Description
Frontal epilepsy refers to chronic pathologies of the nervous system. This disease develops with equal frequency in both sexes. Often the pathology first appears in childhood. In some cases, the disease may occur much later.
Frontal epilepsy is the second most common form of the disease. Characterized by the suddenness of attacks, often occurring against the background of preserved consciousness; very frequent but short-term convulsions.
The main diagnostic method is EEG. Treatment depends on the severity of the disease; most often medicinal. In some cases, surgical destruction of epifoci in the brain is used.
More often this happens after exposure to damaging factors affecting the brain. With this pathological condition, the frontal lobes of the cortical layer of the brain are affected. The exact localization of the epileptic focus is not always possible to establish.
When children experience frequent and prolonged epileptic seizures, one should think about their frontal origin.
To identify organic pathology of the brain, you need to do an MRI of the brain in epileptological mode.If treatment of frontal lobe epilepsy with one antiepileptic drug has no effect, it is advisable to combine it with other anticonvulsants.
Neurologist
Pershina Natalia Sergeevna
8 years of experience
It can be localized in the motor, dorsolateral or opercular cortex. Manifestations of the disease vary. In some cases, psychomotor disturbances and short bouts of seizures are considered signs of frontal lobe epilepsy. Sometimes the disease is characterized by a long-term localized convulsive syndrome, which is accompanied by depression of consciousness.
Frontal epilepsy is considered the second most common form of epilepsy after temporal lobe epilepsy. It occurs in 15-20% of patients. In some cases, the lesion is so widespread that it occupies several lobes of the brain. In this case, a diagnosis may be made: frontotemporal (combined) epilepsy.
Seizures in infants
The question of how to recognize epilepsy in a child under one year old is extremely important. In infancy, the disease often progresses atypically. Parents need to be extremely attentive to the condition and behavior of the newborn.
The initial stage of epilepsy in children under one year of age is characterized by the following signs:
- sudden fading;
- cessation of swallowing movements;
- throwing back the head;
- trembling eyelids;
- an empty, seeing nothing look;
- complete contactlessness.
After this, loss of consciousness and convulsions occur, not always accompanied by spontaneous bowel movements and urination. It should be noted that epilepsy in children under one year of age has a kind of prelude and completion. Harbingers of an attack are increased tearfulness, excessive excitability, and febrile temperature. After the seizure ends, the baby does not always fall asleep.
Classification
There are several classifications of frontal lobe epilepsy. The basis may be the time of occurrence of the seizure, the type of seizure, the frequency and duration of the convulsive syndrome.
Epilepsy awakening
This type of disease is characterized by the fact that an attack of seizures occurs mainly in the morning.
Wakeful epilepsy
This form is considered the most common. Convulsive syndrome develops during the daytime. It is often preceded by a deterioration in general condition. In some cases, an attack occurs suddenly - during study or work. The patient may be conscious.
Nocturnal epilepsy
This type of frontal epilepsy is considered the most dangerous, since in a dream a person cannot control what is happening and call for help. Sometimes the nocturnal form of frontal lobe epilepsy may not be diagnosed for a long time, since with short convulsive seizures the patient’s condition does not suffer.
Another clinically important classification is the division of epileptic seizures into types.
Motor type
Convulsions in this type of pathology can be clonic or tonic. The patient's consciousness was preserved during the attack. At the time of seizure development, gestural automatism is observed. Convulsions occur on the side opposite to the pathological focus.
Frontopolar type
This form of the disease is characterized by the development of pseudogeneralized seizures.
Orbitofrontal type
With this type of pathology, the lower anterior parts of the frontal zone suffer. Convulsive syndrome is accompanied by the development of olfactory hallucinations.
Dorsolateral type of epilepsy
A feature of this type of attack is adversion of the eyes and head.
Cingular type of frontal lobe epilepsy
It is based on damage to the anterior cingulate gyrus of the frontal zone. The attack is preceded by a feeling of fear, sweating, motor automatism and facial hyperemia.
Opercular type of epilepsy
Characterized by damage to the posterior lower part of the frontal zone. The attack is combined with autonomic disorders. Among them are dilated pupils (mydriasis) and increased heart rate.
Thanks to this classification, it is possible to identify the localization of the pathological “epileptic” focus, depending on the clinical manifestations of the convulsive syndrome.
Causes
There are many reasons why a disease such as frontal lobe epilepsy develops. Despite this, it is often not possible to find out exactly what exactly triggered the formation of the pathology. In such cases, the diagnosis is: idiopathic (cryptogenic) frontal lobe epilepsy. This means that the etiology of the disease is unknown.
Compounded hereditary history
The disease is believed to be genetically transmitted. The type of inheritance of epilepsy is autosomal dominant. This means that if the parents have the disease, the probability of developing the pathology in the child is 50%. Hereditary forms include nocturnal frontal lobe epilepsy.
Injuries
The development of pathology can be caused by brain contusions that occur due to blows, car accidents, falls, etc. In these cases, the disease develops at any age.
Tumors of the frontal region of the brain
As tumors develop, compression of neurons occurs. For this reason, normal brain tissue is subject to hypoxia and damage.
Both benign and malignant tumors contribute to the formation of epileptic foci in the frontal lobe. Symptoms depend on the size of the pathological formation and the location of the brain lesion.
Atrophic and degenerative neurological diseases
These pathologies are characterized by the fact that neurons are “discharged” and “gaps” appear in the brain tissue. As a result, various focal and psychological disorders may be observed. Among them is frontal lobe epilepsy.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
In addition, cerebral circulation disorders of the ischemic and hemorrhagic type, vascular malformations and infectious diseases of the brain (encephalitis) lead to secondary (acquired) pathology.
Disease prognosis
As a rule, the prognosis for the patient's future life is quite favorable. In 95% of cases, the disease goes away without a trace, even if it is not treated.
Dangerous consequences of the disease occur either in the case of an incorrect diagnosis, or in 5% of patients who have additional problems in the body that aggravate their condition. As for the adverse consequences, the most unpleasant among them is the development of classical epilepsy with all the ensuing consequences. Read about this disease in our article - What is epilepsy.
So, Rolandic epilepsy is a benign disease, but this does not mean that there is no need to monitor a child with such a diagnosis. The baby always requires attention, and especially with such problems. Don’t sleep through this dangerous illness, take care of yourself!
Clinical picture
Symptoms of frontal lobe epilepsy can vary. This depends on the individual characteristics of the human body, the age of the patient and the location of the epileptic focus. Nevertheless, this type of pathology has its own characteristics. These include:
- Suddenness. In most cases, a seizure develops without a previous change in well-being (aura).
- The initial phase of the convulsive syndrome is characterized by the sequential formation of tonic, postural, clonic and motor convulsive contractions.
- Often, an attack develops against the background of preserved consciousness, in contrast to temporal lobe epilepsy.
- High frequency of seizures.
- The short duration of the attack. Most often, muscle contractions last for several seconds.
- Rapid development of generalized convulsive syndrome.
- Presence of motor automatism.
- Absence of factors provoking an attack.
In the nocturnal form of frontal lobe epilepsy, the clinical picture is accompanied by enuresis, nightmares, and parasomnia. People suffering from this type of disease often complain of sleep disturbances, twitching (shuddering) of the limbs when falling asleep.
The nocturnal form of epilepsy can be combined with sleepwalking. Often such patients talk in their sleep. Waking up after an attack is accompanied by irritability and aggression. Most patients do not remember epileptic attacks that occurred at night.
Depending on the location of the pathological focus and the cause that caused epilepsy, a number of additional symptoms are identified. Among them are movement disorders, general cerebral symptoms, and behavioral disorders. For example, with brain tumors, in addition to seizures, the patient may experience visual or auditory hallucinations, mood changes, and headaches.
Atrophic and degenerative pathologies are characterized by memory and behavior disorders. Inflammatory diseases of the brain are accompanied by increased body temperature, the presence of meningeal symptoms, and photophobia.
Diagnostics
Frontal lobe epilepsy can be identified through patient observation and laboratory and instrumental examinations. First of all, the neurologist pays attention to the nature of the convulsive syndrome. With the motor type of epilepsy, short-term involuntary contractions of the muscles of the face and limbs occur on the side opposite the affected area.
The dorsolateral type of frontal epilepsy is accompanied by an involuntary rotation of the head and eyes in the direction opposite to the epileptic focus.
Orbitofrontal paroxysmal contractions are combined with disorders of cardiovascular activity and respiratory disorders. Frontopolar and cingulate types of epilepsy are characterized by mental and behavioral reactions.
Surgical treatment of epilepsy
Epilepsy is a disease characterized by recurrent seizures.
In addition to collecting complaints and monitoring the patient, instrumental diagnostics are required. This is necessary to identify the localization of the epileptic focus.
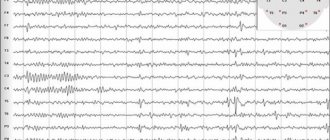
Examination methods for suspected frontal lobe epilepsy include electroencephalography (EEG), CT and MRI of the brain, Doppler ultrasound of the vessels of the head.
The first diagnostic procedure performed when a seizure syndrome occurs is an EEG. This method detects electrical activity in the brain. To improve diagnosis, the method is performed using provocative tests.
These include photostimulation and hyperventilation. It is best to conduct an EEG during an attack, as this will help to accurately determine the nature of the disease and the location of the damage.
In frontal lobe epilepsy, the electrical potentials emanating from this area differ from normal waves. In the period between attacks they become accelerated and sharpened, and at the moment of paroxysm they slow down.
For a qualitative diagnosis of the disease, all patients suffering from epilepsy must undergo an MRI of the brain. Thanks to this method, it is possible to establish the exact localization and extent of the pathological focus, identify brain atrophy, tumor formations, and hemorrhages.
In addition, some patients are indicated for ultrasound examination of the vessels of the neck and head, lumbar puncture (to exclude subarachnoid hemorrhage, meningoencephalitis), echoEG, etc.
Development of children with temporal lobe epilepsy
With temporal lobe epilepsy, parts of the limbic-reticular complex, which are responsible for intellectual brain activity, are affected. Memory and the ability for abstract thinking gradually decrease. The child becomes emotionally unstable and experiences difficulties in mastering educational material. The patient's thinking becomes slow. The teenager seems to be depressed: he often cries or, on the contrary, becomes aggressive. Temporal lobe epilepsy is accompanied by hypothalamic disorders, which manifest themselves in the form of disorders of puberty and the appearance of vegetative-vascular dystonia. Episodic attacks are characterized by shortness of breath, excessive sweating, rapid heartbeat, and abdominal pain.
Treatment methods
Treatment of frontal lobe epilepsy depends on the cause of its occurrence, as well as on concomitant brain pathologies. It should be aimed at stabilizing the patient's condition by reducing the frequency of epileptic seizures.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
Both medical and surgical treatment are used. At the time of attacks, symptomatic therapy is performed. Anticonvulsants are used for this purpose.
Several times a year (depending on the frequency of attacks), patients should be examined by a neurologist and have an EEG done.
For uncontrolled and frequent attacks, surgical intervention is necessary. In addition, it is carried out when identifying tumors in the frontal lobe of the cortex, intracerebral hematoma, stroke. Surgical treatment consists of removing the pathological focus.
Thanks to this, compression of the brain tissue stops, and epileptic seizures do not occur. However, brain surgery has certain risks, so it is indicated only in cases where drug therapy is ineffective.
Disease prognosis
In 80% of cases, persistent and long-term treatment of epilepsy in children leads to relief from a serious illness. The immediate environment of little epileptics should help them develop normally and find their place in society. Patience, wisdom and love of parents play a huge role in this.
Svetlana Fomenko
Local therapist, freelance regional nephrologist, head of the day hospital of the Bogorodchansk Central District Hospital.
Education
Ivano-Frankivsk Medical Institute Faculty of Medicine, General Medicine, Ivano-Frankivsk Higher specialized, from 09.1984 to 06.1990
Forecast for life
The prognosis for this disease depends on where the lesion is located, as well as on the clinical picture of epilepsy present in a particular patient. Congenital epilepsy has a poor prognosis, as it tends to progress. With acquired frontal epilepsy, a complete cure is possible if it is possible to remove the pathological focus.
Considering that attacks with frontal lobe epilepsy occur suddenly, patients need constant monitoring from loved ones. In the presence of concomitant pathologies of the brain (dementia, motor and mental disorders), as well as uncontrolled attacks of convulsive syndrome, patients are assigned disability group 2 or 3.
Frontal epilepsy is a serious disease of the nervous system. If you suspect this pathology, you should immediately undergo examination. People suffering from epilepsy are monitored by a neurologist for life.