Causes
There is still no 100% reliable data on why seizures occur in children with benign childhood epilepsy. The dominant theory in medicine is that the disease is a consequence of minor disorders in brain maturation, which in 60% of cases are genetically determined.
The disease is temporary. As the cortex and frontal lobes mature, epileptic seizures diminish. In general, childhood epilepsy is a classic age-related disorder.
Violations are provoked by a number of factors:
- individual characteristics of the maturation of certain areas of the brain (hippocampus, neocortex, etc.);
- excessive production of excitatory neurotransmitters;
- immaturity of GABA receptors, etc.
Survey results
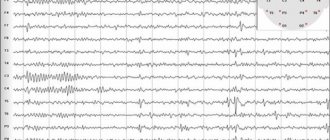
A specific symptom of epilepsy in children during instrumental research is the identification of a high-amplitude sharp wave or squeaks localized in the central-temporal region. With the combined development of such formations with subsequent slow waves, an entire Rolandic complex is formed. External signs of the disease may be very similar to the clinical picture obtained during an ECG.
Most often, the disease is diagnosed on the side opposite to convulsive seizures, but sometimes the doctor detects a bilateral picture. The main distinguishing features of benign rolandic epilepsy include variability in readings from one ECG recording to another.
Symptoms and signs
Childhood benign epilepsy manifests itself with a number of characteristic symptoms:
- The main symptom is convulsive attacks, in which there is no loss of consciousness. Spasms affect the limbs, facial muscles, and larynx.
- The seizure is preceded by a so-called “sensory aura.” The child feels slight pinching, tingling on one side of the body, numbness in part of the face and throat.
- Due to spasms of the larynx, problems with speech arise. During a seizure, characteristic “gurgling” sounds appear, as if gargling. Speech is impaired. There is increased salivation.
- In 80% of cases, attacks occur at night, when the brain's operating mode changes.
- Spasms of the right/left side of the face often spread to the limbs located on the same side (homolateral). Sometimes the “side of the attack” can change from left to right and vice versa.
- In rare cases, the disease is accompanied by complex epileptic seizures, in which the child loses consciousness for several seconds. In 20% of young patients, an epileptic seizure affects the entire body. For the entire period of convulsions, the patient loses consciousness.
- During a seizure, the patient cannot control the position of his body, the work of his arms and legs.
One of the varieties of the disease is occipital epilepsy with a late onset (from 8 years of age and older). With it, attacks are often combined with disturbances of consciousness, rolling (deviation) of the eyes, and vomiting.
Spasms occur quite rarely. In 75% of cases - in a dream, when the child is absolutely helpless. With late onset of childhood epilepsy, the patient may experience visual hallucinations. Cramps usually affect one side of the body. After their completion, many patients experience severe headaches.
Features of the disease
Rolandic type is included in the category of focal epilepsies. Its name means that the problem area is located in the Rolandic sulcus of the brain. Therefore, the focus of seizures is concentrated in the neurons of the temporal regions. According to the ICD, the disease is coded G40.
This epilepsy is considered the most common of all benign ones that can occur in children. It accounts for approximately 15% of cases of such diseases under the age of 15 years and more than 20% of any manifestations of convulsive seizures. In most cases, the initial symptoms of epilepsy appear between the ages of 4 and 10 years, and the peak of symptoms is concentrated between 7 and 9 years of age. Sometimes the disease first appears in 2-3 year old children or adolescents whose age does not exceed 11-12 years. Boys are more likely to experience Rolandic epilepsy - the ratio of the incidence of the disease to girls is 6 to 4.
Often the early stages of the disease are preceded by mild seizures in newborns under 18 months of age. Febrile seizures may also occur in children under 2 years of age, which later develop into epilepsy. Adults never experience this disease.
The exact root causes of this pathology have not yet been identified. It is assumed that heredity may play a large role. If a mother or father suffers from epilepsy, the risk of it developing in a child increases significantly. The main reason that scientists are leaning toward is gene defects. Studies have shown that the disease develops when there are disorders at the stage of brain formation. Also, its appearance is partly due to an increase in the excitability of individual neurons. This is associated with an increase in neurotransmitters, a drop in GABA levels and an increase in the number of excitatory reentrant synapses.
The main manifestation of benign epilepsy in children is seizures. According to their characteristics, the disease is classified into several types:
- simple seizures - short-term twitching or convulsions on the left or right side of the face, accompanied by numbness, as well as loss of control over the muscles of the lips, tongue, larynx and pharynx;
- complex partial seizures - convulsions of one or more facial muscles with continuous tension of the tongue or pharynx, often combined with speech impairment and increased salivation;
- secondary generalized seizures are ordinary seizures involving the muscles of the face, numbness and immobilization, developing into a generalized seizure.
An atypical type of epilepsy in combination with rolandic is possible. It is classified into: nocturnal seizures, myoclonic and astatic seizures, atonic seizures and atypical absence seizures. In some cases, such epilepsy occurs outside the Rolandic type, but is similar to it.
Seizures may be part of idiopathic seizures. In this case, epilepsy is not Rolandic and may be accompanied by many other symptoms, including prolonged loss of consciousness and respiratory arrest
It is very important to differentiate these two types of disease in order to receive the correct treatment
Course of the disease
Benign childhood epilepsy in a child is episodic in nature. Seizures occur quite rarely, from one to several times a year. Each lasts, on average, 2-3 minutes. At an early age, epileptic seizures occur more often. The older the baby gets, the less often his illness makes itself felt.
Landau -Kleffner syndrome may occur . With it, the baby experiences frequent seizures. Sometimes they literally follow one another. Most often this happens at the age of 3-7 in children whose relatives had (suffer from) epilepsy. Patients with this diagnosis experience a long-term speech disorder (can last several months).
A similar picture is observed with pseudo - Lennox syndrome , which is accompanied by a variety of frequent attacks accompanied by cognitive impairment. The peak of disease activity occurs in the early period (up to 7-8 years).
Epilepsy: general characteristics
In the classical definition, epilepsy is a mental illness manifested in the form of periodic paroxysmal seizures, which is most often accompanied by neurological and somatic pathologies and a personality tendency towards concentric dementia. From a clinical point of view, epilepsy is characterized by chronic psychoses and other personality disorders. Seizures occur as a result of sudden synchronous activity of neural connections called discharges. The characteristic features of paroxysms, as well as symptoms, directly depend on the type and form of manifestation of the disease.
Types and forms of epilepsy in children
For children, traditional types of epilepsy are also typical - reflex, temporal, frontal and Lennox-Gastaut syndrome, but below we consider exclusively the forms characteristic of minors.
Febrile seizures.
Age – up to 6 years.
High body temperature is a serious stressor for a child. It is characterized by severe, prolonged convulsions and loss of consciousness by the child. Febrile epilepsy is often confused with chills or symptoms of fever.
Infantile spasms.
Age – up to 2 years.
Manifested by a sudden raising of the head or limbs by the child. They can be repeated many times even throughout the day. Accompanied by a delay in the intellectual development of the baby. At 2-3 years, infantile spasms stop, most often the disease develops into Lennox-Gastaut syndrome.
Rolandic epilepsy.
From 2 to 13 years.
Attacks manifest themselves in the form of numbness in one part of the face, tongue and lips. Speech is difficult, sometimes the child cannot remember the name of this or that thing. Consciousness is preserved. Other types of spasms may also occur.
Myoclonic epilepsy.
Puberty
Atonic and tonic-clinical seizures with loss of consciousness most often occur in the morning or under the influence of sudden and unexpected irritating factors. Deviations in intelligence are not noticed in adolescents with such a deviation.
Types of seizures in children
There are dozens of different types of epileptic seizures, but the most common, especially among children, are the following 3 types:
- Atonic attacks. They imply a sharp simultaneous relaxation of muscles. Very similar to normal fainting.
- Tonic-clinical seizure. Most often, its effect is directly associated with epilepsy. A seizure is expressed in loss of consciousness and simultaneous convulsions of the whole body. Usually lasts only a few minutes.
- Absence seizures. It is quite difficult to notice the signs of this form. During an attack, a person simply freezes. May be accompanied by eyelid tic. It lasts only 3-4 seconds, during the attack the patient does not react to what is happening.
Epileptic signs are not necessarily associated with loss of consciousness, for example, with fibrous, rolandic and myoclonic forms of the disease, the child will fully or partially retain consciousness and even the perception of temperature and pain.
Diagnostics
The main method for diagnosing the disease is EEG. Since Rolandic epilepsy most often manifests itself at night, the child is measured with amplitude fluctuations in brain activity both during wakefulness and during sleep. The attack is expressed in high-amplitude peaks, followed by slow waves.
In parallel with this study, diagnostics of other disorders is carried out, which makes it possible to separate childhood epilepsy itself from abscess, purulent meningitis, traumatic brain injury, pseudo-Lennox syndrome and other diseases. If the picture is not clear, the child is given an MRI of the head.
Treatment of Rolandic epilepsy
Due to the fact that childhood epilepsy goes away on its own after puberty, the need for its treatment is still in question. Here the opinions of neurologists are divided. Some believe that drug treatment for this age-related disease is not advisable. Others insist on therapy to prevent the development of arrhythmias and other disorders.
Monotherapy is always used to treat this disease. The child is not prescribed a whole complex of various medications (which is usually the case with other diseases), but only 1 antiepileptic drug. Most often this is something from a series of medications based on valproic acid.
In case of intolerance, levetiracetam, carbamazepine, topiramate, etc. are prescribed. Any drug from this list should be prescribed by a doctor. Every medicine has side effects. If used incorrectly, attacks may become more frequent.
First aid
Nocturnal epileptic seizures often go undetected. The fact that they took place can only be indicated by a severe headache in the morning. However, benign rolandic epilepsy requires constant monitoring.
Attacks that occur during the day usually frighten the patient himself. The child needs to be reassured at this time. If coordination is lost, he should be placed comfortably on his back and his head turned to the side. A handkerchief should be placed in the patient's mouth. This will help prevent biting or sticking of the tongue.
If the attack lasted a couple of minutes and passed without consequences, you can do without calling an ambulance. Increased duration of convulsions with arching of the whole body and the danger of asphyxia requires medical intervention.
Description of the disease
Most often, benign rolandic epilepsy goes away on its own by the age of 15-18 years. It is for this reason that such a disease is usually called benign. The name is also associated with the location of the epileptic focus. Roland's fissure is a region of the brain.
Boys are susceptible to this condition several times more often than girls. The ratio of boys to girls is 6:4. Seizures are distinguished by their partial nature, in another way - focal. This can be explained by the fact that the diseased area is located in the area of the Rolandic sulcus. The international classification classifies this disease as class G40.