Meningitis is a dangerous brain disease that leads to disability and, in the absence of medical care, death. Since cerebrospinal fluid changes its properties during meningitis, the doctor, after examining it, can make an accurate diagnosis and immediately prescribe the necessary treatment. Cerebrospinal fluid is taken using a lumbar puncture (puncture). There is no need to be afraid of this procedure, because it helps you choose the most effective treatment method.
What is cerebrospinal fluid
Cerebrospinal fluid controls the functionality of the nervous system. To obtain it, the doctor performs a lumbar puncture on the patient. Functions of cerebrospinal fluid:
- protect the brain from damage and exposure to mechanical factors;
- maintain optimal pressure inside the skull;
- promote metabolic processes between the brain and the fluid environment of the body;
- evacuate metabolic products;
- maintain the functioning of parts of the brain.
The total volume of spinal fluid ranges from 140 to 270 cubic meters. cm . It is formed by secretion by cells located in the vascular connections of the ventricles of the brain. Approximately 700 cubic meters are produced every day. see cerebrospinal fluid.
Normal indicators
Normally, cerebrospinal fluid has the following indicators:
- density - from 1.005 to 1.009;
- the pressure should be within 100-200 millimeters of water;
- there should be no coloring;
- cytosis (per 1 microliter): ventricular fluid - up to 1, cisternal fluid - up to 1, lumbar fluid - within 2-3);
- alkaline index - from 7.31 to 7.33;
- total protein - from 0.16 to 0.33 grams per liter;
- glucose indicator - from 2.8 to 3.9 mmol per liter;
- chlorine (ions) - 120-128 millimoles.
How to do a lumbar puncture
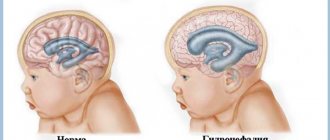
Meningitis is an absolute indication for lumbar puncture. This procedure is prohibited if:
- severe swelling of the brain tissue (the procedure can cause great harm);
- a sharp jump in cerebrospinal fluid pressure;
- the presence of a large formation inside the brain;
- dropsy.
Carrying out a puncture procedure for hydrocephalus and in the event of a pressure surge inside the skull can lead to a condition where a piece of brain tissue extends into the opening of the back of the head. At the same time, the work of the most important human life support centers is disrupted.
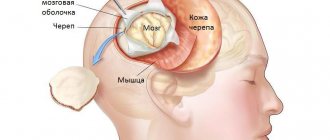
During the puncture, the person lies on his side, tilts his head to his chest and brings his legs bent at the knee joint to his stomach. This position ensures optimal accessibility at the puncture site. It is located between the 3rd and 4th vertebrae in the lower back. There is no longer a spinal cord in this place.
Alcohol is applied to the puncture site, and an anesthetic is injected under the skin. The skin is pierced with a special needle with a tip. If it is inserted correctly, cerebrospinal fluid begins to be released through the needle.
Symptoms of serous meningitis
After completing the incubation period, which lasts up to 20 days, severe symptoms begin:
- headache, aggravated by noise and bright light, which cannot be relieved with painkillers;
- double vision;
- dizziness;
- loss of consciousness;
- convulsions;
- swelling of the fontanelles in newborns;
- frequent vomiting and nausea;
- hypertension;
- with paralysis and paresis - difficulty or inability to breathe;
- critical temperature up to 40 degrees with sharp drops and rises, which is the most difficult for a child’s body;
- intoxication (arthralgia, weakness, myalgia).
In rare cases, there are symptoms of other diseases, which can make it difficult to diagnose a meningitis infection:
- typical signs of ARVI: cough with sputum, sore throat;
- symptoms of inflammation of the cranial nerves: drooping eyelids, strabismus, diplopia.
Characteristic signs and postures of pathological changes in the meninges:
- typical posture for stiffness of the muscles of the back of the neck - the patient lies on his side, head thrown back;
- Kernig's symptom - the tone of the lower leg muscles is increased, the patient cannot straighten the leg from a bent state;
- Brudzinski's symptoms (a group of symptoms that arise due to irritation of the meninges): upper: when trying to reach the chin to the chest, the legs involuntarily bend;
- lower: when trying to straighten one leg, the second bends even more, reaching to the stomach;
Features of analysis
Cerebrospinal fluid during meningitis is examined according to certain rules. The first drops of it do not fall into the test tube and are carefully removed because they contain an admixture of blood. The liquid must be in a sterile and chemically clean tube. It is collected in two vessels: one is sent for chemical and general clinical analysis, and the other for bacteriological.
All liquor samples are carefully protected from overheating and cooling. To determine bacterial bodies, they are additionally heated.
Liquid analysis is carried out in several stages:
- assessment of color, volume, measurement of relative density;
- counting cells in the sample (calculated per 1 ml);
- microscopic examination of the sample;
- cytological examination of the stained sample;
- biochemical analysis;
- microscopy.
Deviations from normal indicators - video
In the presence of brain diseases, the cerebrospinal fluid changes its characteristics:
- If pathogenic microorganisms are present in it, it turns greenish-gray. A large number of leukocytes are found in the fluid.
- The red color of the cerebrospinal fluid indicates the presence of red blood cells. It happens with intense inflammatory damage or after injury.
- With the development of inflammatory processes in the body, the cerebrospinal fluid becomes yellow and even brown, and hemoglobin decomposition products are found in it. This condition is called xanthochromia.
- False coloration of the cerebrospinal fluid is also possible. It occurs with prolonged use of certain medications.
- The green color of the liquor occurs with purulent inflammation of the lining of the brain.
- A cyst rupture turns it dark.
- When protein elements are cytosed, the cerebrospinal fluid becomes opalescent.
- The disease process in the meninges increases the density of the spinal fluid to 1.015.
- Increased amounts of fibrinogen promote the growth of fibrosis clots and films. Typically, such phenomena occur during the development of the tuberculosis process.
Sometimes enzymes are found in the liquor. Normally, it should contain few enzymes. An increase in the content of these substances may indicate a disruption in brain activity.
With meningitis, counting the number of microbial cells is of particular importance . This number is critical for determining an accurate diagnosis and selecting a treatment method. The following calculation methods are used:
- determination of the number of cells that are stained using the Romanovsky Giemsa or Nokhtu method);
- counting liquor elements using a Fuchs and Rosenthal chamber. In its absence, a Goryaev chamber is used.
The increase in cells in the cerebrospinal fluid during meningitis is called pleocytosis. It is often diagnosed during inflammatory diseases. This phenomenon is most pronounced in the tuberculous form of meningitis.
Staining with Samson's solution makes it possible to accurately differentiate microbial and other cells. With meningitis, the number of lymphocytes, neutrophils, monocytes, eosinophils, and basophils increases. The doctor is interested in the quantity of all these elements.
Slow leakage of cerebrospinal fluid, the impossibility of obtaining it, pronounced coloring, discrepancy between the patient’s serious condition and the composition of the fluid, pronounced coagulation of the cerebrospinal fluid indicates that the patient is developing blocked types of meningitis.
The presence of atypical cells in the fluid while maintaining its transparency and the absence of increased protein content does not confirm the diagnosis of meningitis. The patient is referred for additional studies, since this sign may indicate the progression of a malignant process in the brain.
Liquor in pathology
Pathological processes in the spinal cord and brain lead to changes in the physicochemical properties of the cerebrospinal fluid, as well as to changes in its cellular composition. These changes, as a rule, are characteristic of a number of diseases, which greatly facilitates the diagnosis of the patient and facilitates the choice of treatment tactics.
- Changes in color and transparency.
Cloudiness of the cerebrospinal fluid can occur with an increase in protein in its composition, the appearance of bacteria or fungi, or with an increase in the number of erythrocytes (> 400 * 10 6) and leukocytes (> 200 * 10 6). Red blood cells in the cerebrospinal fluid can appear in large numbers with subarachnoid hemorrhage, brain tumors and traumatic brain injuries. Infectious and inflammatory diseases of the brain occur with an increase in the content of leukocytes in the cerebrospinal fluid. Purulent meningitis causes clouding and a change in color (usually gray). Liqueur in serous meningitis may remain colorless or acquire a xanthochromic (yellowish) tint and flow out under high pressure.
A grayish-pink color of the liquid will appear when the number of erythrocytes is 0.6-1.0*109/l, pinkish-red when the number of erythrocytes is 2-50*109/l, when the number is 51-150*109/l - the color of fresh meat, and at >150*109/l - bloody.
- Cellular composition of cerebrospinal fluid in pathology.
When the total number of cells in the cerebrospinal fluid increases, the term “pleocytosis” is used, the causes of which are organic lesions of the central nervous system.
If the number of cells in the cerebrospinal fluid ranges from 6 * 106 / l to 70 * 106 / l, then in this case they speak of weak pleocytosis. Moderate pleocytosis - from 70 to 250 *106/l, pronounced - from 250 to 1000 *106/l, pronounced - more than 1000 *106/l.
Bacterial meningitis, meningoencephalitis, and multiple sclerosis occur with mild pleocytosis. Severe pleocytosis occurs in malignant brain tumors, as well as in stroke, especially in the first 24 hours. Hematomas and subarachnoid hemorrhages also occur with pronounced pleocytosis.
- Changes in the number of neutrophils and lymphocytes, as well as their ratio.
The reasons for the sharp increase in the number of lymphocytes are viral meningitis, tuberculous meningitis, parasitic diseases of the brain (echinococcosis, etc.), multiple sclerosis, subacute sclerosing panencephalitis, syphilitic meningoencephalitis and other diseases.
Changes in spinal fluid in purulent meningitis
The liquor in this case is heterogeneous. A feature of the disease process is that the number of pathologically altered cells and microorganisms in the cerebrospinal fluid rapidly increases. If the patient is suspected of developing purulent meningitis, then a general examination should be carried out no later than 60 minutes after the lumbar puncture.
The fluid in the spinal canal with purulent meningitis is usually opaque and green or milky in color. Laboratory studies confirm the growth of neutrophils, the spread of indicators of all formed elements.
If the number of neutrophils in the spinal fluid decreases significantly, this indicates that the outcome of the disease is favorable. Analysis of cerebrospinal fluid during meningitis helps determine the severity of the pathological process.
In the presence of purulent formations, the amount of protein increases, but with timely sanitation it begins to decrease. The combination of pleocytosis and elevated protein indicates an unfavorable prognosis for meningitis.
With the purulent variety of the disease, there is a decrease in glucose in the cerebrospinal fluid .
If its quantity increases, then this indicates regression of the disease.
Causes of serous meningitis
The origin of the disease, conditions and causes of occurrence are as follows:
- viruses (adenovirus , herpes , enterovirus , measles , polio , influenza).
- complications of infection (tuberculosis , syphilis).
- fungus (occurs in immunodeficiencies).
- previous pathological conditions of the central nervous system leading to the formation of serous effusion (tumors and cysts).
- infected domestic mice and rats (lymphocytic choriomeningitis).
Infection occurs through household contact (through wounds or using objects of the sick person), by airborne droplets (by sneezing or coughing), through water (swimming pool).
Characteristics of spinal canal fluid in tuberculous meningitis
Laboratory tests for microorganisms for the tuberculous type of meningitis do not show positive results. A more thorough study of the cerebrospinal fluid helps to detect the presence of a pathogen in it.
Precipitation can be noticed no earlier than 12 hours after analysis. The sediment looks like a fibrin network in the form of a web or flakes. A large number of Mycobacterium tuberculosis can be found in it.
During the tuberculous process, the cerebrospinal fluid remains transparent, without noticeable coloring. Cytosis occurs in a fairly wide range and differs depending on the stage of meningitis. In the absence of etiotropic treatment, the number of cells always increases. Repeated cerebrospinal fluid sampling after the start of therapy notes a decrease in the number of cells.
A characteristic feature of the development of pathology is the presence of lymphocytes in the cerebrospinal fluid. If the level of monocytes and macrophages in it increases, this is a bad sign. Neutrophils and giant lymphocytes can be found in large quantities in the cerebrospinal fluid. Protein in this pathology usually increases; its level can reach 3 grams per liter.
The glucose level in the cerebrospinal fluid with tuberculous meningitis sharply decreases to 0.8 mmol. Sometimes the chloride level also decreases. A favorable indicator is an increase in the level of these cerebrospinal fluid indicators.
Spinal canal fluid in meningococcal meningitis
Bacterial examination of the cerebrospinal fluid is mandatory to establish the type of pathogen. If the analysis was carried out on the first day after hospitalization, then in almost all cases pathological microorganisms are detected. On the 3rd day of disease development, the number of microbes decreases significantly.
Changes in cerebrospinal fluid go through several stages:
- increased level of intracranial pressure;
- development of neutrophilic type of cytosis;
- the appearance of changes indicating the development of a purulent type of meningitis.
If meningitis is not treated or is not treated correctly, bacteria are found in the patient’s cerebrospinal fluid. The amount of protein and neutrophils increases. The more protein, the more severe the disease.
In the pneumococcal form of meningitis, the fluid is cloudy, purulent, and sometimes turns green. The number of neutrophils is moderate. Proteins can be up to 10 grams per liter or even more.
Treatment of serous meningitis
Therapy is carried out in a hospital setting. Quarantine must be observed; contact with the sick person must be done only after wearing a mask. In case of illness, the following is prescribed:
- antiviral drugs ( Interferon, Acyclovir );
- antimicrobial agents. Sowing takes a long time, which the patient does not have, so a wide range of products are used. Penicillin drugs are used ;
- agents that restore the microflora of the gastrointestinal tract;
- antimycotics for fungal etiology. Fungal disease is caused by immunodeficiency, relapse is possible;
- drugs against tuberculosis;
- to boost immunity, immunoglobulins are prescribed intravenously;
- anti-inflammatory drugs;
- Dehydration medications are used to combat high blood pressure. They reduce hypertension by removing fluid. Diuretics ( Lasix ) are administered;
- antipyretics at high temperatures;
- to stop seizures, sedatives are prescribed, which are not addictive and are mildly tolerated by children;
- nootropics for the protection of nerve cells;
- intravenous vitamins (namely B vitamins);
- cerebral cortex polypeptides are administered after completion of therapy and are repeated every six months.
If aseptic meningitis is detected due to medication, all medications should be immediately discontinued and symptomatic therapy should be carried out.
It is necessary to create the following conditions for a comfortable stay of the child in the hospital:
- dim light, preferably thick curtains;
- there should be no sharp sounds;
- lack of stress (when crying, the child’s nervous system is in a state of tension, his health deteriorates sharply);
- a diet with no sweets, fatty foods, salty foods, or hot foods.
Features of cerebrospinal fluid in serous inflammation
In serous meningitis, the cerebrospinal fluid is usually clear with the presence of a small number of lymphocytes. At the initial stage of the disease, some accumulation of neutrophils is observed. This indicates a complicated course of the disease and usually indicates a poor prognosis for meningitis .
Most often, protein levels fluctuate within normal limits. Among some patients, the amount of this substance in the cerebrospinal fluid decreases slightly, which is caused by an increase in the production of cerebrospinal fluid. Pleocytosis is increased only in the case of meningitis caused by the Coxsackie virus. With herpes, on the contrary, it is almost absent.
During the recovery stage, the patient exhibits lymphocytosis. In mild cases, it is noted already on the third day of illness. With serous meningitis caused by the mumps virus, the cerebrospinal fluid is usually clear and without color. It reveals the presence of lymphocytes, and the level of chloride ions and glucose increases slightly.
Examination of the spinal fluid during meningitis is mandatory: this is the only way to determine whether a patient has inflammation of the meninges and choose the most appropriate therapy. You should not be afraid of damage to the spinal cord, since there is no spinal cord at all at the puncture site. After receiving the biological material, the laboratory assistant immediately studies it. This must be done as quickly as possible, because some forms of meningitis progress quickly, and every second is valuable for the patient’s recovery.
Viral and bacterial meningitis
MGMSU named after N.A. Semashko Meningitis is a group of diseases characterized by damage to the meninges and inflammatory changes in the cerebrospinal fluid.
Normal number of cells in cerebrospinal fluid (CSF)
is no more than 5 in 1 µl [1, 2], the amount of protein is no more than 0.45 mg/l, sugar is no less than 2.2 mg/l. Cells in normal cerebrospinal fluid are represented by lymphocytes.
According to the composition of the formed elements in the cerebrospinal fluid and etiology, meningitis is divided into purulent
(bacterial) with a predominance of neutrophilic leukocytes and
serous
(usually viral) with predominantly lymphocytic pleocytosis.
Some bacterial meningitis is characterized by a predominance of the lymphocytic (serous) composition of the cerebrospinal fluid (tuberculosis, syphilitic, Lyme borreliosis, etc.). Meningitis can be primary
or
secondary
(develops against the background of an existing general or local infectious process);
according to the nature of the course - acute
,
chronic
, sometimes fulminant.
In pathogenesis
Meningitis is played by a complex of factors: first of all, the properties of the pathogen, the reaction of the host organism and the background against which the contact of the micro- and macroorganism occurs. The virulence of the pathogen, its neurotropism and other features are of great importance. In the host’s reaction, a significant role is played by age, nutrition, social factors, previous injuries and diseases, the nature of previous treatment, immune status, etc. Environmental conditions include exposure to physical factors of cooling, overheating, insolation; contacts with animals, vectors and sources of infection, etc.
Certain individuals have an increased risk of developing infections of the nervous system. These include people with certain concomitant diseases and chronic infections, such as skull injuries, consequences of neurosurgical interventions and shunting of the cerebrospinal fluid system, chronic purulent processes in the chest cavity, septic endocarditis, lymphoma, blood diseases, diabetes, chronic diseases of the paranasal sinuses, alcoholism, long-term therapy with immunosuppressants, etc. The high-risk group also includes patients with congenital and acquired immune defects, pregnant women, patients with unrecognized diabetes, etc. In such individuals, due to a defect in immune defense, there is an increased risk of viral infections that they have already encountered in early childhood. This primarily includes diseases caused by the herpes group: cytomegalovirus, Epstein-Barr virus, varicella-zoster virus.
The pathogen can penetrate into the meninges in various ways: hematogenous, lymphogenous, perineural or contact (in the presence of a purulent focus in direct contact with the meninges - otitis media, sinusitis, brain abscess).
Overproduction of CSF, disruption of intracranial hemodynamics, and the direct toxic effect of the pathogen on the brain substance are essential in the pathogenesis of meningitis. The permeability of the blood-brain barrier increases, the endothelium of the brain capillaries is damaged, microcirculation is disrupted, and metabolic disorders develop, aggravating brain hypoxia. As a result, cerebral edema occurs, the progression of which can lead to brain dislocation and death from respiratory and cardiac arrest [3].
Viral meningitis
The etiological classification of viral meningitis most fully meets epidemiological and practical requirements. Most authors consider enteroviral meningitis to be one of the most common types of viral meningitis [4, 5]. The genus of enteroviruses (family Picornaviridae) includes poliovirus types 1–3, Coxsackie viruses A (types 1–24) and B (types 1–6), ECHO viruses (types 1–34), enteroviruses 68 -71st types. All representatives of enteroviruses cause meningitis, but most often the Coxsackie and ECHO viruses. Often the causes of viral meningitis are also paramyxoviruses (mumps, parainfluenza, respiratory syncytial), viruses of the herpes family (herpes simplex type 2, varicella-zoster, Epstein-Barr, herpes virus type 6), arboviruses (tick-borne encephalitis) , lymphocytic choriomeningitis, etc.
Clinic
Meningitis, including viral ones, is characterized by an acute onset with high fever, headache, nausea and vomiting, general malaise and weakness
. Typical for meningitis is the presence of meningeal symptoms, indicating irritation of the meninges. The meningeal symptom complex includes, in addition to headache, stiff neck, Kernig and Brudzinski symptoms, photophobia, and hyperesthesia of the skin. In young children, bulging and tension of the fontanel, tympanitis when tapping the skull, and a symptom of “suspension” (Lessage) are observed.
For some types of pathogens, a blurred clinical picture is observed with low-grade fever and moderate headache, absence of vomiting, meningeal monosymptoms or reduced symptoms.
General cerebral symptoms
in the form of impaired consciousness, convulsions and
signs of focal damage
to the nervous system
during meningitis are absent,
and their presence indicates encephalitis, but some authors admit their short-term presence at the onset of the disease as a manifestation of cerebral edema.
The main criterion for meningitis is an increase in the number of cells in the CSF. In viral meningitis, a lymphocytic composition of the CSF is observed.
Cytosis is represented by a two to three-digit number, usually no more than 1000 in 1 μl. The percentage of lymphocytes is 60–70% of the total number of cells in the cerebrospinal fluid. Protein and sugar levels are within normal limits. In the presence of meningeal signs, but in the absence of inflammatory changes in the cerebrospinal fluid, they speak of meningism. In some meningitis, signs of a general viral infection are observed (Table 1).
The duration of viral meningitis is 2–3 weeks. In 70% of cases the disease ends in recovery
[6], but in 10% the course is longer and may be accompanied by complications.
Features depending on the pathogen
Although in most cases of viral meningitis there is no clear clinical correlation with a specific pathogen, some features may be observed. So, often Coxsackie viruses of group B
cause diseases that occur with severe
myalgic syndrome
(the so-called epidemic pleurodynia or Bornholm's disease);
Diarrhea may occur. Both groups of Coxsackieviruses can cause pericarditis and myocarditis
.
Adenoviral meningitis
accompanied by an inflammatory reaction from the upper respiratory tract,
conjunctivitis and keratoconjunctivitis
.
Parotitis
often occurs
with damage to the parotid glands
, abdominal pain and increased levels of amylase and diastase (pancreatitis), orchitis and oophoritis. At the onset of the disease, the composition of the CSF may be neutrophilic with low sugar levels. Often the disease becomes protracted with a delay in the sanitation of the cerebrospinal fluid.
Lymphocytic choriomeningitis can also have a protracted course.
, and meningitis caused by
herpes simplex virus type 2
. With these types of disease, at the onset of the disease, the sugar level in the CSF may be below normal, which forces them to be differentiated from tuberculous meningitis.
Herpetic meningitis
often observed against the background of a primary genital infection - in 36% of women and 13% of men. In most patients, herpetic rashes precede the signs of meningitis an average of a week. Herpetic meningitis can cause complications in the form of sensory disturbances, radicular pain, etc. Relapses of the disease are described in 18–30% of cases [7].
Meningitis with herpes zoster
in some cases it occurs with minimal meningeal syndrome or asymptomatically. As a rule, it is not a monosyndromic lesion of the nervous system, but develops against the background of concomitant radicular phenomena, sensory disturbances, etc.
Meningitis with tick-borne encephalitis
observed in almost half of the sick. The onset is acute, accompanied by high fever, intoxication, pain in muscles and joints. Characterized by hyperemia of the face and upper body, severe headache, and repeated vomiting. In 20–40% of cases, a two-wave fever with a period of apyrexia of 2–6 days is observed. In the cerebrospinal fluid in the first days of the disease, neutrophilic leukocytes may predominate, the preponderance of which may persist for several days. Inflammatory changes in the CSF last a relatively long time - from 3 weeks to several months, accompanied by poor health. At the same time, diffuse neurological symptoms may be observed. Asthenic syndrome after illness, characteristic of tick-borne encephalitis, is observed in approximately 40% of those who have recovered from the disease and lasts from 1–3 months to 1 year. In 2–6%, a transition to a progressive form of the disease may subsequently occur.
Diagnosis
The diagnosis of viral meningitis is difficult, especially in cases of sporadic disease. For some viral meningitis, a history or associated organ involvement may be helpful (Table 1). But the main attention is paid to laboratory diagnostics: isolating the virus from the CSF and determining the 4-fold increase in specific antibodies in the dynamics of the disease
.
Currently, large treatment centers use polymerase chain reaction
(PCR), which has high sensitivity and specificity.
Treatment of the vast majority of viral meningitis is symptomatic
.
In the acute period detoxification therapy
: solutions of glucose, Ringer, dextrans, polyvinyl lyrrolidone, etc. Moderate dehydration is used: acetazolamide, furosemide). Symptomatic drugs (analgesics, vitamins A, C, E, group B, antiplatelet agents, etc.).
For meningitis caused by herpes simplex virus type 2, intravenous acyclovir
10–15 mg per 1 kg per day for 10 days, based on 3-fold administration.
Bacterial meningitis
The causative agents can be meningococci, pneumococci, Haemophilus influenzae, staphylococci, salmonella, listeria, tubercle bacilli, spirochetes, etc. The inflammatory process that develops in the meninges is usually purulent. In recent years, the etiological structure of purulent bacterial meningitis (PBM) has changed significantly. In adults, in more than 30% of cases, the causative agent is Streptococcus pneumoniae, in people over 50 years old - S.pneumoniae and gram-negative bacteria of the intestinal group (E.coli, Klebsiella pneumoniae, etc.), in children under 5 years of age in more than 30% of GBM is caused by Haemophilus influenzae type B [2, 8]. However, according to the forecast of epidemiologists, another increase in the incidence of meningococcal infection is expected in a few years.
Clinically, GBM is characterized by a more acute onset of the disease, more severe intoxication and high fever, compared to viral meningitis, and a more severe course
. CSF in GBM is turbid, with high neutrophilic pleocytosis, increased protein content; sugar levels are reduced.
Meningococcal meningitis
Meningococcal meningitis occurs mainly in children and young people. In almost half of the patients it is preceded by nasopharyngitis, which is often mistakenly diagnosed as ARVI. Against this background or in the midst of complete health, meningitis begins acutely - with chills, an increase in body temperature to 39–39.50 C, and a headache, the intensity of which increases with every hour. On the very first day, vomiting, photophobia, hyperacusis, skin hyperesthesia, and meningeal symptoms appear. There is a revival or suppression of tendon reflexes and their asymmetry. A little later, signs of increasing cerebral edema may appear: attacks of psychomotor agitation, followed by drowsiness, then coma. Focal symptoms are also possible: diplopia, ptosis, anisokaria, strabismus, etc. When often combined with meningococcemia, a characteristic hemorrhagic rash appears on the skin, the appearance of which usually precedes the symptoms of meningitis.
Possible atypical forms
, especially in patients receiving antibacterial drugs. The course of meningitis in these cases is subacute, the body temperature is subfebrile or normal, the headache is moderate, there is no vomiting, meningeal symptoms appear late and are mild, but encephalitis, ventriculitis subsequently develops and death can occur.
In infants
The onset of meningitis, including meningococcal, is manifested by general anxiety, crying, screaming, refusal to suck, sudden agitation from the slightest touch, and convulsions.
In the first hours of meningitis, the CSF is either not changed at all, or the inflammatory changes are mild. From the end of the 1st day, the CSF becomes typical for purulent meningitis. Microscopy of smears of cerebrospinal fluid sediment in most cases reveals gram-negative diplococci, mainly intracellularly. Timely initiation of adequate therapy ensures recovery in most cases.
; in the absence of this, mortality reaches 50%.
Pneumococcal meningitis
Pneumococcal meningitis can be either primary or secondary (in this case it is preceded by otitis media or mastoiditis, pneumonia, sinusitis, traumatic brain injury, cerebrospinal fluid fistulas, etc.). It often occurs in persons with a burdened premorbid background: alcoholism, diabetes mellitus, splenectomy, hypogammaglobulinemia, etc.
The onset can be either rapid (25%) or gradual, over 2–7 days. Meningeal symptoms are detected later than with meningococcal meningitis, and in very severe cases they are completely absent. Most patients experience convulsions and impaired consciousness already in the first days of the disease. The clinical course is characterized by exceptional severity due to the involvement of brain matter in the pathological process. The encephalitis that develops as a result is manifested by focal symptoms in the form of paresis and paralysis of the limbs, ptosis, oculomotor disorders, etc. In cases where meningitis is one of the manifestations of pneumococcal sepsis, a petechial rash is observed on the skin, similar to that of meningococcemia.
The CSF is very turbid, greenish, the number of cells ranges from 100 to 10,000 or more in 1 μl, and cases with low cytosis are especially severe. The protein level increases to 3–6 g/l and higher, the sugar content decreases. When smear microscopy, gram-positive diplococci located extracellularly can be detected.
The prognosis for pneumococcal meningitis is worse than for meningococcal meningitis: even with early therapy, due to the rapid consolidation of pus, the process progresses and mortality reaches 15–25%.
Meningitis caused by Haemophilus influenzae type B
Meningitis caused by Haemophilus influenzae type B most often affects children under 1.5 years of age,
but it can also occur in older children, in adults after 65 years of age, and sometimes in young and middle-aged people. According to some data [9], in recent years, up to 95% of all cases of GBM are caused by pneumococcus and Haemophilus influenzae type B (Hib).
The symptoms of Hib meningitis depend on the age of the patient and the duration of the disease. The onset can be sudden, with a sharp increase in body temperature to 39–400 C, repeated vomiting, and severe headache. After a few hours, convulsions, impaired consciousness, coma occur, and death may occur. A gradual development of the disease is also possible, with symptoms associated with the primary focus of Hib infection first appearing (epiglottitis, cellulitis, purulent otitis, arthritis, etc.), and then meningeal, cerebral and focal symptoms are added. The CSF is cloudy and green in color. There is a characteristic discrepancy between turbidity of the cerebrospinal fluid (it is caused by a high concentration of the pathogen in the CSF) and relatively low cytosis. Meningitis can occur sluggishly, in waves, with alternating periods of improvement and deterioration. Untimely and/or inadequate antibiotic therapy leads to death, the frequency of which reaches 33% [5].
Purulent meningitis of other etiologies (staphylo- and streptococcal, klebsiella, salmonella, caused by Pseudomonas aeruginosa, etc.) are usually secondary (oto- and rhinogenic, septic, after neurosurgical operations) and are relatively rare.
Diagnosis
The acute onset of the disease, a combination of fever, intoxication, meningeal syndrome, and characteristic changes in the CSF (high neutrophilic pleocytosis, increased protein content and decreased glucose levels) give grounds to diagnose purulent meningitis.
The etiology of GMB can be tentatively established by bacterioscopy of a CSF smear and clarified using bacteriological examination of CSF and blood. However, in patients who have already received antibiotics, the likelihood of detecting the pathogen using these methods is low. Therefore, various immunological methods are used to detect pathogen antigens and antibodies to them (VIEF, latex agglutination). The etiology of meningitis is most accurately determined using PCR [10]. Differential diagnosis for both purulent and serous meningitis is carried out between meningitis of various etiologies, as well as with other diseases accompanied by meningeal syndrome and neurological disorders: cerebral and subarachnoid hemorrhage, brain injuries, brain abscess and other volumetric processes, cerebrovasculitis, infectious diseases with meningeal syndrome, etc.
Treatment
For GBM, unlike viral ones, antibacterial therapy
which is urgent.
At the first stage, before the etiology of
GBM is established, one of the following antibiotics is recommended: ampicillin/oxacillin (200–300 mg/kg per day); ceftriaxone (100 mg/kg/day) or cefotaxime (150–200 mgkg); in young children, a combination of ampicillin with ceftriaxone [2, 11]. In the future, antibacterial therapy is adjusted depending on the etiology of meningitis and the sensitivity of the pathogen. Antimicrobial drugs must be prescribed in maximum doses that provide bactericidal concentrations in the CSF [12]. In patients with secondary GBM, sanitation of the primary lesion is necessary.
Tuberculous meningitis
Tuberculous meningitis most often affects children and the elderly
. The disease in most cases is secondary in nature, spreading from primary foci in the internal organs (lungs, lymph nodes, kidneys). It is also possible to damage the membranes from subependymal caseous foci that existed for a long time without manifestations. Provoking factors are immunodeficiency states, alcoholism, exhaustion, drug addiction.
In the membranes of the base of the brain, dense infiltrates form with compression of the cranial nerves and vessels of the circle of Willis. The disease develops gradually, weakness, adynamia, sweating, increased fatigue, and emotional lability appear. A headache occurs, increasing in intensity, low-grade fever, and vomiting. Damage to the oculomotor nerves appears early.
In the CSF – lymphocytic pleocytosis, protein-cell dissociation, hypoglycorrhachia. The diagnosis is based on the determination of antigen and antibodies to Mycobacterium tuberculosis in the CSF using enzyme-linked immunosorbent assay (ELISA) and the use of PCR.
The treatment uses isoniazid (5 mg/kg/day) in combination with rifampicin (10 mg/kg/day) and pyrazinamide (15–30 mg/kg/day). Duration of treatment is 9–12 months.
Meningitis with syphilis
Meningitis in syphilis is observed in all stages of clinical manifestations of the disease and in asymptomatic cases. It may have a manifest or blurred clinical picture. From 10 to 70% of people with early syphilis have lymphocytic pleocytosis in the CSF, which is often combined with an increase in protein. In diagnosis, taking into account the polymorphic clinical picture, the main role is given to laboratory tests: a complex of serological reactions with cardiolipin and treponemal antigens in serum and CSF; microhemagglutination reactions of Treponema pallidum [13]. Treatment is carried out with penicillin (2–4 million units intravenously every 4 hours) or 2.4 million units/day intramuscularly with probenecid (500 mg orally 4 times/day). The course of treatment is 10–14 days.
Meningitis due to Lyme borreliosis
Meningitis in Lyme borreliosis is a common complication of the disease. It may occur in combination with erythema migrans
– a characteristic marker of the disease.
The disease is usually preceded by ticks biting when visiting the forest. The course of meningitis is polymorphic, meningeal signs can be moderately expressed. In the CSF there is lymphocytic pleocytosis. Serological tests play a decisive role in the diagnosis: immunofluorescence reaction or ELISA with the B.burgdorferi
. Treatment is carried out with intravenous penicillin 24 million units/day for 14–21 days or ceftriaxone 1 g 2 times a day.
Specific prevention
Specific prevention of bacterial meningitis. Currently, there are vaccines to prevent meningococcal meningitis, Haemophilus influenzae and pneumococcal infections. Vaccination is carried out in high-risk groups, as well as for epidemiological reasons.
The list of references can be found on the website https://www.rmj.ru
References
1. Menkes JH Textbook of Child neurology, 4ed. Lea & Feiberg, London. 1990; 16–8.
2. Roos KL Meningitis. 100 maxims in neurology. Arnold, London, 1996.
3. Pokrovsky V.I., Favorova L.A., Kostyukova N.N. Meningococcal infection. M., Medicine, 1976.
4. Lobzin V.S. Meningitis and arachnoiditis. L., Medicine, 1983.
5. Acute neuroinfections in children. Ed. A.P. Zinchenko. L., Medicine, 1986.
6. Sagar S., McGir D. Infectious diseases. Neurology. Ed. M. Samuels. M., 1997; 193–275.
7. Dekonenko E.P., Lobov M.A., Idrisova Zh.R. Damages of the nervous system caused by herpes viruses. Neurological Journal. 1999; 4:46–52.
8. Demina A.A. Epidemiological surveillance of meningococcal infection and purulent bacterial meningitis. Epidemiology and Infectious Diseases 1999; 2: pp.25–8.
9. Sorokina M.N., Skrinchenko N.V., Ivanova K.B. and others. Meningitis caused by Haemophilus influenzae type B: diagnosis, clinical picture and treatment. Epidemiology and infectious diseases. 1998; 6:37–40.
10. Platonov A.E., Shipulin G.A., Koroleva I.S., Shipulina O.Yu. Prospects for diagnosing bacterial meningitis. Journal of Microbiology. 1999; 2; 71–6.
11. Guidelines for the clinic, diagnosis and treatment of meningococcal infection. Appendix to the order of the Ministry of Health of the Russian Federation, 1998.
12. Padeyskaya E.N. Antimicrobial drugs for the treatment of purulent bacterial meningitis. RMJ, 1998; 6 (22): 1416–26.
13. Marra CM Neurosyphilis. Current Therapy in Neurologic Disease, ed. R. T. Johnson, J. W. Griffin. Mosby, 1997; 136–40.
| Applications to the article |