Neuroleptics are psychotropic drugs. They are the main group of psychotropic medications used to treat all types of schizophrenia and mental disorders.
The term “neuroleptics” itself comes from the ancient Greek νευρον, which means nerve, nervous system, and the ancient Greek ληψη, which means retention. When determining the names of the drugs, it was assumed that they help keep the nervous system in a certain stable state.
However, the first antipsychotics showed a side effect called neurolepsy. This is a condition in which the patient’s motor and mental activity decreases, and indifference to others develops.
This unpleasant side effect was reduced in subsequent generations, however, the name was considered outdated and the more adequate name is now used - antipsychotic drugs or antipsychotics.
But the term “neuroleptics” is also used.
Attention! There are no antipsychotic medications available without a prescription. All of these drugs are strictly prescription drugs (even if you look at the names given in articles on other sites, these drugs are also sold by prescription, so this is a deliberate lie and misinformation). And there are no antipsychotics without side effects either.
Neuroleptics - what are they?
Neuroleptics are a group of drugs that can have a calming and inhibitory (in some cases depressant) effect on the central nervous system. They are also called antipsychotic drugs or antipsychotics.
For reference. Antipsychotic drugs are highly effective in eliminating pathological agitation (affective disorders), delusions, hallucinatory attacks, mental automatisms and other signs of psychosis.
In old reference books, neuroleptics are mentioned under the names of neuroplegics, antischizophrenic drugs, major tranquilizers, and ataractics.
Most often, antipsychotics are used in psychiatric practice. Traditionally, the main indications for prescribing antipsychotics are:
- schizophrenia (antipsychotic drugs are used to relieve acute psychosis, as well as for long-term maintenance treatment);
- schizoaffective disorders;
- bipolar affective disorder;
- major depression;
- obsessive-compulsive disorder.
Less commonly, antipsychotic drugs are prescribed in small dosages for non-psychotic diseases accompanied by the development of pathological agitation.
Neuroleptics can be used for psychomotor, emotional, neuroendocrine disorders, and neurodegenerative diseases.
When using antipsychotic medications, it is important to remember that they should only be used as prescribed by a doctor.
It should also be noted that all antipsychotics are prescription drugs. That is, antipsychotics are not sold in pharmacies without a prescription.
“Over-the-counter antipsychotics” advertised on the Internet are not antipsychotics; they are often the name given to powerful sedatives. However, even “non-prescription antipsychotics” have their side effects and should be used strictly according to indications.
Mechanism of action of antipsychotics
The effects that antipsychotic drugs have on the body are quite multifaceted.
For reference. The main pharmacological effect of antipsychotics is manifested by a calming effect (without impairment of consciousness), a decrease in the body's response to external stimuli, inhibition of pathological psychomotor agitation and affective tension, suppression of feelings of fear, anxiety and attacks of aggression.
When used in standard dosages, antipsychotics do not have a pronounced hypnotic effect, but can induce light drowsiness (promoting deeper relaxation and rapid onset of sleep).
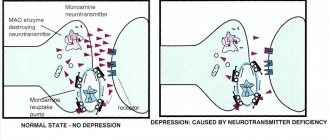
The neurochemical mechanisms of action of all antipsychotics are due to their interaction with dopamine brain structures. Antipsychotic drugs inhibit the transmission of nerve impulses in those systems where the main neurotransmitter is dopamine.
Due to this, the antipsychotic effect of neuroleptics is achieved. The sedative and hypotensive effects of antipsychotics are realized mainly due to the inhibitory effect on central noradrenergic receptors.
What are dopamines
To better understand the actions of antipsychotics, a few words about dopamines.
First of all, dopamines are neurotransmitters. This is the name given to biologically active chemicals that act as intermediaries in the transmission of electrochemical impulses between nerve cells.
Dopamine molecules help exchange information in the so-called dopamine systems.
There are several subsystems in the dopamine system of the brain. One is responsible for the functioning of the cerebral cortex, the other, extrapyramidal , for muscle tone, and the third for the production of hormones in the pituitary gland.
It is important to understand that it is the dopamine subsystems that determine the cognitive capabilities of a particular person - thinking, speech, attention, memory.
For reference. Failures in the dopamine neurotransmitter system are the most important biological prerequisite for the disease schizophrenia. Acceleration of the transmission of nerve impulses leads to unreasonable excitement with loss of control.
The task of psychotics (neuroleptics) is to partially block dopamine receptors (D2 type) to slow down the transmission of nerve impulses. The blockade is needed at least 60-65%.
However, reducing the transmission speed leads to negative consequences. For example, to emotional autism, social isolation, or apathy.
To eliminate such costs, modern antipsychotics are given the property of an “antipsychotic threshold” below which the antipsychotic effect is not realized. Although not completely. Only nonspecific effects appear - hypnotic, sedative and anti-anxiety, or, on the contrary, activating and disinhibiting, as well as antiemetic.
Pharmacological and therapeutic effects
Due to their influence on different brain structures, antipsychotics have multiple effects on the body. When treating diseases, the ability of antipsychotics to calm the nervous system and reduce the effects of stress and other external influences is primarily taken into account. Therefore, they are successfully used for schizophrenia and other severe mental illnesses. They help quickly eliminate:
- psychomotor agitation
- phobia
- affective tension
- aggression
- hallucinations
- rave
- automaticity syndrome, etc.
Without directly affecting the quality and quantity of sleep, neuroleptics, by enhancing inhibitory processes, accelerate falling asleep and potentiate the effect of sedatives, narcotics, analgesics and anesthetics.
The simultaneous use of psychostimulant drugs reduces the effectiveness of therapy. The pharmaceutical action of antipsychotics is as follows:
- calming (sedative)
- tranquilizing
- antiemetic
- hypotensive
- potentiation of the effects of drugs, sleeping pills, tranquilizers, alcohol
They also reduce the frequency of hiccups and coughs, and eliminate the negative manifestations of autonomic reactions. Some types of antipsychotic medications may improve mood during depression.
Classification of antipsychotics
There are several classifications of antipsychotic drugs. One of the most common classifications is the division of antipsychotics into atypical and typical.
The list of typical antipsychotic drugs includes a group of derivatives:
- Phenothiazine, divided into:
- aliphatic derivatives (preparations of levomepromazine (Tizercin), chlorpromazine (Aminazine), alimemazine (Teraligen));
- piperazine derivatives (preparations of perphenazine (Etaperazine), trifluoperazine (Triftazine), fluphenazine (Moditen-depot), thioproperazine (Mazeptil));
- piperidine derivatives - preparations of pericyazine (Neuleptil), thioridazine (Sonapax)).
- Butyrophenone (haloperidol, droperidol preparations).
- Indole (drugs ziprasidone (Zeldox), sertindole (Serdolekg)).
- Thioxanthene (preparations of flupenthixol (Fluanxol), chlorprothixene (Truxal), zuclopenthixol (Clopixol)).
The list of atypical antipsychotics includes the following drugs:
- quetiapine (Quentiax);
- clozapine (Azaleptin, Leponex);
- olanzapine (Zyprexa);
- amisulpride (Solian);
- sulpiride (Eglonil);
- risperidone (Rispolept);
- aripiprazole (Zylaxera).
Antipsychotic drugs - list
Antipsychotics come in a huge variety. The specialist has the opportunity to select the optimal antipsychotics for a particular patient - he always has a list of drugs at hand. Before making a prescription, the doctor assesses the condition of the person contacting him and only after that makes a decision on what medicine to prescribe. If the desired result is not achieved, the specialist may re-prescribe antipsychotics - the list of drugs will help you choose a “replacement”. At the same time, the doctor will prescribe the optimal dosage of the new medicine.
Generations of antipsychotics
Typical antipsychotics are represented by the following drugs:
- Chlorpromazine;
- Haloperidol;
- Molindon;
- Thioridazine and so on.
The most popular new generation antipsychotics without side effects:
- Abilify;
- Fluphenazine;
- Quetiapine;
- Fluanxol;
- Triftazin;
- Levomepromazine.
Neuroleptics - list of drugs without prescriptions
There are few such medicines. However, you should not think that self-medication with them is safe: even antipsychotics sold without prescriptions should be taken under the supervision of a doctor. He knows the mechanism of action of these medications and will recommend the optimal dosage. Antipsychotic drugs without prescriptions - list of available drugs:
- Olanzapine;
- Serdolect;
- Ariprizole;
- Etaperazine;
- Chlorprothixene.
Indications for the use of neuroleptics
Most often, antipsychotic drugs are prescribed to eliminate productive symptoms: delusions, hallucinatory attacks, illusions, severe behavioral disorders, pathological psychotic agitation, mania.
Atypical antipsychotics are often used to eliminate negative (deficit) symptoms: signs of emotional exhaustion, autistic disorders, signs of personality disintegration.
Antipsychotic drugs may be used to treat:
- chronic and acute psychoses;
- psychomotor forms of agitation;
- chronic forms of insomnia;
- Tourette's syndrome;
- schizophrenia (neuroleptics can be used both to relieve acute attacks and for maintenance therapy);
- manic episodes;
- severe phobias;
- hallucinations;
- movement disorders associated with mental illness;
- disorders of somatoform and psychosomatic type;
- bipolar affective disorder.
For reference. Also, antipsychotics can be used one-time to relieve ongoing bouts of vomiting (if other medications are ineffective), as well as for preoperative preparation of the patient.
Less commonly, antipsychotic drugs are used when the patient has constant mood swings.
According to the APA (American Psychiatric Association) guidelines, antipsychotic drugs are not recommended for use as drugs of choice for the treatment of behavioral and psychological disorders in patients with dementia.
Attention. Neuroleptics are not the drugs of choice for the treatment of insomnia (they can be used strictly according to indications, in case of severe insomnia and the ineffectiveness of other medications).
Cognitive effect of antipsychotic drugs
The cognitive benefit is not a side effect.
For reference. Cognitive functions are the complex cognitive functions of the main organ of the central nervous system - the brain. With their help, a person not only learns about the world around him, but also actively interacts with it.
Thanks to cognitive functions (thinking, speech, memory, attention), a person’s personality is formed, and his abilities for education, work and other areas of life are determined.
When taking antipsychotics, these functions are partially blocked. There is a cognitive effect. What is needed is something between the effectiveness of the drugs and the reduction in cognitive effect.
In a prospective efficacy study, it was theorized that atypical antipsychotics were more effective than typical antipsychotics in the treatment of neurocognitive impairment.
To accept or not to accept?
Photo from clinicaladvisor.com
“Don’t be afraid to take antipsychotics” is the title of an article by one doctor, in which he tries to convince the reader that these drugs are not nearly as scary as they are made out to be, and that their benefits are great.
And in fact: delusions, hallucinations, psychotic agitation, mania - each of these manifestations of a mental disorder can turn the life of both the patient and his loved ones into hell, and in some cases, cause suicide.
A number of scientific studies indicate that antipsychotics can help, if not every patient, but a significant number of them, to escape from the worst.
However, the neuroleptic revolution consisted not only in the fact that the straitjacket, stun gun and life in a psychiatric clinic were replaced by pills taken by the patient at home on a schedule, which, of course, is a huge humanitarian achievement. Its wave swept through hundreds of thousands of children and adults who did not suffer from schizophrenia or bipolar disorder.
Indications for antipsychotics gradually expanded, and they began to be used to treat children with neurodevelopmental disorders, adults with depression, anxiety and obsessive-compulsive disorders, senile dementia, and physical aggressiveness of unknown origin.
Do they have a positive effect on these mental disorders?
Research results are contradictory.
Here, for example, are the absolutely shocking figures from a 2008 British study published in the number one medical journal in the world, namely the Lancet. Scientists examined the effectiveness of classical haloperidol and atypical risperidone in stopping aggression and defiant behavior in patients with mental retardation without a diagnosis of schizophrenia.
The 86 study participants were divided into three groups. For 4 weeks, each group received risperidone, haloperidol, or placebo, respectively. By the end of the period, the haloperidol group experienced a 65% reduction in symptoms, the risperidone group by 58%, and the placebo group by 79%!
The dummy drug turned out to be more effective than both typical and atypical antipsychotics, without causing - of course - negative side effects.
“Antipsychotics should no longer be considered an acceptable treatment for aggressive and challenging behavior in people with mental retardation,” British scientists have concluded.
Side effects of antipsychotic drugs
Attention. All antipsychotic drugs have a wide range of severe side effects.
The likelihood of developing side effects during therapy with antipsychotic drugs depends on the patient’s age, the presence of concomitant diseases, prescribed dosages, regimens and duration of treatment with antipsychotics.
Frequent side effects from the use of antipsychotics are headaches , decreased blood pressure and fainting, constant dizziness , anxiety, drowsiness, slurred speech, and lethargy.
With long-term use, problems with potency, infertility, visual impairment, hyperprolactinemia, diabetes mellitus develop, and the secretion of somatotropic hormone, thyroid-stimulating hormone, and oxytocin decreases.
Disorders of the cardiovascular system can manifest themselves as tachycardia, extrasystole, the development of drug-induced myocarditis (inflammation of the myocardium), stroke, myocardial ischemia, myocardial dystrophy.
It is also possible to develop epileptic seizures, thrombocytopenia, pneumonia, hyponatremia, aplastic anemia, bleeding disorders, and decreased immunity.
For reference. In addition, during therapy with antipsychotics, patients complain of feelings of severe inhibition of thinking, loss of their character, feeling like a “vegetable” or “unreal,” and the inability to derive pleasure from activities that previously brought them joy.
New generation neuroleptics without side effects
Please note that the phrase “no side effects” in the subtitle is the wish of patients or their relatives who have heard about the negative effects of antipsychotics.
Attention. There are no antipsychotic drugs without side effects. Even the most modern antipsychotics have side effects. This is due to the general mechanism of action of this group of drugs and its effect on dopamine receptors.
The general mechanism of action on dopamine receptors occurs through four main pathways:
- mesolimbic (reducing or blocking dopaminergic transmission in these areas of the brain leads to a pronounced antipsychotic effect and relief of productive symptoms: delirium, hallucinatory attacks);
- mesocortical (with blockade of dopamine receptors in this mesocortical area of the brain when using typical antipsychotics for long-term therapy, it can lead to increased negative symptoms: apathy, poor speech, personality disintegration);
- nigrostrial (when dopamine receptors in the nigrostrial pathway are blocked, it leads to the development of such typical side effects of neuroleptics as the development of parkinsonism, painful spasms of the jaw muscles, muscle tremors, pathological restlessness);
- tuberoinfundibular (blocking dopamine receptors in the limbic pathway leads to the development of hyperprolactinemia, gynecomastia (enlargement of the mammary glands in men), galactorrhea (secretion of milk from the mammary glands outside of lactation), menstrual irregularities, the development of osteoporosis, the appearance of infertility, problems with potency, increased risk of developing oncology with long-term use).
Atypical antipsychotics affect dopamine receptors less than typical antipsychotic drugs. In this regard, they are less likely to cause complications such as neuroleptic depression, hyperprolactinemia, and parkinsonism.
However, atypical antipsychotics can cause life-threatening hyponatremia, have high hepatotoxicity, cause sexual dysfunction, and significantly increase the risk of developing cardiovascular pathologies.
Also, atypical antipsychotics can lead to the development of diabetes, stroke, pneumonia (while taking antipsychotics, the risk of developing pneumonia increases by more than 60%), and visual impairment.
Important! In this regard, all antipsychotics should be used only as prescribed by a doctor and strictly under his supervision. Independent adjustment of dosages and treatment regimens is unacceptable.
About opening a group and starting to use it
As mentioned above, the first antipsychotic was developed back in the 50s, but it was discovered by accident, since Aminazine was originally invented for surgical anesthesia, but after seeing the effect it has on the human body, it was decided to change the scope of its application and in 1952, Aminazine was first used in psychiatry as a potent sedative.
The main merit of this remedy should be attributed to the abolition of lobotomy, since a similar effect from this procedure could be obtained using medication without surgery.
A few years later, Aminazine was replaced by the more improved drug Alkaloid, but it did not stay long on the pharmaceutical market and already in the early 60s, second-generation antipsychotics began to appear, which had fewer side effects. This group includes Triftazin and Haloperidol, which are still used today.
Today, powerful tranquilizers are also considered neuroleptic drugs, since they have a similar effect.
The procedure and features of the use of antipsychotics
The treatment regimen is selected individually and depends on the severity of the diagnosis and symptoms.
With the fast method, the dose of antipsychotics is adjusted to the optimal dose in 1-2 days, then the required concentration of the drug in the blood is maintained.
With a slow increase, the dose of the drug taken is gradually increased. In the case of using a zigzag technique, alternate the use of high and low dosages of the drug.
Treatment with pauses can also be used (the drug is stopped for 5-6 days).
Important. The duration of taking antipsychotics is also calculated individually.
To prevent the development of withdrawal syndrome, after stopping treatment, the doctor gradually reduces the dose of the drugs used or transfers the patient to tranquilizers. In addition, B vitamins may be prescribed.
When using antipsychotics it is prohibited:
- take simultaneously two drugs with a pronounced antipsychotic effect or two drugs with a sedative effect;
- take 3 or more antipsychotics;
- combine atypical and typical drugs.
Also, before prescribing antipsychotic drugs, the patient should exclude the presence of pregnancy, porphyria, parkinsonism, severe diseases of the cardiovascular system, agranulocytosis, angle-closure glaucoma, kidney and liver pathologies.
Types of neuroleptic therapy
- Neuroleptic therapy is possible in an active form: administration through injections and infusions (used to quickly achieve an effect using small doses).
- Inactive antipsychotic therapy is the most common type of treatment: drugs are taken in tablet form according to the regimen prescribed by the doctor. Used to treat conditions that are not severe and do not require a quick effect, to maintain remission.
- Depot therapy. The antipsychotic drug is given as an injection (usually oil-based for slow release). The injection is given once every 2-4 weeks, ensuring a constant supply of the drug to the body. A convenient form of treatment that allows you not to constantly monitor the patient (whether you took the medicine or not, forgot or didn’t forget).