In modern diagnosis of various neurological diseases, electroencephalographic monitoring is the main method for studying epileptic activity. In patients with epilepsy, certain waves of oscillations are recorded that characterize epileptiform activity.
For the most accurate diagnosis, it is better to conduct the study during an exacerbation, however, epileptiform activity is recorded on the EEG also in the interictal period with the appearance of pathological waves, or wave complexes, that differ from the background activity.
These can be sharp waves, single peaks or flashes that last literally a few seconds. For a clear diagnosis of the disease epilepsy, this form of wave activity is not an absolute basis.
The concept of “epileptic activity”
This term is used in two cases:
- Registration of epileptiform phenomena on the EEG during a seizure (psychomotor seizure pattern or ongoing polyspike). The activity may not contain epileptic seizure patterns.
- In the case of a clear activity schedule. Can be recorded outside of an attack .
Hereditary EEG patterns may be associated with epileptic seizures. Some specific combinations have different epileptic syndromes.
The presence of epileptiform activity and epileptic seizure patterns on the EEG, high-amplitude bursts of activity (more than 150 μV) are important signs of the presence of epilepsy.
EEG patterns
EEG patterns in clinical epileptology
The most studied patterns:
- focal benign sharp waves (FOW);
- photoparoxysmal reaction (PPR);
- generalized spike waves (during hyperventilation and at rest).
FOV is more often registered in childhood, between 4 and 10 years, and FPR in children under 15-16 years of age.
With FOV, the following negative deviations are observed:
- mental retardation;
- febrile seizures;
- development of Rolandic epilepsy;
- partial epilepsy;
- mental disorders;
- speech disorders;
- various functional disorders.
Develops in approximately 9%.
In the presence of FPR, the following are revealed:
- photogenic epilepsy;
- symptomatic partial epilepsy;
- idiopathic partial epilepsy;
- febrile seizures.
FPR is also observed with migraines, dizziness, syncope, and anorexia.
Generalized spike waves
The frequency of FGPs is observed in children under 16 years of age. They also occur very often in healthy children, in about 3% of cases under the age of 8 years.
Associated with primary generalized idiopathic epileptic conditions, for example: Govers-Hopkins or Herpin-Jantz syndrome, Calp's pycnolepsy.
What can be seen on the EEG with different forms of epilepsy?
Each type of this pathology is characterized by its own clinical symptoms. In addition, epilepsy looks different on the EEG.
Benign rolandic epilepsy:
- During an attack (exacerbation), a focal epileptic discharge is noted in the middle temporal and central leads. It looks like high-amplitude spikes, in addition to which a combination of sharp and slow waves is observed. Exit beyond the boundaries of the original location is noted.
- In the absence of an attack, focal spikes are often recorded, combining waves that arise simultaneously in several leads. Often, epileptic activity on the EEG does not manifest itself in any way during the daytime while the person is awake. In this case, it necessarily appears as soon as the person falls asleep.
Rolandic epilepsy is the most common form of childhood epilepsy
Epilepsy form Panagiotopoulos:
- During an exacerbation, an epi-discharge is recorded - high-amplitude spikes, combined with slow and sharp waves that rarely remain within the initial localization.
- At rest, multifocal low- or high-amplitude complexes can most often be seen. It is characteristic that the complexes arise serially - at the moment of closing the eyes, and at the moment of opening they are blocked. An attack can be triggered by photostimulation.
Generalized idiopathic epilepsies
EEG patterns can be more often observed in a child and in juvenile epilepsy with absence seizures:
- During an exacerbation, the equipment can show an extensive discharge in the form of rhythmic activity in excess of 10 Hz with a steadily increasing character, as well as sharp waves and high-amplitude delta and theta waves. They are unstable and asymmetrical.
- Outside of an exacerbation, the EEG picture may remain standard, with uncharacteristic activity occasionally present.
Typical absence seizures are short, generalized epileptic seizures with sudden onset and termination.
Early infantile epileptic encephalopathy:
- An exacerbation causes an increase in the number and amplitudes of the spike in combination with sharp waves.
- Outside the exacerbation, there is extensive activity, where the outbreak is followed by its disappearance. Possible hypsarrhythmia.
Lennox-Gastaut syndrome:
- An exacerbation is characterized by the occurrence of numerous spikes and sharp waves; a “spike-slow wave” combination can be recorded. Desynchronization develops.
- Outside of exacerbation - hypersynchronous activity accompanied by sharp waves, spike-slow wave complexes, focal disorders.
Lennox-Gastaut syndrome is a severe form of epilepsy that begins in childhood
Seizure patterns can also be recorded in phenotypically healthy patients. In this case, a diagnosis of epilepsy is not made, but it is believed that such people have a genetic predisposition to this pathology. As a rule, periodic examination is recommended.
Basis of epileptiform activity
At the basis of epileptiform activity at the cellular level, a paroxysmal displacement of the membrane occurs, which causes a burst of action potentials. They are followed by a long period of hyperpolarization.
This action occurs regardless of what kind of epileptiform activity is recorded, focal or generalized.
Each of these patterns can also be observed in phenotypically healthy people. The presence of these patterns is not a clear basis for diagnosing epilepsy, but does indicate the possibility of a genetic predisposition.
In some patients, epileptiform activity is recorded only during sleep. It can be triggered by certain stressful situations or the behavior of the person himself.
To clearly determine the pathology, you can provoke an attack with special stimuli. If the patient is subjected to rhythmic light stimulation during sleep, it is possible to detect the presence of epileptiform discharges and patterns of epileptic seizures.
To generate epileptiform activity, it is necessary to involve a huge number of nerve cells – neurons.
There are 2 types of neurons that play an important role in this process:
- 1 type of neurons – “epileptic” neurons . PD flashes are issued autonomously;
- Type 2 – surrounding neurons . They are under afferent control, but can be involved in the process.
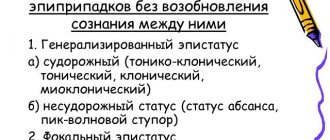
There are some exceptions to severe epileptic activity that occurs without seizures but reaches the level of status epilepticus.
These include:
- Landau-Kleffner syndrome;
- ESES;
- various non-convulsive epileptic encephalopathies.
How is the diagnosis of epilepsy confirmed?
The only reliable signs of the disease are epileptiform activity on the EEG and seizure patterns. As a rule, high-amplitude bursts of brain waves are recorded at the same time, but they cannot accurately indicate pathology. An EEG is necessarily prescribed to confirm the diagnosis, since epileptic discharges can be recorded outside of a seizure. In addition, the study allows you to accurately determine the form of the disease, which helps prescribe adequate treatment.
Epiactivity on the EEG in a child without seizures can be determined in various ways. Most often, rhythmic light provocation is used to stimulate epiactivity, but hyperventilation or other additional techniques can be used. Sometimes cases of epiactivity can be detected only during prolonged EEG recording, often performed during night deprivation sleep. Only a small proportion of patients cannot confirm the diagnosis with such a study.
Diagnosis process
For a high-quality diagnosis, it is necessary to take into account epileptiform changes when analyzing the EEG in conjunction with clinical manifestations and anamnesis data.
It is important to remember that an electroencephalogram is of great value for diagnosis if done specifically during a patient’s seizures.
The diagnostic value in the period between attacks is low. In patients with neurological diseases and in patients with nonepileptic seizures, epileptiform activity is detected in 40% of cases.
The term “epileptic change on the EEG” itself is becoming a thing of the past today, as it is directly related to the disease.
And the term “Epileptoid activity” misleads the doctor and leads to errors in diagnosis due to the prefix “epi”. There are either changes in the EEG or not, there is no choice, so it is important to strictly adhere to the generally accepted rules of medical terminology in order to avoid serious consequences for the patient.
Diagnostics
A conversation with the patient and finding out the history of the disease is an important stage of the diagnostic process.
When diagnosing epilepsy, the classification of epilepsies and episyndromes, developed back in 1989 by the International League Against Epilepsy, is used. The division is based on the cause of seizures. From this point of view, all types of epilepsy and episyndromes (both local and generalized) are divided into:
- idiopathic - this group includes all episyndromes with a hereditary predisposition. Similar clinical symptoms can be identified in the patient's relatives. At the same time, a full clinical examination and the use of additional research methods do not reveal signs of primary brain damage (i.e., at the onset of the disease, nothing is found in the brain that could provoke an epileptic seizure. Despite this, epileptic seizures still appear);
- symptomatic - this includes those situations when the appearance of epileptic seizures is caused by brain damage or the presence of some disease in the body as a whole. For example, previous severe traumatic brain injuries or neuroinfections, metabolic disorders;
- cryptogenic - this group includes those episyndromes that are probably symptomatic, but it was not possible to detect their cause using modern diagnostic methods. Cryptogenic epilepsy is a diagnosis that prompts further search for the cause of the disease.
Why is the reason so important? Because treatment tactics fundamentally depend on it. If the cause of epilepsy is known, then, if possible, it should be eliminated. Sometimes only eliminating the factor that caused the episyndrome can reduce the frequency of attacks or even eliminate them. When the cause remains unknown, when prescribing treatment, they rely on the type of epileptic seizure (local or generalized) that occurred in the patient.
To determine the type of seizure, the doctor must carefully collect an anamnesis of the disease. Even the smallest details are important. Did the patient anticipate the attack? What sensations did he experience during and after the seizure? What does the patient think triggered the seizure? How often do such conditions occur? And much more should be found out by the doctor. Since during most seizures the patient cannot remember his feelings, information from relatives and colleagues who were present during the development of the seizure can be helpful.
After clarifying complaints and medical history, a neurological examination is performed. At the same time, epilepsy is characterized by an interesting feature: in most cases, at the onset of the disease, the neurologist does not find any gross neurological changes. This, oddly enough, serves as little evidence in favor of the diagnosis of epilepsy.
To accurately establish the nature of the seizure, exclude other diseases resembling epileptic seizures (for example, fainting, hysterical seizures), and select a drug for treatment, additional research methods are carried out for the patient.
Approach to therapy
Treatment should be prescribed only if the patient has seizures, which is confirmed by epileptic EEG activity.
In the absence of attacks, even against the background of pathological waves on the EEG, treatment should not be prescribed, since pathological changes can be recorded without symptoms of diseases of the nervous system (observed in approximately 1% of healthy people).
In the presence of Landau-Kleffner syndrome, ESES, and various non-convulsive epileptic encephalopathies, antiepileptic drugs are prescribed, since these diseases cause memory and speech impairment, mental disorders, and, in children, growth retardation and learning difficulties.
Indications and contraindications
The procedure has no absolute contraindications. Electroencephalography is not performed if there are open wounds or rashes on the scalp. The study can be done on children and pregnant women, but in this case it is carried out without functional tests.
Indications for electroencephalography:
- traumatic brain injuries;
- epilepsy;
- seizures;
- loss of consciousness, panic attacks, dizziness, headaches;
- changes in sleep (waking up at night, insomnia);
- hepatic encephalopathy;
- delayed speech development;
- diencephalic syndrome;
- encephalitis, meningitis;
- suspicion of a tumor;
- assessment of the depth of anesthesia in case of surgery;
- confirmation of brain death;
- vegetative-vascular dystonia;
- vascular pathologies of the head and neck identified by ultrasound;
- stuttering;
- autism.
EEG is indicated for people with frequent headaches, convulsions, loss of consciousness, tics, sleep disorders, alalia, dyslexia, dysgraphia, dysarthria. Babies born as a result of complicated childbirth always need an examination.
For children under one year old, electroencephalography is performed only in a state of sleep. For older children, the procedure can be performed during the day. To do this, the child is seated on a chair or laid on a couch, a cap with sensors is put on his head, or electrodes (about 12) are attached to the scalp.
The frontal, parietal, temporal, occipital lobes of the brain should be covered
This is important for establishing the localization of epiactive zones. Next, the specialist performs the necessary manipulations
Parents need to explain to their child that the procedure is painless. Before examining the baby, it is necessary to feed and calm him. You will need to wash your hair, remove metal jewelry, and do not need to braid your hair. You are allowed to have your favorite toy with you.