Neoplasms of the nervous system are increasingly encountered in the clinical practice of doctors of all specialties.
The incidence of primary neurotumors averages 7-14 cases per 100 thousand population per year.
An atypical, poorly differentiated cell with an uncontrolled division process can arise in all tissues of the brain and spinal cord (neurons, astrocytes, glial elements, ependymocytes), as well as in the cells of blood vessels, peripheral nerves, glandular formations and membranes.
One type of tumor of the central nervous system is ependymoma.
Basic Concepts
A neuroepithelial tumor of a thin layer of cells lining the surface of the brain's ventricles and central canal is called an ependymoma.
It is more common in children, although the disease is quite common among adults. According to the histological structure, ependymoma belongs to glial formations.
The posterior cranial fossa is considered the most typical place where cerebral ependymoma can be localized. The location of the tumor in the lateral (right or left) ventricle is also considered typical. The neoplasm is most often benign and does not tend to grow rapidly or invade nearby tissues. However, given the direct contact of ependymomas with the cerebrospinal fluid, tumor metastasis through the cerebrospinal fluid pathways is possible. The prognosis of the disease is largely determined by the shape of the tumor .
Surgery for spinal cord astrocytoma
Astrocytoma is one of the most common tumors from the group of gliomas, formed inside the spinal cord by neuroepithelial cells (astrocytes) of atypical growth. This is a primary disease that can be benign or malignant. According to statistics, males are 1.5 times more likely than females to be susceptible to this pathology. Astrocytic gliomas mostly form in the cervical and cervicothoracic areas. Most often they affect the pediatric category of patients of younger and middle age.
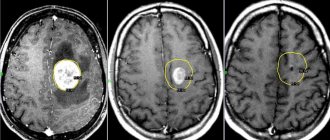
Astrocytoma on MRI slice.
For glioma of any type, questions about removal, for glioblastoma, similarly, are decided on the basis of specific data: subtype, location, degree of tumor, age and health status of the person. Currently, improved neurosurgical developments make it possible to safely eliminate this type of tumor, but bright prospects are possible only with their early detection and timely treatment.
At stages 1-2, the formation has a clear boundary from healthy tissue, so it is easily recognized and can be safely removed radically with minimal risk of relapse in the long-term postoperative period. With each subsequent stage, the growth of infiltration and invasion of the neoplasm progresses, which significantly worsens the prognosis for cure and prolongation of human life.
Treatment is based on microsurgical surgery with neuronavigation for complete or partial resection of glioma, followed by radiotherapy sessions. In the final stages, when the tumor is operable, a course of radiation therapy is initially prescribed in order to achieve the maximum possible separation of the tumor tissue from healthy structures, and only then the surgical part of the treatment begins. Chemotherapy is practically not used for this diagnosis.
The clinical picture of astrocytomas is characterized by local pain, curvature of the spine, inhibition of motor skills, forced position of the head, which appears to the patient as a necessity to reduce painful phenomena.
Causes
The nature of the development of ependymomas is not fully understood. It is believed that this is a polyetiological disease. Recently, the theory of the occurrence of ependemoma as a result of exposure to the SV40 virus has become widespread. It was this representative of polyomaviruses that was found in some patients with neoplasms from the ependymal epithelium.
The US National Cancer Institute, after conducting two independent studies, suggested that the SV40 virus does not cause the development of ependymoma in humans, despite the fact that it can cause cancer in some experimental animals.
Other factors that provoke the formation of ependymoma include:
- Genetic predisposition;
- Chronic intoxication;
- Hormonal disorders;
- Radioactive radiation;
- Infectious and inflammatory diseases;
- Injuries.
Rehabilitation after spinal cord surgery
The final result of the patient’s functional recovery entirely depends on how adequate and complete the postoperative rehabilitation is. The patient receives first medical care while still in the hospital; then he should continue his recovery in the rehabilitation department or in a specialized center for this profile. Recovery after spinal surgery is a long process, generally lasting 12 months. Of these, at least 3 months a person needs careful monitoring by doctors.
Rehabilitation therapy consists of 3 stages, each of which includes its own tasks and a set of therapeutic measures.
- Stage I – eliminating pain, preventing possible complications, working on the muscle complex in a gentle manner, bringing the general state of health back to normal, learning basic self-care skills, walking with supporting devices.
- Stage II – compensation of asymmetry of the pelvic axis, upper and lower back, elimination of paresis and restoration of sensitivity of the limbs, return of control over the functioning of the pelvic organs, gradual expansion of the range of physical skills at the everyday level, fruitful work on strengthening the musculoskeletal system.
- Stage III – full or maximum possible restoration of biomechanics and stabilization of the endurance of the musculoskeletal center, returning the patient to a natural social environment with some restrictions on physical activity.
It doesn’t matter whether the operation was aimed at treating spasticity after an injury, removing a tumor, or another therapeutic goal, without strict adherence to a special wellness plan, positive dynamics will be impossible.
Rehabilitation consists of:
- drug treatment - antibiotics, anticoagulants, vitamin-mineral complexes, NSAIDs, neuroprotectors, etc.;
- regular therapeutic exercises are daily dosed exercise therapy sessions (the introduction of new elements, the duration and intensity of the load is carried out gradually and very carefully);
- physiotherapy – electrophoresis, diadynamic therapy, ultrasound, magnetic therapy, laser therapy, electrical stimulation, etc.;
- massage, manual therapy and reflexology - the impact of specialist hands, as well as special tools on important areas of the human body ;
- sanatorium-resort treatment is always prescribed immediately after completion of the main course of rehabilitation (it is recommended to take place 1-2 times a year) .
Classification
Ependymomas of the central nervous system can be benign (more common) or malignant (relatively rare). The degree of differentiation of ependymoma cells directly determines the prognosis of the disease.
Representatives of benign tumors are the following forms of ependymoma:
- True with a typical arrangement of cells and a tendency to recur in the same place;
- Papillary with characteristic villi and trabeculae;
- Myxopapillary – a form of extramedullary tumor with symptoms of mucous degeneration;
- Subependymoma has the appearance of a node, located under the ependymal tissue.
Among malignant neoplasms there are:
- Anaplastic form. Has rapid growth, poorly differentiated cells, and a tendency to metastasize.
- Ependymoblastoma. An extremely rare malignant neoplasm. Mostly children under five years of age are affected. It is characterized by severe consequences, high mortality rates, and frequent relapses.
Myxopapillary ependymoma, which belongs to the benign formations of the cauda equina, in practice can have a pronounced aggressive course.
Clinical picture of the disease
The symptom complex of the disease will depend on the shape of the epindymoma, its location and size.
In the initial stages, the disease manifests itself by signs of increased pressure in the cerebrospinal fluid tract:
- Compressive headache, often in the frontal region,
- Dizziness
- Pain and pressure in the eyeballs
- Nausea not associated with food intake
- Vomiting, and not bringing relief
- Irritability
- Emotional lability.
If the tumor completely blocks the cerebrospinal fluid pathways, convulsive paroxysm may develop. Often this phenomenon can accompany aggressive tumors of the lateral ventricle.
Brain ependymoma is manifested by the addition of focal neurological symptoms, depending on the topic of the pathological process. Localization of the tumor in the posterior cranial fossa gives rise to the phenomena of vestibulo-cerebellar syndrome - unsteadiness of gait, unsteadiness when walking, impaired coordination of movements. Tumors located in the region of the IV ventricle, where the nuclei of most cranial nerves are localized, can manifest as oculomotor disorders, hypoesthesia and facial asymmetry, hearing loss, swallowing disorders, low voice and unclear speech.
Ependymomas of the spinal cord appear:
- Pain syndrome in the back,
- Sensory impairment of the spinal conduction type.
- Paresis and paralysis of the limbs
- Violations of the functions of the pelvic organs.
Treatment of ependymoma
The only effective treatment for ependymoma is radical removal of the tumor. Surgical treatment is performed by a neurosurgeon using microsurgical technologies. During the entire manipulation, motor and sensory potentials are monitored.
During the operation, the benign formation is easily separated from the surrounding tissue and completely removed. For a malignant tumor, extended resection of neoplasia is performed. In the postoperative period, a control MRI is performed. If the slightest part of the tumor is not removed, repeat surgery is recommended.
Radiation therapy is carried out when the malignant nature of the ependymoma is confirmed. In the future, a course of rehabilitation with massage and exercise therapy is required. Drug treatment involves the prescription of anti-inflammatory, vascular, and neurometabolic drugs.
Diagnostics
Confirming the diagnosis of ependymoma requires a number of instrumental diagnostic procedures. First of all use:
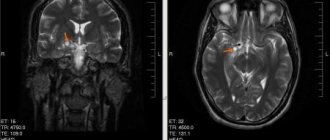
- Neuroimaging (MRI or CT);
- Neurosonography (for children of the first year of life);
- Electroencephalography;
- Lumbar puncture with biochemical and cytological examination of the cerebrospinal fluid;
- Myelography;
- Ventriculoscopy;
- Angiography;
- Direct ophthalmoscopy;
- Stereotactic biopsy.
The final diagnosis takes place after the conclusion of a histological examination of the ependymoma material obtained intraoperatively.
Tests to make a diagnosis
To diagnose the disease, a specialist may prescribe the following examinations:
- Magnetic resonance imaging of the brain.
- X-ray contrast diagnostics (angiographic examination) of the vessels of the head and spine.
- Myelography is an examination that allows, using the injection of contrast, to examine the paths of the cerebrospinal fluid.
- Electroencephalogram (a test that detects the electrical activity of the brain).
- Ventriculoscopy (3rd and 4th ventricles of the brain).
- Ultrasonography (this examination is prescribed for young children whose fontanel is not overgrown).
WE RECOMMEND WATCHING: How does a cerebellar tumor manifest?
A number of additional examinations are also prescribed by highly specialized specialists:
- Consultations with an ophthalmologist (testing the patient's vision).
- A lumbar puncture may be prescribed to examine the cerebrospinal fluid (if a tumor in the spinal canal is suspected).
- Carrying out a stereotactic biopsy to examine tumor tissue.
- Consultation with a neurologist with testing of skin sensitivity and assessment of reflex functions.