What is absence epilepsy
Absence epilepsy is a generalized seizure that occurs most often in children aged 3 to 14 years. From the outside it is not easy to identify, since it looks more like thoughtfulness and daydreaming.
Few people know what absence seizures are in epilepsy in adults and children. They are characterized by a short-term clouding of reason, accompanied by a fixed gaze at one point, frequent blinking or rolling of the pupils upward. The patient may experience 50 to 100 episodes per day. In many young patients, this type of disease goes away on its own by the onset of adolescence.
Diagnostics
The identification and subsequent treatment of absence epilepsy is carried out by a neurologist or epileptologist.
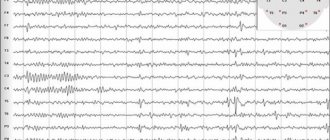
To make a diagnosis, a characteristic clinical picture and specific changes in the electroencephalogram (EEG) are required. According to EEG data, absence seizures are divided into typical and atypical.
Typical ones include simple and complex absence seizures, in which the electroencephalogram reveals generalized, synchronous, symmetrical peak-wave activity with a frequency of 3 waves per 1 second, slowing down during the seizure to 2-2.5. In the vast majority of cases, they occur in children.
An atypical absence seizure according to EEG data is an attack with symmetrical, bilateral peak waves with a frequency of 2 per second, multiple peak waves with a frequency of 4-6 per second.
Despite the fact that the electroencephalogram is the “gold standard” for diagnosing absence epilepsy (especially if performed during a seizure), there are patients with a completely normal EEG.
To exclude organic pathology of the brain (tumors, cysts, inflammatory diseases), the patient is shown magnetic resonance or computed tomography.
Symptoms of absence epilepsy
With absence seizure, a short-term clouding of consciousness occurs; at this moment, the victim can look into the “emptiness” straight ahead for 5-30 seconds, without responding to external stimuli. After the episode ends, everything returns to normal, so seizures may go undetected.
The main difficulty associated with non-convulsive absence epilepsy is the risk of confusing the disease with thoughtfulness, which is why the disease often remains without due attention. The symptoms of absence epilepsy in adults are not always clear, but the main signs include:
- unfocused gaze;
- lack of response to external influences;
- stopping a sentence mid-sentence at the time of an attack;
- confused movements of the limbs;
- blinking;
- aimless wandering.
Causes
Absence epilepsy refers to idiopathic forms of the disease, i.e. the reason for it has not been reliably established.
The leading role in development is currently assigned to hereditary mutations, but a single causative gene has not been found.
In patients with different clinical manifestations, different parts of the chromosomes are changed.
As a result, an epileptic focus is formed in a region of the brain, which determines “convulsive readiness.” For the full development of the disease, a combination with risk factors is necessary:
- brain injuries;
- inflammatory diseases of the central nervous system (including those occurring in utero);
- tumor neoplasms of the brain.
Provoking factors that directly trigger attacks are:
- hyperventilation, which causes changes in the ratio of oxygen and carbon dioxide in the blood;
- chronic intoxication with various toxic substances;
- disruption of the content of neurotransmitters in brain neurons;
- increased mental activity;
- stress;
- insomnia;
- rapidly changing visual objects (TV, monitor).
Find out more about epilepsy and its types:
- cryptogenic and generalized;
- idiopathic and myoclonic;
- partial and focal;
- congenital and acquired;
- alcoholic and drug-resistant;
- Kozhevnikovskaya and Jacksonian;
- rolandic and temporal;
- nocturnal and symptomatic.
What types of absence seizures are there?
Many people wonder: “What is absence epilepsy?” There are several main types. Typical or simple is characterized by short-term clouding of consciousness. The victim suddenly stops talking and freezes, as if frozen. At the same time, the gaze is directed clearly in front of you, and facial expressions do not change. The patient does not respond to touch, voice, words and other external factors. During the episode, the patient does not answer questions, and his speech breaks down into occasional silence. However, after a couple of seconds, mental activity returns to normal, and there are no memories of what happened, because for the patient himself it goes unnoticed, the victim simply continues the interrupted action.
A characteristic feature is a high frequency, in particularly tense situations reaching several tens and hundreds of seizures per day. They are provoked by the following phenomena:
- active mental activity;
- excessive relaxation;
- hyperventilation;
- lack of sleep;
- flashes of light;
- flickering TV or computer screen.
Absence seizures are manifested by the following clinical picture of simple episodes:
- lasts a matter of seconds;
- the victim has no reaction and is unconscious;
- the person does not notice the attack.
The paroxysm can last 5-30 seconds, during which the patient loses conscious perception of the surrounding world. From the outside, one can notice the lack of a conscious look, the person’s switching off from the activity and a short period of freezing in place. A pronounced episode is caused by a stop in the beginning of speech or actions, as well as an inhibited continuation that occurs before the attack of activity.
In the first case, after the onset of paroxysm, there is a restoration of motor activity and words exactly from the episode where they stopped. The victims characterize this condition as a sudden stupor, loss of memory, loss of reality, trance. In the post-attack time, the patient’s health is normal.
Another type of seizure is more noticeable both for the victim and for others, as it is distinguished by motor and tonic phenomena. Paroxysm occurs with a decrease in muscle activity, which leads to drooping of the head and weakening of the limbs. In rare cases, the patient may slide out of the chair, and with total atony, fall.
Tonic paroxysms are accompanied by muscle hypertonicity. Depending on the location of the lesions, the following may be noticeable:
- body bending;
- flexion and extension of limbs;
- throwing back the head.
An attack with a myoclonic component is characterized by low-amplitude muscle contractions in the form of frequent body jerks. An adult may experience twitching of the corners of the mouth, chin, and eyelids. Myoclonus occurs:
- symmetrical;
- asymmetrical.
Automatisms that occur during an episode can be of the nature of elementary but repetitive movements:
- mumbling;
- swallowing;
- chewing;
- rubbing hands;
- leg swing;
- fastening buttons or buttons.
The frequency of complex ones can vary from several to dozens of times a day. Episodes may be the patient's only manifestation, which is more common in children.
Features of absence epilepsy by age
At different ages, childhood absence epilepsy can occur differently and has specific features.
In childhood
Childhood absence epilepsy is the most favorable form. It makes its debut at 6-7 years of age and appears more often in girls. Mostly typical absence seizures are observed (in 35% of cases - simple, in 43% - complex, and in 22% of cases they are combined). The attacks occur mainly in the first half of the day and are repeated very often - up to several dozen times a day.
In adolescence
Absence epilepsy that occurs in adolescence is called juvenile. Unlike DAE, it has some features. The disease begins at a later age - at 8-14 years. In such patients, simple absence seizures predominate, occurring in 66% of cases.
With juvenile absence epilepsy, the frequency of attacks is lower - they are observed up to several times a day. In adolescence, the disease may appear due to changes in lifestyle, which can provoke various stressful situations. In addition, young men often imitate adults, adopting their habits - they start smoking and drinking. This can cause alcohol intoxication, which leads to disorders in the cerebral cortex, provoking epilepsy.
Nonconvulsive absence epilepsy
Pathology occurs much more often at an early age, from 7 to 14 years, and in youth - from 15 to 30 years. Until the age of four, simple absence seizures do not occur in patients, since a certain maturity of the brain is required for the manifestation of this phenomenon.
The trigger mechanism for nonconvulsive neuralgia is:
- neuroinfection;
- skull injuries.
During nonconvulsive paroxysms, gustatory, olfactory and visual hallucinations may occur. A characteristic feature of the disease is a large number of clinical manifestations. Therefore, organic diseases of various etiologies, in the absence of qualified assistance, tend to become chronic.
Main manifestations
Absence epilepsy most often manifests at an early age - from 3 to 8 years. Children experience epileptic paroxysms that develop in a certain way:
- The attack always begins unexpectedly. There are no warning signs of the condition.
- Due to loss of consciousness, the child stops responding to surrounding people and events. At the same time, muscle tone is preserved, and therefore the baby’s posture remains the same.
- After an absence attack, the child cannot remember it. This period of time completely disappears from his consciousness.
From the outside, absence seizures look like a complete lack of movement, which lasts several tens of seconds. Convulsive phenomena, as well as drowsiness and fatigue after an attack are not observed, which distinguishes absence paroxysms from classic epileptic seizures. If a child develops complex absence seizures, various stereotypical movements appear, which can be regarded by others as meaningful activities: unbuttoning and fastening buttons, licking lips, etc. Complex absence seizures last up to several minutes. Consciousness is gradually lost at the onset, and in the period after the attack, children develop weakness and apathy.
Paroxysms are the main symptoms of absence epilepsy in children and adolescents. At the beginning of the disease they occur several times a day. However, with further progression, their frequency increases and can reach several dozen paroxysms per hour.
Manifestations in adolescents
Epileptic paroxysms, when they occur in adolescents, serve as the basis for the diagnosis of juvenile absence epilepsy. The disease first manifests itself between the ages of 9 and 15 years and has a number of clinical features. The main manifestation of epilepsy is simple absence seizures.
Often the disease develops after severe stress, which may be associated with school, family relationships or the teenager’s personal life. Alcohol consumption or smoking may act as a provoking factor, leading to toxic brain damage. Absence seizures are rare, usually 2-3 paroxysms during the day, which makes timely diagnosis difficult.
Complex forms of absence epilepsy
Complex forms are conditions in which characteristic and repeated actions or manifestations for the patient are noted against the background of complete loss of consciousness. For example, these may be automatic actions characterized by stereotypical alternating or similar movements:
- movements of the eyes, lips or tongue;
- gestures;
- habitual actions brought to automatism, combing, folding clothes or office supplies.
Therefore, paroxysms are difficult to distinguish from ordinary human behavior. Complex absence seizures may also be accompanied by an increase in muscle tone. In this case, the body is pulled back, the pupils are rolled back, and the head is thrown back. In more severe situations, the patient may arch his torso from behind and take a step back to maintain balance. Often, clouding of consciousness occurs against the background of a decline in muscle tone followed by a fall.
With complex myoclonic absences, bilateral rhythmic phenomena of a myoclonic nature are observed, often in the facial muscles and muscles of the upper extremities. Complex seizures require less brain maturity and may occur as early as 4–5 years of age.
Clinical picture of complex attacks:
- duration more than ten seconds;
- an unconscious victim can be moved, and he moves independently;
- a person who has suffered a paroxysm understands that something is happening to him, and additionally notes the fact of clouding of consciousness.
Diagnosis of absence epilepsy
Pathology can manifest itself in the form of a combination of various signs. Seizures may occur with or without loss of consciousness. During the localization of a convulsive attack, muscles twitch, unfamiliar sensations are felt in the body, unconscious influxes of thoughts. Additionally, each age is characterized by certain features of the onset and course of the pathology.
Diagnosis of the disease involves a number of procedures, usually including:
- complete blood count;
- electroencephalography;
- computed tomography;
- magnetic resonance tomography.
The above methods allow the doctor to identify the cause of the disease, as well as determine its type.
One of the most important stages of diagnosis is the initial examination by a doctor. It begins with an analysis of the victim’s complaints; as a rule, the main ones will be:
- clouding of consciousness;
- muscle spasms;
- freezing in place.
By asking clarifying questions, the doctor can find out the frequency of seizures and how they manifest themselves in a particular case.
To make an accurate diagnosis, it is necessary to understand the conditions under which the paroxysm occurred, what symptoms were associated with it, and what happened after it. This information is necessary for differential diagnosis, that is, the process of distinguishing between similar pathologies and filtering out incorrect options. Because the presence of headaches, distortions of perception, and movement disorders can indicate not only illness, but also migraine.
After an oral interview, the doctor proceeds to collecting an anamnesis, which includes:
- information about cases of pathology in close and distant relatives;
- age of onset of seizures;
- and the presence of head injuries or related illnesses.
Already at this stage, the data obtained enable the neurologist to assume the presence or absence of the disease, as well as to outline the direction of the diagnostic process and preferred therapy. However, decisions must also be supported by instrumental and laboratory studies. This will help avoid unintentional mistakes when making a diagnosis.
A blood test is one of the most accessible research methods for many diseases, as it helps to obtain the most accurate data about the state of the human body. Timely identification of various deviations from normal indicators allows effective therapy to begin as soon as possible. The disease can be detected by measuring the amount of electrolytes in the blood plasma. An analysis is also carried out while taking antiepileptic drugs to determine whether the required concentration of the active substance has been achieved.
An electroencephalogram is a harmless diagnostic tool used to evaluate the electrical activity of the brain. The duration of the procedure is from 60 to 90 minutes. During the examination, special electrodes resembling metal circles are placed on the patient's head.
Additionally, a technique is used when an electroencephalogram is performed during sleep. This helps to study the person’s condition in as much detail as possible. The study is carried out not only at the diagnostic stage, but also during the treatment process, to monitor the effectiveness of therapy. If there is a diagnosis, the procedure may be performed more often.
To detect structural disorders of the brain, neuroimaging methods are used:
- computed tomography;
- magnetic resonance tomogram.
These diagnostic procedures are absolutely painless. The most uncomfortable part of the process may be the injection of a contrast agent, which is necessary to ensure that certain areas of tissue are visible in the image as clearly as possible. During the scan, the patient is advised to relax and not make any movements.
Treatment of absence epilepsy
The main emphasis in the treatment of pathological factors is on drug therapy with drugs belonging to the anticonvulsant and antiepileptic group. The selection of medications should be made directly by the attending physician, based on the age of the victim and the frequency of attacks.
If the first remedy has lost its effectiveness, it must be urgently replaced with another. Taking several medications at the same time is allowed only in a situation if their action complements each other.
Prognosis of absence epilepsy
Provided that adequate therapy is used, treatment of the disease is successful. It is impossible to unequivocally answer the question of whether absence epilepsy is curable. Because often, as you grow older, the disease transforms into a stable remission, and does not remind you of itself. Patients with high frequency myoclonic seizures, subnormal intelligence, and resistance to drug therapy have a worse prognosis.
The withdrawal of medications is carried out in stages, only after consultation with a neurologist and with a long period of absence of attacks.