease that caused the condition should be treated. - Brief fainting at the height of coughing
. Most often it lasts from 2 to 10 seconds. Treatment of the underlying pathology is necessary. - Prolonged loss of consciousness
. Complicated by convulsions, involuntary urination, defecation. Often combined with organic brain damage with lasting consequences. Aggravating factors include alcohol, nicotine intoxication, and drug poisoning.
Clinical manifestations may differ not only in different patients, but also each attack in an individual patient can take on different course options. Paroxysmal conditions - cough syncope - occur at the peak of the cough reflex.
Similar symptom complexes are also observed when laughing, sneezing, straining, lifting heavy objects, etc.
They may be preceded by prodromal phenomena (presyncopal states) in the form of dizziness, tinnitus, blurred vision, facial flushing, which is subsequently replaced by cyanosis, and swelling of the neck veins when coughing. In some cases, some warning signs may be missing.
Bettolepsy is accompanied by attacks of severe convulsive cough, at the height of which signs of impaired consciousness or fainting appear. Typically, the occurrence of an attack is not related to the position of the body.
A cough can be triggered by a strong smell or cold air. The duration of twilight consciousness or deep fainting ranges from a few seconds to 2-5 minutes.
At the peak of the cough, loss of consciousness is usually accompanied by a fall; most often, patients come to their senses without outside help.
Sometimes bettolepsy can be accompanied by convulsions that are local in nature: for example, twitching of the upper or lower extremities. The skin acquires a grayish-bluish tint, and profuse sweating appears.
Biting the tongue during an attack is usually not observed. In rare cases, bettolepsy leads to urinary and fecal incontinence.
With organic brain lesions, cough syncope can be replaced by petit epileptic seizures, which are not dependent on coughing.
In the post-syncope period, neck pain and headache may be felt. The patient complains of general weakness and dizziness, which disappear over time. The state of stupor and memory loss observed during epileptic attacks are not characteristic of bettolepsy. In the absence of aggravating factors, the consequences do not cause mental disorders.
Complications rarely occur with bettolepsy. They are usually associated with the underlying disease that caused the syndrome. One of the serious consequences is increasing pulmonary heart failure.
Circulatory disorders in the brain can lead to permanent damage to cerebral tissue - hypoxic encephalopathy.
During cough syncope, there is a risk of injury if you fall from your own height.
To make a correct diagnosis, a comprehensive clinical and instrumental examination is required to identify the cause of cough syncope, as well as differentiate it from other diseases. The diagnostic algorithm includes:
- Consultations with specialists
(therapist, neurologist, pulmonologist, cardiologist). At the appointment, the history of the disease, the nature of the attacks, and their connection with cough are studied. Great importance is attached to physical methods. During the examination, attention is paid to the general condition of the patient, constitutional features (tendency to obesity). - Vagal tests
(Valsalva maneuver, test with pressure on the carotid sinus). They are carried out with the aim of modeling the pathogenetic mechanisms of syncope. - EPI of the cardiovascular system.
An ECG allows you to identify pathological processes in the heart, indicating the presence of pulmonary heart failure. In some cases, stress tests and daily ECG monitoring are used. - EEG
. It makes it possible to record pathological impulses emanating from certain areas of the brain, which is extremely important for excluding organic cerebral lesions. Functional tests are used to identify foci of seizure activity. - Methods for assessing the bronchopulmonary system
(radiation diagnostics, endoscopy of the respiratory tract). X-ray of the lungs is used to identify chronic diseases of the respiratory system and pulmonary heart. With the help of tracheobronchoscopy, foreign bodies of the trachea and bronchi are detected and removed.
When carrying out differential diagnosis, loss of consciousness due to orthostatic hypotension, cerebral vascular occlusion, or epilepsy should be excluded. Episodes of loss of consciousness in these conditions are in no way related to the cough reflex.
During an attack, at the stage of pre-medical care for the patient, it is necessary to ensure the flow of arterial blood enriched with oxygen to the brain. For this purpose, it is necessary to lay the patient on his back, lower his head and raise his lower limbs, ensure free breathing and access to fresh air.
Medical care consists of measures aimed at reducing congestion in the brain, eliminating disturbances in the functioning of the cardiovascular system by administering cardiotonics, vasoconstrictors, as well as drugs that improve bronchial patency. For bradycardia, atropine is administered. Subsequently, the patient may be hospitalized in the department of neurology or pulmonology for treatment of the underlying disease.
To prevent paroxysmal conditions, it is necessary to monitor your health and, if symptoms of bettolepsy occur, promptly seek medical help. Diet is of great importance, since excess body weight is one of the risk factors.
It is necessary to avoid conditions that contribute to the development of fainting: prolonged cough, overwork, prolonged standing, severe tension, sudden movements of the head.
Good rest, gymnastics and sports, and hardening have a beneficial effect on the body.
Source: https://www.KrasotaiMedicina.ru/diseases/zabolevanija_neurology/betolepsy