Partial (focal, local) seizures are seizures whose initial, clinical and electrophysiological manifestations indicate the involvement of one or more areas of one cerebral hemisphere in the pathological process.
The incidence of partial epilepsies depending on the anatomical location is:
- epilepsy of the frontal lobe - 30%;
- temporal lobe epilepsy - 60%;
- epilepsy of the parietal lobe - 2%;
- epilepsy of the occipital lobe - 8%.
Simple partial (focal) seizures occur suddenly, last no more than a minute, and are accompanied by symptoms corresponding to the excitation of certain cortical areas against the background of preserved consciousness. The most typical are tonic or clonic contractions of the muscles of half the face, part of a limb, half of the body, adversion of the head and/or eyes to the side, and sudden stop of speech. With a lesion in the mediobasal temporal cortex, olfactory or gustatory hallucinations, sensations of already seen or never seen, already heard or never heard (seizures of impaired perception) occur. Seizures with other psychopathological phenomena are less common: scene-like, auditory and visual hallucinations; ideational (with obsessive thoughts, actions, memories), affective paroxysms (with a sharp change in mood, the appearance of melancholy, anger, fear or bliss, extraordinary lightness, clarity of thoughts).
Complex (complex) partial seizures often begin with gaze fixation, followed by automatism, including repeated steps like stepping on the spot, fussy, swallowing, chewing and other stereotypical movements, snatches of speech that are not related to the circumstances, muttering, and mooing. At the end of automatism, a period of confusion lasting several seconds is noted. Outpatient automatisms are manifested by more complex actions and behavioral reactions that outwardly resemble conscious, purposeful behavior and action (patients continue the activities they have started, consciously answer questions) against the background of a twilight narrowing of consciousness. After the seizure ends, the patient may retain some fragmentary memories of this period. A seizure may occur while consciousness is turned off and subsequent amnesia.
Symptoms of frontal lobe epilepsy
- Motor frontal epilepsy (Jacksonian epilepsy). Occurs with focal hemiclonic seizures with Jacksonian march. More often against the background of preserved consciousness. After an attack, Todd's paresis (Todd's palsy) is possible.
- Dorsolateral epilepsy. It is characterized by focal adversive attacks: adversion of the head and eyes to the side with tonic tension of the arm contralateral to the focus. Often – secondary generalization.
- Opercular frontal epilepsy (posterior parts of the inferior frontal gyrus). Characterized by focal seizures with automotor automatisms. The severity of vegetative phenomena in the structure of attacks (mydriasis, tachycardia, tachypnea).
- Frontopolar frontal epilepsy is manifested by the phenomenon of secondary bilateral synchronization with the formation of “pseudogeneralized seizures.”
- Orbitofrontal frontal epilepsy (anterior parts of the inferior frontal gyrus) is characterized by the appearance of attacks of olfactory hallucinations with or without secondary generalization; focal seizures with hypermotor automatisms.
- Cingular frontal epilepsy (anterior part of the cingulate gyrus) occurs in the form of focal seizures with automotor automatisms; focal attacks, accompanied by a feeling of fear, redness of the face, hyperhidrosis. There is an aura in the form of a feeling of fear.
- Frontal epilepsy with seizures originating from the supplementary motor area (Penfield's supplementary motor area). May be accompanied by unilateral tonic seizures; bilateral asymmetrical tonic seizures (“fencing pose”); hypermotor seizures.
Clinical features of focal seizures originating from the frontal cortex (Luders, 1993):
- sudden onset of attacks (usually without an aura);
- high frequency of attacks with a tendency to be serial;
- cycloleptic course;
- short duration of attacks; minimal post-ictal confusion;
- pronounced motor phenomena (pedaling, chaotic movements, complex gestural automatisms);
- occurs predominantly at night;
- rapid secondary generalization;
- speech impairment (vocalization or stopping of speech);
- bilateral but asymmetrical tonic axial spasms.
Focal seizures originating from the temporal cortex
→ accompanied by various types of aura and automatisms.
Auras observed in temporal lobe epilepsy:
- vegetative-visceral epigastric (unpleasant sensations in the abdominal area with an ascending epileptic sensation);
- mental (for example, the feeling of “already seen”, “already heard”); vegetative (pallor, redness of the face);
- olfactory (Jackson's unbite attacks) – sensation of unpleasant odors (burnt rubber, sulfur);
- intellectual;
- auditory;
- visual – complex visual hallucinations.
Automatisms encountered in focal seizures emanating from the temporal lobe:
- oroalimentary (smacking, chewing movements, licking lips, swallowing movements);
- carpal automatisms (ipsilateral to the lesion),
- ambulatory automatisms;
- verbal automatisms;
- dystonic placement of the hand (contralateral to the lesion);
- typical development of a focal automotor attack, aura (freezing with gaze stopping (staring)), oroalimentary automatisms, hand automatisms and contralateral dystonic positioning of the hand (secondary generalized attack).
Symptoms of temporal lobe epilepsy
- Focal seizures originating from the medial parts (amygdala-hippocampal) of the temporal lobe. Onset occurs in the first 10 years of life in 53% of patients (Engel, 1994). Typical seizures are focal automotor seizures. Most patients experience auras that precede the automotor phase of the attack: epigastric, olfactory, gustatory, and mental. At the beginning of the disease, auras may be isolated. The duration of attacks is 1-2 minutes.
- Focal seizures originating from the neocortex of the temporal lobe. They debut at the age of 10 to 50 years and can manifest themselves as auditory hallucinations (unpleasant voices, sounds), visual hallucinations (complex visual images), attacks of sensory aphasia, focal automotor seizures, “temporal syncope” - attacks with a slow switching off of consciousness, “limping” , falling without convulsions. Temporal syncope begins with an aura (usually dizziness) or occurs in isolation. Characterized by a relatively slow loss of consciousness followed by “losing” and falling (not a sharp fall). There may be slight tonic tension in the muscles of the limbs and facial muscles; the appearance of oroalimentary or gestural automatisms. More often develop with unilateral temporal lobe epilepsy. Their appearance indicates the spread of excitation to the reticular formation of the brain stem. This type of attack should be differentiated from non-epileptic fainting, in which provoking factors are identified (prolonged immobile vertical position, stuffiness) and lipothymia preceding the attacks.
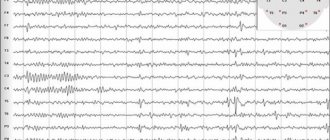
- Benign focal epilepsy of childhood with central temporal peaks (rolandic). Debuts at the age of 2-12 years with two peaks - at 3 and 9 years. Boys get sick more often. Typically, the presence of short hemifacial and pharyngo-brachial attacks (frontal localization of the source of irritation), which are preceded by paresthesia in the mouth and pharynx (temporal localization of the source of irritation). Vocalization, speech arrest, dysarthria, hypersalivation, and guttural sounds are observed. The attacks, usually simple focal and secondary generalized, often occur at night. Frequency – 1 time per month. The EEG shows “rolandic” peak-wave complexes, mainly in the central temporal leads. Treatment: valproate 20-40 mg/kg/day, carbamazepine 10-20 mg/kg/day.
- Primary reading epilepsy. The age of manifestation is puberty. Seizures develop during reading, especially long reading and aloud. Clinically manifested by myoclonus of the masticatory muscles, jaw clonia, sensory disturbances in the form of a blurred image. EEG shows spike-wave complexes in the temporo-parietal parts of the dominant hemisphere, generalized spike-wave complexes at the time of an attack.
- Epileptic aphasia syndrome (Landau-Kleffner). Manifestation – 3-7 years. In 1/3 of cases it proceeds without seizures, and the diagnosis is made on the basis of EEG. The main syndrome is aphasia, starting with verbal agnosia, transition to paraphasia, perseveration, stereotypy with loss of expressive speech. Combined with partial or generalized tonic-clonic seizures. Often interpreted as deaf-muteness in a child. EEG outside a seizure - continuous irregular (1-3.5 Hz, 200-500 μV) spike-wave complexes, spikes, sharp waves in the temporal leads. Treatment: sulthiam (ospolot) 5-15 mg/kg/day, clobazam (Frisium) 0.3-1 mg/kg/day, valproate, ACTH.
- Chronic progressive epilepsy of childhood (Kozhevnikov syndrome), Epilepsiapartialiscontinue. Presented with continuous partial seizures (temporo-frontal localization of the source of irritation). It is divided into: a) Kozhevnikov’s epilepsy; b) Rasmussen's syndrome.
Read also Ischemic stroke - causes, symptoms, treatment
a) Kozhevnikov epilepsy is a partial non-progressive rolandic epilepsy in children or adults associated with damage to the motor cortex. The seizures last for days or years. Clinically – focal motor attacks in the form of rhythmic contractions of agonists and antagonists in a limited area, continuing during sleep and intensifying with movement and stress. Secondary generalization of the seizure is possible. The EEG shows epi-discharges in the rolandic area contralateral to convulsive manifestations against a relatively normal background. Treatment: carbamazepine, valproate, benzodiazepines, neurosurgical methods.
b) Rasmussen syndrome is a chronic progressive symptomatic epilepsy, identical in type to the myoclonic manifestations of Kozhevnikov’s epilepsy, but occurring more often in childhood: the age of manifestation is 2-14 years (average age is 7 years). Clinically manifested by focal motor seizures followed by constant myoclonus, often during sleep. Generalization possible. Hemiparesis, dysarthria, dysphasia, hemianopsia, and mental retardation increase. EEG shows diffuse slow waves with a predominance in the hemisphere contralateral to neurological manifestations, multifocal high-amplitude spikes, sharp waves, spike-wave.
Diagnostics
A patient with a first-time partial attack should be carefully examined. It is necessary to exclude cerebral pathologies: vascular malformations, tumors, cortical dysplasia. The neurologist collects anamnesis. Finds out the frequency, sequence, duration of an epileptic attack. Clarifies the neurological status. With the symptomatic nature of FE, it helps to establish the approximate localization of the source of excitation.
Instrumental diagnostics include:
- Electroencephalography. This form of epilepsy is recorded even during the interictal period. If the information content of a regular EEG is low, an examination with provocative tests and testing at the time of an attack is indicated.
- Subdural corticography allows you to establish the exact localization of the affected area.
- MRI helps to identify the morphological substrate. To diagnose the slightest structural changes, a minimum thickness of sections is required. With symptomatic FE, it is possible to establish the underlying disease and note dysplastic transformations. If there are no abnormalities during magnetic resonance imaging, cryptogenic or idiopathic focal epilepsy is diagnosed.
- PET of the brain helps to identify the area of hypometabolism in cerebral tissue corresponding to the lesion.
- Area SPECT examines the area of hyperdiffusion during attacks and hypoperfusion in the interictal period.
Symptoms of parietal epilepsy
- debut in a wide age range;
- at the beginning of the disease, isolated somatosensory auras are characteristic, as a rule, against the background of preserved consciousness;
- somatosensory auras;
- elementary paresthesia (numbness, tingling, “crawling” sensation);
- pain (sudden throbbing pain in one limb, often spreading like a Jacksonian march);
- disturbance of temperature perception (burning or cold sensation);
- “sexual” attacks (unpleasant sensations of numbness, tingling in the genital area);
- ideomotor apraxia (feeling of impossibility of movement in the limbs);
- violation of the body diagram.
Symptoms of occipital epilepsy
- debut in a wide age range;
- characterized by simple partial attacks (auras): simple visual, hallucinations, paroxysmal amaurosis, paroxysmal disturbances of visual fields, subjective sensations in the area of the eyeballs; deviation of the head and eyes with oculoclonus (usually contralateral to the lesion); autonomic disorders (headache, vomiting, pale face);
- a common symptom is post-attack migraine-like headache; Often there is a spread of epileptic activity to the temporal and frontal regions with the addition of motor or automotor seizures.
Early-onset benign occipital epilepsy (Panayotopoulos type) is characterized by the fact that 2/3 of all seizures occur during sleep. In the same patient, attacks can occur both during the day and at night. Seizures are an unusual combination of autonomic symptoms (most often nausea, retching and vomiting), behavioral changes, lateral deviation of the eyes, and other more familiar manifestations of an epileptic seizure.
During an attack, the child complains of lightheadedness and poor health. At this moment, as a rule, the child feels nauseous, pale, and has excessive sweating and hypersalivation. Headache is common. Vomiting may begin 1-5 minutes after the first symptoms appear. Nausea ends with vomiting in 74% of all cases. The frequency of vomiting can be different: in some children the vomiting is one-time, in others it is repeated, observed over several hours and leading to dehydration. Other vegetative symptoms are also possible: mydriasis or miosis (respectively, dilation or constriction of the pupils); disorders of the respiratory system (irregular breathing, short-term apnea), cardiovascular system (tachycardia); cough; urinary and fecal incontinence; changes in intestinal motor functions; increase in body temperature, both at the beginning of the attack and after it.
Along with vomiting, eye deviation is a very common attack syndrome. Averting the eyes to the extreme lateral position can be accompanied by turning the head in the same direction and lasts from several minutes to several hours. Deviation of the eyes can be either constant or intermittent - the eyes are either moved to the side or brought back to their original position.
The degree of impairment of consciousness may vary; sometimes the child partially follows instructions. The child either suddenly or gradually becomes disoriented in time and space and does not respond to his surroundings. The severity of the disturbance of consciousness increases as the symptoms of the attack unfold. In approximately 20% of all cases, the child loses consciousness and “goes limp,” and motor epileptic manifestations are not always observed. The condition resembles cardiogenic syncope). In 20% of children, the attack ends with hemiconvulsions, sometimes with a Jacksonian march.
In some cases, symptoms reminiscent of an attack of rolandic epilepsy are observed - speech arrest, hemifacial spasm and oro-pharyngolaryngeal movements. In a small percentage of cases (6% according to Covanis et al., 2005), blindness, visual hallucinations or illusions may occur. Visual symptoms usually occur after the development of autonomic symptoms.
Read also Epileptic encephalopathies - symptoms, syndromes, treatment
On interictal EEG, in 90% of cases, an acute-slow wave complex is recorded, usually multifocal and of large amplitude. The morphology of spikes is the same as in Rolandic epilepsy. The localization of complexes can be very different (all parts of the brain can be involved), although the greatest severity of epileptic changes is observed in the posterior parts of the brain. Most often, spikes are observed in the occipital leads, a little less often in the frontal leads, and even less often in the temporal leads. In 17% of all cases, adhesions are recorded in the vertex leads.
Despite the high incidence of vegetative status epilepticus, Panagiotopoulos syndrome is considered a prognostically favorable condition. The duration of epileptic seizures is short, on average 1-2 years. However, individual patients have been described who experienced attacks for 7 years.
Emergency care: administration of benzodiazepines intravenously (0.2-0.3 mg/kg per day) or rectally (0.5 mg/kg per day) is indicated. Prophylactic use of antiepileptic drugs is not carried out due to the fact that seizures can be very rare and the duration of their existence in a child is not very long.
Reflex (stimulus-sensitive) epilepsies are epileptic seizures that occur under the influence of external environmental factors: simple (photo and color stimulation, sharp sudden external influences, laughter, eating food) and complex (reading, listening to musical compositions, mental operations) sensory stimuli. The latter lead to the appearance of foci of excitation in the corresponding sensory systems, forming excessive responses at various levels of the brain in the form of hypersynchronous neuronal discharges.
- Photosensitive epilepsy. It is provoked by flickering light, watching TV, working on a computer, bright saturated colors, “striped” objects (black and white striped wallpaper, escalator steps, etc.), rapid opening and closing of the eyes, fluttering of the eyelids. It manifests itself in various types of seizures: myoclonic, absence, absence with eyelid myoclonus, generalized tonic-clonic, simple and complex partial. Treatment: valproate, lamotrigine, levetiracetam, topiramate.
- Seizures caused by thinking (thinking epilepsy). They are provoked by mental operations: arithmetic calculations, playing chess or cards, solving test tasks. They occur in the form of myoclonic, absence, and generalized tonic-clonic seizures. Treatment: valproate, phenobarbital, clonazepam, clobazam.
- Seizures caused by fear (startle epilepsy). They are provoked by fear, sudden external influence (sound, touch). They occur in the form of simple (fencer’s pose with rotation of the body) and complex partial seizures with paresthesia, sensations of “already seen,” paroxysmal dyskinesias, often accompanied by vocalisms. Treatment: carbamazepine, phenobarbital, valproate, clonazepam, levetiracetam. This form of epilepsy must be differentiated from hyperexlexia (startle syndrome) - a hereditarily predisposed pathological increase in the reaction to fear.
- Seizures caused by sound (sound epilepsy). They are provoked by listening to (or even remembering) a certain piece of music or fragment. Occurs in the form of complex partial seizures (derealization).
- Walking epilepsy. Provoked by walking. It occurs in myoclonic and clonic generalized seizures.
- Reading epilepsy. It is provoked by reading an incomprehensible, complex text, for example, in a foreign language. Manifests itself in partial, myoclonic, and less commonly generalized tonic-clonic seizures. Treatment: valproate, clonazepam.
- Epilepsy of food. It is provoked by dense food, the sight, smell of food or a certain type of food (soups, hot dishes). It manifests itself as complex partial (with automatisms, dysphoria, vegetative aura) attacks. A transition to generalized tonic-clonic seizures is possible. Treatment: carbamazepine, phenobarbital.
- Epilepsy provoked by laughter. It occurs in the form of generalized tonic-clonic seizures, astatic (atonic) seizures, and is provoked by laughter adequate to the situation. This form of epilepsy must be differentiated from epilepsy of laughter (gelastic epilepsy), which is characterized by the development of attacks of unmotivated violent laughter.
When treating all forms of reflex (stimulant) epilepsy, it is necessary to avoid specific situations that provoke a seizure, use anticonvulsants according to the type of seizure, and conduct psycho-behavioral therapy.
What it is
Epilepsy is a chronic neurological disease that is characterized by an increased susceptibility of the body to the occurrence of epileptic seizures. Epilepsy is one of the most common pathologies of the central nervous system; among adults and children, the prevalence of the disease is approximately 50–100 cases per 100 thousand population.
Depending on the etiology, there are 3 forms of pathology:
Cryptogenic epilepsy is a disease of unknown etiology, that is, the cause of the development of the disease is not clear and has not been identified. The diagnosis is established only after excluding other forms.
For some reason, there is a predisposition of brain cells to form excessive paroxysmal discharge. Such a discharge disrupts the normal functioning of neurons, which leads to clinical manifestations of epilepsy - loss of consciousness, convulsions, sensory and autonomic disorders.
In the cryptogenic form of the disease, focal changes are more often detected. The focus of excessive activity may be localized in the frontal, temporal, parietal or occipital lobe. Less commonly, the discharge spreads to both hemispheres of the brain.
Provoking factors
Most neurologists believe that the cause of partial epilepsy can be a complex of different factors. The main reason is considered to be genetic predisposition. That is why the first symptoms of the disease appear in childhood or adolescence.
The following factors can cause partial seizures of epilepsy:
- neoplasms that have appeared in the brain (they can be either benign or malignant);
- abscesses, hematomas, cysts;
- all kinds of vascular changes: malformations, aneurysms;
- disruption of the blood circulation of the brain (for example, with stroke, ischemia and other pathologies);
- penetration of neuroinfection (syphilis, encephalitis, meningitis, etc.);
- congenital pathological changes in the nervous system;
- various head injuries.
These factors can trigger the onset of epilepsy or worsen seizures. Under the influence of any of the listed factors in a certain area of the brain, neurons begin to send pathological signals with altered intensity.
Over time, this negatively affects all the cells that surround the pathological area. This provokes the development of epileptic seizures.
Classification
There are three forms of focal epilepsy:
- Idiopathic. Develops against the background of absence of changes in the central nervous system. It is caused by genetically determined membrane and channelopathies, disorders of the maturation of the cerebral cortex. This pathology is benign. These are Panagiotopoulos syndrome, Rolandic epilepsy, Gastaut childhood occipital epilepsy and infantile episyndromes.
- Sympathetic. It is characterized by the presence of a cause. Morphological changes in most cases are visualized on tomography.
- Cryptogenic. It is secondary in nature, but morphological changes are not detected by neuroimaging. Another name for this type of FE is probably sympathetic.
Localization of the disorder in the brain area
The classification of partial epilepsy is based on identifying an area in the brain with increased activity during an attack. By the way, the picture of a particular seizure will largely be determined by the location of the focus of pathological excitability of neurons.
Possible localization of the outbreak:
- Temporal . This is the most common type of partial epilepsy (about 50% of all cases of the disease are provoked by the pathological activity of neurons in the temporal zone).
- Frontal . It deservedly ranks second in frequency of cases (24-27%).
- Occipital (about 10% of all patients with this form of epilepsy).
- Parietal . Occurs least often (1%).
How to determine the exact location of the outbreak? Now this is very easy to do. An EEG (electroencephalogram) will help.
Diagnosis is most often carried out while the patient is at rest or asleep (polysomnography). But the most accurate result is given by an EEG directly during the next attack. It is almost impossible to wait for it. Therefore, an attack is provoked by the introduction of special drugs.
Causes of cryptogenic focal epilepsy
Cryptogenic focal epilepsy is a form of the disease characterized by uncertain or unknown causes. The disease is diagnosed in situations where the symptoms do not fit other types. Often it is not possible to determine the cause of the disease even after all possible tests have been carried out.
According to researchers, the main factors of occurrence are:
- hereditary predisposition;
- poisoning with toxic substances;
- history of viral infections;
- sudden exposure of a person to a bright flashing light, a sharp sound, or a strong temperature change.
It is worth noting that in other forms, a focus of pathological activity is observed in the cerebral cortex in an area where in a normal situation it should not be. But with the cryptogenic form, there is no obvious localization of the lesion.
Types of attacks and their symptoms
Partial epilepsy in each patient manifests itself in purely individual attacks. But there is an accepted classification of their main types. In simple partial attacks, the patient’s consciousness is retained completely or partially. This condition has different forms of manifestation:
- one can observe not very intense contractions of the muscles of the legs, arms, facial muscles, the patient feels numbness, tingling, so-called “goosebumps” on his skin;
- the patient turns his eyes, head, and sometimes his entire body in a certain direction;
- there is drooling;
- the patient performs chewing movements and grimaces;
- the speech process stops;
- pain appears in the epigastric area, heartburn, heaviness, peristalsis increases, flatulence appears;
- hallucinations may be observed: gustatory, olfactory, visual.
Read also Alzheimer's disease - causes, symptoms, treatment
About a third of patients experience complex partial seizures, in which the person loses consciousness. Such patients are often fully aware of what is happening, but are not able to speak or answer the questions posed.
Often after another attack the patient experiences amnesia. He forgets everything that happened.
It often happens that epilepsy begins with a partial form, and then both hemispheres of the brain suffer. This becomes the cause of the development of a secondary seizure, generalized. It often makes itself felt in the form of severe cramps.
Symptoms of complex partial seizures:
- The patient develops severe anxiety and fear of death .
- He concentrates on the events that happened or the words he heard , and experiences strong feelings because of them.
- The patient begins to perceive a completely familiar environment as unfamiliar to him. Or maybe, on the contrary, you are haunted by a feeling of “déjà vu” .
- The patient perceives what is happening as something unreal . He may perceive himself as the hero of a book, a movie he has seen, or even observes himself as if from the outside.
- Automatisms . These are certain obsessive movements. What specific movement a patient will experience depends on which area of his brain is affected.
- In the short periods between seizures, a person at the initial stage of development of partial epilepsy feels quite normal. But over time, symptoms of brain hypoxia or underlying pathology become more and more apparent . Headaches, sclerosis appear, personality changes, dementia (dementia) is observed.
Let us consider the manifestation of each type of disease in more detail.
How to treat pathology
Treatment for epilepsy should be selected by a doctor after a final diagnosis has been made. The difficulty of treating the cryptogenic form lies in the fact that the cause of the disease could not be identified; therefore, etiotropic methods are not used. The basis of therapy is the use of antiepileptic drugs.
The choice of medication primarily depends on the type of seizure; the patient’s age and the presence of concomitant diseases are also taken into account.
The main antiepileptic drugs are valproic acid derivatives (valproates) and carbamazepine. Valproates are a universal remedy; they can be used to treat any seizures, carbamazepine - for partial ones.
Modern antiepileptic drugs include lamotrigine, topiramate, levetiracetam, clonazepam, etc.
What drugs are prescribed
Generalized tonic-clonic, tonic, clonic
The drugs of choice for generalized epilepsy are valproate and lamotrigine. If ineffective, topiramate and pregabalin may be prescribed.
Valproate, topiramate, and levetiracetam are used to treat myoclonic seizures.
The main drug used to treat absence seizures is valproic acid. Less commonly prescribed are lamotrigine, clonazepam, and levetiracetam.
To treat partial seizures, valproate, carbamazepine, as well as modern drugs - topiramate, levetiracetam, lamotrigine can be used.
Treatment begins with taking one drug; if it is ineffective or side effects occur, it is changed. Only a doctor can prescribe or change antiepileptic therapy; direct treatment is carried out at home (with the exception of severe generalized seizures, the development of status epilepticus).
Damage to the frontal lobes of the brain
Partial epilepsy in the frontal lobes has characteristic symptoms:
- simple seizures;
- complex seizures;
- secondary generalized paroxysms;
- a combination of these attacks.
Seizures last for 30-60 seconds and are often repeated. You can observe their seriality. They often happen at night. In 50% of patients, the seizure begins without an aura before it begins.
Frontal lobe epilepsy has its own characteristics:
- seizures are quite short-lived (up to 1 minute);
- after the end of complex attacks there is a minimum of confusion;
- secondary attacks occur very quickly;
- motor disturbances can often be observed (uncharacteristic automatic gestures, trampling in one place);
- at the beginning of a seizure, automatisms are very common;
- the patient often falls.
Forms of frontal lobe epilepsy:
- Motor . It manifests itself in the form of convulsions in the limbs, an aura before an attack, Todd's paralysis may occur, and secondary generalization often occurs.
- Anterior (frontopolar) . It manifests itself in the form of painful memories, the sense of time changes, thoughts come flooding in, and memory lapses often occur.
- Cingular . Characterized by hyperemia of the facial area, increased motor skills, blinking, and a state of passion.
- Dorsolateral . The patient turns his eyes, head and even torso in one direction, loses the ability to speak during the attack, and secondary generalization often occurs.
- Orbitofrontal.
- Opercular.
- Additional motor area.
The first signs of cryptogenic focal epilepsy
The main sign of pathology is the observation of seizures. They come in different types, mainly divided into two groups:
With focal cryptogenic epilepsy, it is partial, that is, partial, seizures that are most often observed. In most situations, the approach of an attack is accompanied by a so-called aura - this is a symptom signaling the imminent onset of a seizure. By its appearance, one can determine the localization of focal lesions in the victim’s cerebral cortex.
With a motor aura, the patient begins to make sudden, unexpected movements, this signals that the affected area is located in one of the frontal lobes of the brain. When a patient's vision or hearing deteriorates, the disorder occurs in the occipital or temporal lobe.
The appearance of an aura in itself is a partial seizure.
Temporal form of the disorder
Temporal partial epilepsy manifests itself in the following seizures:
- simple;
- complex;
- secondary generalized;
- their combinations.
Very often, with the temporal form, complex partial seizures with automatisms and upset consciousness are observed.
Very often, before attacks in the case of the temporal form, the patient feels an aura:
- olfactory;
- taste;
- visual;
- somatosensory;
- vegetative-visceral;
- auditory;
- mental.
Types of temporal lobe epilepsy:
- Paleocortical . The patient may freeze with a completely motionless face, his eyes remain wide open, directed at one point. There is a feeling that he is simply “staring” at something. Consciousness may turn off, but motor activity may remain. For example, the patient may be fiddling with his buttons on his clothes. Often the patient can simply fall without the appearance of convulsions (temporal syncope).
- Lateral . During seizures, speech, vision, and hearing are impaired, and auditory and visual hallucinations appear.
Patients with occipital epilepsy suffer from visual hallucinations, impaired visual field, discomfort in the eyeballs, curvature (deviation) of the neck, and they experience frequent blinking.
Treatment of seizures
Medication
The main drugs in the treatment of epilepsy are anticonvulsants. They are prescribed only by a doctor . He selects the dosage and frequency of administration.
If seizures stop during drug therapy, this does not mean that the person has recovered. The disease remains, the negative symptoms simply go away.
The following drugs are used to treat the disease.
Anticonvulsants:
- Lamotrigine;
- Carbamazepine;
- Depakine;
- Trileptal;
- Valporates;
- Sedalite.
Medicines relieve seizures, prevent seizures, and stabilize mood.
Tranquilizers:
- Clonozepam;
- Phenazepam;
- Lorafen.
The drugs soothe, relax muscles, and have an anti-anxiety effect.
Neuroleptics:
- Aminazine;
- Truxal;
- Haloperidol.
The drugs suppress the nervous system and can reduce the convulsive reaction.
Nootropics:
- Piracetam;
- Phezam;
- Picamelon;
- Mexidol.
They have a beneficial effect on metabolism in the brain, restore its proper functioning, improve blood circulation, and help increase intelligence.
Surgery
If drug therapy does not produce positive results, surgery may be prescribed.
There are several methods of surgical treatment:
- Removal of formation. The method is used if the cause is a tumor or hematoma. After their removal, the person recovers.
- Lobectomy . During the operation, the part of the brain that causes the pathological lesions is removed. Most often, the operation is used to excise the temporal lobe.
- Callesotomy . The two halves of the brain are dissected. The operation is indicated for patients with severe forms of the disease.
- Vagus nerve stimulator. A miniature device is sewn under the skin, which sends impulses to the vagus nerve, bringing the foci of excitation to a calm state.
What is cryptogenic focal epilepsy
Cryptogenic epilepsy is one of the most complex chronic diseases of the nervous system. This form of pathology is diagnosed in every second patient who presents with symptoms. In turn, it is divided into separate subspecies:
- partial;
- temporal;
- generalized;
- focal.
The disease is dangerous because it is practically untreatable, so it requires long-term, and in most cases, lifelong treatment.
Epilepsy is a chronic neurological disease, which is characterized by a high predisposition of the victim’s body to the occurrence of epileptic seizures, and is one of the most common pathologies of the central nervous system.
Depending on the etiology, there are three separate forms of epilepsy:
- symptomatic;
- idiopathic;
- cryptogenic.
The latter is a disease with an unknown etiology, when the cause of the onset and development of the disease is unknown. A doctor can make a diagnosis only after other forms of epilepsy have been ruled out.
The disease occurs due to any predisposition of brain cells to the formation of paroxysmal discharge. This discharge disrupts the proper formation of neurons, which leads to the following clinical manifestations:
- loss of consciousness;
- convulsions;
- muscle spasms;
- sensitivity disorders;
- disturbances in the functioning of the autonomic system.
Pathology reveals focal changes, the localization of which changes. The focus of increased activity may occur in the temporal, occipital, parietal or frontal zone. In a more rare case, a discharge can form in both hemispheres of the brain at the same time.
In recent years, doctors have noted an increase in the incidence of epilepsy. The exact causes of this disease have not yet been established. It is known that about 4-10 people per 1000 people suffer from seizures. Drug-resistant cryptogenic epilepsy is considered one of the most severe forms of the disease. It is difficult to select treatment for this species due to drug resistance.
A qualified team of doctors at the Yusupov Hospital takes on complex cases. Diagnosis of epilepsy in our clinic is carried out using modern medical equipment. European CT, MRI and EEG equipment are used for examination. They allow you to determine the location of the pathological focus with high accuracy. An analysis of blood and the degree of resistance of the body to drugs is carried out in a modern laboratory.
Therapy for cryptogenic epilepsy is carefully developed by experienced neurologists and epileptologists. In this case, an individual approach is used. Drugs are selected taking into account the degree of drug resistance and other associated conditions. The prescribed medications meet the latest European standards for the treatment of epilepsy.
First aid
If a person has a seizure, the following steps must be taken:
- Lay it down carefully.
- Raise your head slightly.
- If the person's mouth is open, insert a handkerchief or something tight to prevent him from biting his tongue.
- Turn your head slightly so that the person does not choke on saliva or vomit.
After the attack ends, help the person stand up and hold him until he is completely back to normal. Usually, immediately after an attack, complete normalization of the condition occurs.
Prognosis and prevention
Partial epilepsy is difficult to treat. Most often, the patient is prescribed lifelong drug therapy.
During the stabilization of the condition, the doctor may prescribe a course of anticonvulsants for preventive purposes. This disease is characterized by relapses even with complex drug therapy.
Therefore it is important:
- carry out regular examinations;
- take prescribed medications;
- to refuse from bad habits;
- avoid places with flashing special effects;
- limit physical activity;
- avoid stress;
- limit fluid intake;
- monitor your diet.
Partial epilepsy is a serious disease that should not be treated with disdain. At the first signs of illness, it is important to consult a doctor in a timely manner to select adequate drug therapy. Self-medication is strictly prohibited.
Prognosis of cryptogenic focal epilepsy
The prognosis of the cryptogenic form of the disease depends simultaneously on many factors:
- ongoing therapy;
- type and frequency of attacks;
- duration of the disease.
If the patient receives adequate treatment, the prognosis is favorable. Otherwise, prolonged and frequent seizures can lead to epileptic encephalopathy. In particularly severe situations, an attack can result in head damage during a fall or asphyxia.
To prevent recurrent attacks, it is necessary to carefully follow the treatment plan, completely eliminate the use of alcohol, overwork, stressful situations and lack of sleep.
Cryptogenic epilepsy is the most common form of the disease, occurring in approximately every second patient. A characteristic feature of the cryptogenic form is that it is impossible to establish the cause of the disease. The unknown etiology creates certain difficulties in selecting treatment; the basis of therapy for such patients is anticonvulsants.