Fevarin is an antidepressant, one of the representatives of the SSRI group. Like any psychotropic drug, it is not recommended to take fevarin without consulting a doctor and to voluntarily discontinue the drug if it has been prescribed. Abruptly stopping the drug may lead to withdrawal syndrome.
Pharmacological properties of the drug Fevarin
Pharmacodynamics. Receptor binding studies have shown that fluvoxamine is a potent serotonin reuptake inhibitor both in vitro and in vivo and has minimal affinity for serotonin receptor subtypes. The drug has little ability to bind to α-adrenergic, β-adrenergic, histaminergic, muscarinic, cholinergic or dopaminergic receptors. Pharmacokinetics. Fluvoxamine is completely absorbed after oral administration. The maximum concentration in blood plasma is achieved 3–8 hours after taking the drug. The average absolute bioavailability is 53% (due to the first pass effect through the liver). Concomitant food intake does not affect the pharmacokinetics of fluvoxamine. In vitro, 80% of fluvoxamine is bound to plasma proteins. The volume of distribution in humans is 25 l/kg. Fluvoxamine is extensively metabolized in the liver. Although in vitro the main isoenzyme involved in the metabolism of fluvoxamine is CYP 2D6, its plasma concentration in individuals with reduced CYP 2D6 activity is not much higher than in individuals with extensive metabolism. The average half-life from the blood plasma is 13–15 hours after a single dose and increases slightly (17–22 hours) with multiple doses, while the equilibrium concentration of the drug in the blood plasma is achieved within 10–14 days. Fluvoxamine is extensively transformed in the liver, mainly through oxidative demethylation, resulting in at least 9 metabolites that are excreted by the kidneys. 2 main metabolites have little pharmacological activity. The remaining metabolites are pharmacologically inactive. Fluvoxamine is a potent inhibitor of CYP1A2 and moderately inhibits CYP3A4 and has only limited inhibitory effects on CYP2D6. Fluvoxamine exhibits linear pharmacokinetics when administered as a single dose. The equilibrium concentration in blood plasma is higher than that with a single dose of the drug and is disproportionately higher when taken in higher daily doses. The pharmacokinetics of fluvoxamine are identical in healthy adult volunteers, the elderly and in patients with renal failure. The metabolism of fluvoxamine is impaired in patients with liver disease. Steady-state concentrations of fluvoxamine in blood plasma are twice as high in children aged 6 to 11 years as in children aged 12–17 years. The concentration of the drug in the blood plasma in children aged 12 to 17 years is the same as in adults.
Contraindications
Contraindications for taking Fevarin include the following groups of people with the following pathologies:
- Hypersensitivity to the active and excipients.
- Concomitant use of MAO inhibitors and tizanidine.
- The drug is contraindicated for people with alcohol dependence.
- Not prescribed for children under 18 years of age. An exception is obsessive-compulsive disorder in children over 8 years of age.
- Not prescribed to people with severe pathologies of the liver and kidneys.
- Not recommended for patients with epilepsy.
Use of the drug Fevarin
The tablets are taken orally, without chewing and with water. Depression (adults) The recommended initial dose of the drug is 50 or 100 mg 1 time per day. It should be taken once a day, before bed. The dose should be increased gradually until a clinical effect is achieved. The effective dose of fluvoxamine is usually 100 mg/day. The maximum daily dose is 300 mg/day. If the drug is prescribed at a dose exceeding 150 mg/day, it is divided into several doses throughout the day. In accordance with WHO recommendations, after the patient’s symptoms of depression disappear, treatment should be continued for at least another 6 months. The recommended dose of the drug to prevent relapse of depression is 100 mg of fluvoxamine once a day. Obsessive-compulsive disorders (adults and children aged 8 years and older) The recommended starting dose is 50 mg/day for 3–4 days, after which it should be gradually increased until the maximum effective dose is reached, which is usually 100–300 mg/day. days The maximum daily dose of Fevarin in adults is 300 mg, and in children over 8 years of age and adolescents - 200 mg. Fluvoxamine in a dose of up to 150 mg is prescribed once a day, preferably at night. If the drug is prescribed in a dose exceeding 150 mg, it should be divided into 2-3 doses during the day. Once the therapeutic effect is achieved, treatment can be continued at an individually selected dose. If after 10 weeks of treatment there is no improvement, the advisability of further use of Fevarin should be reconsidered. Although systematic studies have not been conducted on how long treatment with the drug can last for obsessive-compulsive disorders, taking into account their chronic nature, it is recommended to continue treatment after 10 weeks of continuous use of the drug, provided that a positive therapeutic effect is achieved. Dose selection must be very careful to keep the patient on the lowest effective dose. The advisability of continuing treatment should be reviewed periodically. Some clinicians recommend the combined prescription of behavioral psychotherapy for patients who achieved a positive effect during treatment with Fevarin. Patients with hepatic or renal insufficiency should begin treatment with a low dose and be under close medical supervision. The tablets should be swallowed whole with water.
Scheme for correct withdrawal of fevarin
In order to prevent the development of fevarin withdrawal syndrome, it is necessary to strictly adhere to a specific discontinuation regimen. Its main principle is a gradual reduction in dosage until complete withdrawal of the drug. This allows the cells of the central nervous system to relearn how to function without an additional stimulant, which is fevarin.
First of all, it is worth remembering that after achieving remission in the treatment of any mental illness, it is necessary to continue taking the drug for preventive purposes. To do this, the dose of fevarin is reduced by 50 mg per week until a dosage of 100 mg per day is reached and thus taken for about six months. After this, you can think about stopping the drug.
Stopping taking fevarin does not last long - one to two weeks. The dose is again reduced by 50 mg, taken for a week or two weeks, after which the drug is completely abandoned. If the above-mentioned complaints occur when discontinuing this regimen, you should consult a doctor.
Side effects of the drug Fevarin
Nausea and vomiting are the most common symptoms associated with treatment with Fevarin. The severity of this side effect decreases significantly during the first two weeks of treatment. Other adverse events observed during clinical trials at the frequencies listed below were often disease-related and not necessarily related to treatment. Often (frequency 1–10%) Metabolic and nutritional disorders: anorexia. From the central nervous system: agitation, anxiety, dizziness, headache, insomnia, nervousness, drowsiness, tremor. From the cardiovascular system: palpitations/tachycardia. From the gastrointestinal tract: abdominal pain, constipation, diarrhea, dry mouth, dyspepsia. From the skin and subcutaneous tissues: increased sweating. General disorders and reactions at the injection site: asthenia, feeling of malaise. Uncommon (frequency ≤ 1%) Mental disorders: confusion, hallucinations. From the central nervous system: ataxia, extrapyramidal symptoms. From the cardiovascular system: (postural) hypotension. From the skin and subcutaneous tissues: rash, itching, angioedema. From the musculoskeletal system: arthralgia, myalgia. From the reproductive system: disturbance (delay) of ejaculation. Rarely (frequency ≤ 0.1%) Mental disorders: manic states. From the side of the central nervous system: convulsions. From the hepatobiliary system: impaired liver function. From the skin and subcutaneous tissues: photosensitivity. From the reproductive system and mammary glands: galactorrhea. Other side effects that were observed during use of the drug. Cases of weight gain or loss have been recorded, as well as serotonin syndrome, phenomena similar to neuroleptic malignant syndrome, hyponatremia and syndrome of impaired antidiuretic hormone secretion (see also section “Peculiarities of use”). After discontinuation of treatment with Fevarin, a withdrawal reaction may occur, although preclinical and clinical data do not indicate that this treatment is addictive. In connection with drug withdrawal, the following symptoms were observed: dizziness, paresthesia, headache, nausea and anxiety. They usually disappear on their own. Before stopping treatment, it is advisable to consider the need to gradually reduce the dose of the drug. Hemorrhagic manifestations: ecchymosis, purpura, gastrointestinal bleeding (see also section “Peculiarities of use”). Paresthesia, anorgasmia and changes in taste sensations occurred very rarely. In each frequency group, undesirable effects are arranged according to the degree of reduction in their severity.
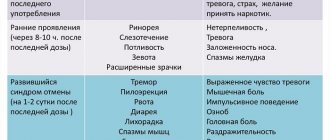
Antidepressant withdrawal syndrome: symptoms
Antidepressants have an effect on the emotional sphere of a person, as a result of which his behavior changes. Withdrawal syndrome appears in patients after abrupt cessation of taking medications of this group; its main manifestations are associated with anxiety disorder or depression. If a patient experiences antidepressant withdrawal syndrome, the symptoms and duration are determined by the characteristics of the drug and the individual characteristics of the body.
Symptoms of antidepressant withdrawal syndrome:
- attacks of headache;
- panic attacks;
- emotional instability;
- impaired coordination, spatial orientation and dizziness;
- nightmares and insomnia;
- fever;
- nausea and lack of appetite.
Fluoxetine, the withdrawal syndrome of which is the least pronounced, reduces feelings of fear, tension and anxiety. Other antidepressants differ in the intensity of symptoms upon drug withdrawal. Psychiatrists at the Yusupov Hospital are familiar with theoretical material and regularly study the scientific research of world experts, therefore they prescribe effective methods for treating the withdrawal syndrome of various antidepressants to patients.
Special instructions for the use of the drug Fevarin
In patients with depression and obsessive-compulsive disorder, there is a constant tendency to commit suicide, which may persist throughout the entire period of treatment until significant remission is achieved. Careful monitoring of this category of patients is necessary. In patients with impaired renal or liver function, treatment should begin with low doses of the drug and under close medical supervision. Occasionally, treatment with Fevarin was accompanied by an increase in the activity of liver enzymes and corresponding clinical symptoms. In such cases, treatment with the drug should be discontinued. Glycemic control may be impaired, especially in the early stages of treatment, which may require dose adjustment of hypoglycemic drugs. Despite the fact that Fevarin did not cause seizures in animal experiments, special caution is required if it is prescribed to patients with a history of seizures. The drug should not be prescribed to patients with unstable epilepsy, and patients with controlled epilepsy should be closely monitored. If the patient develops convulsions or their frequency increases, Fevarin should be discontinued. There are isolated reports of the occurrence of serotonin syndrome or phenomena similar to neuroleptic malignant syndrome, especially when Fevarin is used simultaneously with other serotonergic and/or neuroleptic drugs. Since these syndromes can cause life-threatening conditions, if symptoms such as hyperthermia, rigidity, myoclonus, frequent changes in blood pressure, pulse and respiratory rate, confusion, irritability, agitation with progression to delirium and coma appear, treatment with Fevarin should be stopped and symptomatic treatment should be performed. therapy. Rarely, while taking Fevarin (as well as other selective serotonin reuptake inhibitors), hyponatremia occurs. Plasma sodium levels return to normal after stopping the drug. Sometimes the occurrence of hyponatremia may be due to the syndrome of inappropriate secretion of antidiuretic hormone. Most cases of hyponatremia have been reported in elderly people. There have been reports of cases of ecchymosis, purpura and gastrointestinal bleeding while taking selective serotonin reuptake inhibitors. These drugs are prescribed with caution, especially in the elderly, concomitantly with drugs that affect platelet function (for example, atypical antipsychotics and phenothiazines, most tricyclic antidepressants, acetylsalicylic acid and other NSAIDs), as well as in patients with a history of hemorrhagic conditions or conditions which are caused by a tendency to bleeding (for example, thrombocytopenia). When used concomitantly with fluvoxamine, plasma concentrations of terfenadine, astemizole or cisapride may increase, increasing the risk of QT and torsade de pointes (TdP). Therefore, Fevarin should not be prescribed together with these medications. The results of a study of fluvoxamine in elderly patients taking the drug in the usual daily dose indicate the absence of clinically significant differences compared with younger patients. However, the dose of the drug in elderly patients should be increased more slowly and carefully. Fevarin may slightly reduce heart rate (by 2–6 beats/min). Use during pregnancy and lactation. Data from a limited number of cases of use of Fevarin in pregnant women do not indicate side effects. No other epidemiological data are available. Animal reproductive studies have shown impaired fertility (at doses 4 times the maximum recommended human dose), increased fetal mortality, decreased fetal weight, and increased incidence of fetal eye abnormalities (puckered retina) at doses of fluvoxamine that significantly exceeded the maximum recommended doses for humans. The potential risk to humans is unknown. Caution must be exercised when prescribing the drug to pregnant women. There have been isolated cases of withdrawal symptoms in newborns after using Fevarin at the end of pregnancy. After the use of selective serotonin reuptake inhibitors during the third trimester of pregnancy, some newborns experienced swallowing and/or breathing disorders, convulsions, temperature instability, hypoglycemia, tremors, impaired muscle tone, trembling and constant crying, which required prolonged hospitalization. The drug is excreted in small amounts in breast milk, so it should not be prescribed to women who are breastfeeding. Children. Fevarin should not be used to treat children except for patients with OCD. In clinical studies, among children who received antidepressants, compared with the placebo group, suicide attempts and suicidal thoughts and aggressiveness (conflict behavior, anger) were more often observed. If a decision is made to prescribe therapy based on clinical indications, the patient must be carefully monitored for the possible emergence of suicidal symptoms. In addition, there are no long-term safety data in children regarding growth, maturation, and cognitive development. The drug cannot be used to treat depression in children due to lack of sufficient experience. The ability to influence the reaction rate when driving vehicles or other mechanisms. Fevarin in a daily dose of 150 mg has no or almost no effect on the ability to drive vehicles and work with potentially dangerous machines and mechanisms. However, during treatment with Fevarin, drowsiness may occur, which must be taken into account before establishing an individual response to the drug.
Manifestations of fevarin withdrawal syndrome
The official instructions for the drug indicate that immediate discontinuation of the drug can lead to withdrawal syndrome. During clinical post-marketing trials of fevarin, no dangerous consequences were identified when stopping this drug. However, some subjects experienced a number of unpleasant side effects.
Fevarin withdrawal syndrome can be suspected when the following symptoms appear:
- Headache;
- Dizziness;
- Trembling and weakness in the arms and legs;
- Paresthesia (feeling of “crawling goosebumps”, electric shock, numbness);
- Insomnia;
- Nightmarish dreams;
- Irritability, aggressiveness, short temper;
- Sudden mood swings;
- Increased appetite.
As a rule, the listed symptoms appear in varying degrees within a day or two after discontinuation of fevarin. Their duration ranges from several days to several weeks. In the most severe cases, some symptoms may persist for a month or more.
Interactions of the drug Fevarin
Fevarin should not be prescribed in combination with MAO inhibitors. Fluvoxamine is a potent inhibitor of CYP 1A2 and, to a lesser extent, CYP 2C and CYP 3A4. Drugs that are metabolized primarily through these isoenzymes are eliminated more slowly and may create higher plasma concentrations when used concomitantly with Fevarin. This is especially true for drugs with a narrow range of indications for use. Careful monitoring of the patient's condition and, if necessary, dose adjustment of drugs is necessary. Fluvoxamine has a moderate inhibitory effect on CYP2D6. It does not appear to affect non-oxidative metabolism or renal excretion. CYP 1A2 When used together with Fevarin, an increase in the previously stable plasma concentrations of tricyclic antidepressants (for example, clomipramine, imipramine, amitriptyline) and antipsychotics (for example, clozepine, olanzapine), which are metabolized primarily through cytochrome P450 1A2, was noted. The need to reduce the dose of these drugs should be considered before starting treatment with Fevarin. Careful monitoring of the condition of patients who simultaneously take fluvoxamine and drugs with a narrow range of indications for use, metabolized by CYP 1A2 (such as tacrine, theophylline, methadone, mexiletine), and, if necessary, adjustment of their doses is necessary. When used together with Fevarin, the concentration of warfarin in the blood plasma increases significantly and the prothrombin time increases. There are reports of special cases of the cardiotoxic effect of the combination of fluvoxamine and thioridazine. The concentration of propranolol in the blood plasma may increase when taken simultaneously with Fevarin and there may be a need to reduce its dose. Plasma caffeine levels may increase. Therefore, patients who consume a significant amount of caffeine-containing drinks are advised to reduce their amount in the diet when used concomitantly with Fevarin, especially if side effects of caffeine are noted (such as tremor, palpitations, nausea, anxiety, insomnia). When taking ropinirole in combination with Fevarin, the concentration of the former in the blood plasma increases and the risk of its overdose increases. Therefore, it is necessary to monitor patients and, possibly, reduce the dose of ropinirole during treatment with Fevarin and after its discontinuation. CYP 2C Careful monitoring of the condition of patients concomitantly taking fluvoxamine and drugs with a narrow range of indications that are metabolized by CYP 2C (such as phenytoin) is necessary, and their doses should be adjusted if necessary. CYP 3A4 Terfenadine, astemizole, cisapride - see SPECIAL INSTRUCTIONS. Careful monitoring of the condition of patients concomitantly taking fluvoxamine and drugs with a narrow range of indications for use, metabolized by CYP 3A4 (such as carbamazepine, cyclosporine), and, if necessary, dose adjustment is necessary. When taken simultaneously with Fevarin, the plasma concentration of benzodiazepines metabolized by oxidation (for example, triazolam, midazolam, alprazolam and diazepam) may increase. Doses of these drugs should be reduced when used simultaneously with Fevarin. Fluvoxamine does not affect the plasma concentrations of digoxin or atenolol. Serotonergic effects may be enhanced when Fevarin is administered in combination with other serotonergic drugs (including triptans, tramadol, selective serotonin reuptake inhibitors and St. John's wort). Fevarin was prescribed in combination with lithium drugs to patients with severe forms of the disease resistant to drug treatment. However, lithium (and possibly also tryptophan) may enhance the serotonergic effect of Fevarin, so they should be prescribed together with caution. Patients taking oral anticoagulants and Fevarin may have an increased risk of bleeding, so these patients should be closely monitored. During treatment with Fevarin, like other psychotropic drugs, you should avoid drinking alcohol.
Analogs
Fevarin is not the only antidepressant of choice today. There are many similar drugs on the market, an analogue of Fevarin:
- Flucosetine. The active substance is flucosetine hydrochloride. In addition to depression and OCD, it acts against bulimia nervosa and is an anorexigenic agent. The spectrum of action includes anorexia.
- Alprazolam is an anxiolytic (tranquilizer). Indicated for neuroses and psychopathy. Effective against phobias, anxiety disorders, reactive depression, withdrawal syndrome, relieves agitation. The spectrum of action is much wider than that of Fevarin.
- Bromazepam. This is a tranquilizer that acts against diseases such as neuroses and psychopathy, relieves anxiety, and relieves insomnia. This drug is used in an outpatient or hospital setting.
- Haloperidol is an antipsychotic. It is used in the treatment of alcohol dependence, schizophrenia, manic episodes, personality and behavioral disorders, relieves agitation, but causes drowsiness.
Fevarin overdose, symptoms and treatment
The most common symptoms are nausea, vomiting, diarrhea, drowsiness and dizziness; possible tachycardia, bradycardia, arterial hypotension; liver dysfunction; convulsions and coma. Fevarin has a fairly wide range of safety in case of overdose. Reports of deaths due to overdose of Fevarin alone are isolated. The highest recorded dose of the drug during an overdose was 12 g. The patient who took it completely recovered. More serious complications have been reported in cases of deliberate overdose of fluvoxamine in combination with other drugs. Treatment is symptomatic. There is no special antidote. In case of overdose, you should rinse your stomach as soon as possible, take activated charcoal, and carry out maintenance therapy. If necessary, osmotic laxatives are prescribed. The effectiveness of forced diuresis or dialysis is questionable.
Overdose
With an overdose of the drug, side effects increase - dizziness, anxiety, nausea, vomiting, abdominal pain, confusion and others. When the recommended dose is significantly exceeded multiple times, the heart rhythm is disturbed, blood pressure decreases, convulsions begin, and liver failure develops up to coma. There have been several cases of death due to an overdose of the drug.
There is no specialized substance – fluvoxamine antidote. Symptomatic therapy is carried out. Gastric lavage, enterosorbents are administered. Next, the main symptoms are monitored and relieved depending on the frequency of exceeding the specified dose and the development of adverse symptoms. If necessary, osmotic laxatives are administered. Diuresis is ineffective.