The human brain remains a poorly understood organ to this day. Mental processes occurring in the brain, their origin, control and modification are constantly of interest to neurologists who study the functioning of the brain. Since the possibility of recording brain function indicators on an electroencephalogram, paroxysmal activity has been identified and studied as a collective concept for many pathological processes.
The concept of paroxysmal activity
Paroxysmal states in neurology are the process of an increase in the amplitude of brain activity on the electroencephalogram. An interesting fact is that the amplitude of the waves not only increases sharply, but also does not appear chaotically. In addition to the waves themselves, the source of their origin is also recorded. Sometimes some doctors deliberately narrow paroxysmal activity to epileptic seizures , however, this is not true.
In fact, the concept of paroxysmal activity is much broader; it includes various pathological conditions, in addition to the most well-known disorder - epilepsy. For example, typical wave rises with a center of origin of activity are recorded both in neuroses and in acquired dementia.
An interesting fact is that a child may have paroxysms as a variant of the norm, since paroxysmal activity of the brain will not be supported by pathological changes in the structures of the brain.
Even in the presence of diagnosed foci of paroxysms, doctors believe that before the age of 21 it is too early to sound the alarm - at this time the bioelectrical activity of the brain may not be synchronous and a paroxysmal case is precisely such confirmation.
For adults, it makes sense to talk about paroxysms as a pathological process occurring in the cerebral cortex. If we talk about paroxysm, as the most general concept, we can summarize the following: paroxysm is an intensified attack, occurring at the maximum of its tension and repeating a certain number of times.
Thus, the paroxysmal state will have the following characteristics:
- in the cerebral cortex there is an area with excitation processes that prevail over inhibition processes;
- excitation of the cortex is characterized by a sudden onset and an equally unexpected decline in activity;
- When studying brain impulses, a characteristic pattern is noticeable on the electroencephalogram, in which one can trace the waves reaching their highest amplitude.
Paroxysmal brain activity - signs and therapy
The human brain matures gradually.
By the age of 21, brain structures are fully formed. The maturity of the cerebral cortex and subcortex is revealed by electroencephalography - a method of recording bioelectric impulses that arise during electrical activity of the brain. Normally, in a healthy person, all waves on the EEG have the correct rhythm and amplitude. If the brain is immature or a person suffers from mental and neurological diseases, the qualitative and quantitative indicators of waves on electroencephalography change. One of these manifestations is paroxysmal activity.
What it is
Paroxysmal activity is a value that is recorded on the electroencephalogram. Paroxysmal brain activity is a change in the normal wave, and is manifested by peaks, peaked waves, pathological complexes and a slowdown in the electrical activity of the brain.
In a broad sense, paroxysmal activity is abnormal electrical activity of the brain.
The focus of paroxysmal activity occurs in many pathological human conditions:
- Neurotic (depression, social phobia, panic attacks) and severe mental (schizophrenia) disorders.
- Immaturity of the brain.
- Epilepsy and epileptiform disorders.
- Dementia.
- Severe intoxication with drugs, alcohol, metals.
- Encephalopathy.
- Chronic stress, severe physical fatigue or mental exhaustion.
- Increased intracranial pressure.
- Psychopathic personality changes.
- Autonomic disorders.
When paroxysmal activity is recorded, doctors mean by this a phenomenon in which the processes of excitation in the cortex and subcortex greatly predominate over the processes of inhibition. Signs of paroxysmal activity: sudden onset, transience, sudden termination and tendency to relapse.
On the electroencephalogram, paroxysmal brain activity appears as a series of waves, the amplitude of which quickly approaches a peak. Paroxysmal activity covers EEG rhythms: alpha, beta, delta and theta rhythms.
To study the nuances, doctors compare peaked waves with normal ones. Fundamental indicators of activity are considered: basic activity, symmetry, rhythm, amplitude. Changes in activity during brain stimulation are also recorded: light or sound stimulation, a state of hyperventilation, opening or closing the eyes.
Kinds
Classification of paroxysmal disease based on changes in wave types on the electroencephalogram.
Alpha rhythm. Its normal frequency is from 8 to 13 Hz, the amplitude reaches 100 μV. Paroxysmal brain activity in children with alpha rhythm indicates the following possible pathologies:
- The third type of neurotic reactions is a continuous course, prone to relapses and exacerbations of the clinical picture.
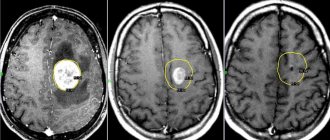
- Tumor, cyst and other intracranial space-occupying processes. The difference in activity between the right and left hemispheres of the brain speaks in their favor.
- Recent traumatic brain injury with unstable frequency.
Beta rhythm. Normally, its amplitude is from 3 to 5 μV, frequency is from 14 to 30 Hz. Local and paroxysmal pathological activity occurs when the frequency reaches 50 μV. It is registered when a child’s psychomotor development is delayed.
Delta and theta rhythms. Paroxysmal activity of the brain in an adult is recorded during chronic atrophic and dystrophic changes in the cortex and subcortical structures. Most often this is associated with dyscirculatory encephalopathy, tumors, hypertensive syndrome, and profound acquired dementia. Bilaterally synchronous paroxysmal activity speaks in favor of dementia.
The most distinct paroxysmal activity is observed in epilepsy. Paroxysmal activity on the EEG in a child with a benign course is revealed by central and temporal spike waves, focal discharges with sharp waves mainly in the area of the temporal cortex.
The type of epilepsy can be judged by the type of pathological activity. Childhood epilepsy with absence seizures is characterized by bilateral synchronous waves with a spike wave frequency of 3 Hz. Activity duration is up to 10 seconds per episode. The attack begins with a frequency of 3 Hz, and then the rhythm slows down. Juvenile absence epilepsy is characterized by polyspikes, the frequency of which is above 3 Hz.
Landau-Kleffner syndrome is characterized by sharp and slow waves in the projection of the temporal cortex. They are bisynchronous and multifocal. As the disease progresses, an electrical status of slow-wave sleep occurs. It is characterized by continuous spike waves that are activated during the rapid eye movement phase of sleep.
Progressive epilepsy with myoclonus is characterized by generalized spike waves, potentiated amplitudes, and disturbances in wave rhythms.
When hypersynchrony of all waves on the EEG is observed, this is a decrease in the threshold of paroxysmal activity. Typically, with hypersynchrony, the amplitude increases greatly, and the wave acquires a pointed peak. If the threshold for paroxysmal activity is reduced, the threshold for seizure activity in the brain decreases.
This means that for a convulsive seizure to occur, a large-scale paroxysmal focus in the brain is needed, that is, mild paroxysmal activity of the cerebral cortex will not provoke a seizure and the anticonvulsant system of the brain will work.
A low threshold indicates effective antiepileptic treatment.
Therapy
Paroxysmal activity is not the target of therapy. Initially, the cause that caused the abnormal functioning of the brain is eliminated. The following treatment principles are used:
- Etiotropic therapy. Aimed at eliminating the cause. For example, for dyscirculatory encephalopathy - improvement of cerebral circulation, for neuroses - psychotherapy.
- Pathogenetic therapy. Aimed at eliminating pathological factors. For example, in case of metal intoxication, drugs are prescribed that bind the heavy metal and remove it from the body.
- Symptomatic therapy. Aimed at eliminating symptoms.
When these three treatments are prescribed and effective, the paroxysmal brain activity resolves on its own.
Didn't find a suitable answer? Find a doctor and ask him a question!
Source: https://sortmozg.com/zabolevaniya/paroksizmalnaya-aktivnost
Analysis of the rhythm of bioelectric impulses
Biorhythms of the brain are divided into several groups, each of which is named after its Latin letters. So, there are alpha rhythms, beta rhythms, theta and delta rhythms. Depending on the identified rhythm of activity, one can assume what pathology such impulses are associated with.
This is extremely important in the diagnosis of hidden brain pathologies, which sometimes manifest themselves as paroxysmal states.
When deciphering an electroencephalogram, rhythms are the main focus. When reading diagnostic results, it is very important to take into account the symmetry of the appearance of activity in both hemispheres, the basal rhythm, and changes in rhythms during functional loads on the body.
Alpha rhythms normally have an oscillation frequency of 8 to 13 Hertz (Hz). The amplitude of normal oscillations is up to 100 μV. Rhythm pathologies are spoken of in the following cases:
- if the rhythm is associated with neuroses of the third type;
- with interhemispheric asymmetry of more than a third, there is reason to talk about a tumor or cystic neoplasm, a post-stroke condition with tissue scarring, or a previously suffered hemorrhage in this location;
- if the rhythm is unstable, doctors suspect a concussion.
Amplitude disturbances are also recognized as a sign of pathology. Although officially it is the maximum possible 100 μV, but with a value less than 20 and more than 90 units, doctors already suspect pathological abnormalities.
Beta rhythms are also present during normal brain activity and, under certain parameters, do not at all indicate a paroxysmal state. This rhythm is most pronounced in the frontal lobes of the brain.
The amplitude is normally small - from 3 to 5 μV. A normal reserve is an increase in activity by 50 percent, i.e. Even with an amplitude of 7 µV, beta rhythms can be conditionally considered normal, but already when this figure is exceeded they are classified as paroxysmal activity.
For example, waves of this type of diffuse nature with a length of up to 50 µV indicate a concussion. Short spindle-shaped waves will indicate the presence of encephalitis - an inflammatory disease of the meninges, and the frequency and duration of the wave’s existence illustrate the severity of the inflammatory process.
When beta-active waves with a high amplitude of about 30-40 μV and a frequency of about 16-18 Hz are detected in a child, they speak of delays in the child’s mental development.
Theta and delta waves are predominantly recorded in humans during sleep. Therefore, when examined by a doctor while awake, they are not normally recorded. If such waves appear, then this indicates degenerative processes in the brain.
A paroxysmal state usually occurs when the brain matter is compressed, so the doctor may suspect swelling of the brain or a tumor. Theta and delta waves differ in that they indicate severe and profound changes in the brain. Like all waves, theta and delta waves before the age of 21 are not considered a pathology, since in children and adolescents they are a variant of the norm .
In people older than this age, the presence of such waves indicates acquired dementia. In parallel, this is confirmed by synchronous flashes of theta waves with high amplitude. In addition, such waves indicate the presence of neurosis.
Disorder of consciousness
Paroxysmal disorder of consciousness manifests itself in the form of neurological attacks. It can occur against the background of apparent health or during an exacerbation of a chronic disease. Often, paroxysmal disorder is recorded during the course of a disease that is not initially associated with the nervous system.
The paroxysmal state is characterized by the short duration of the attack and the tendency to recur. The disorder has different symptoms, depending on the provoking condition. Paroxysmal disorder of consciousness can manifest itself as:
- epileptic seizure,
- fainting,
- sleep disorder,
- panic attack,
- paroxysmal headache.
The causes of the development of paroxysmal conditions can be congenital pathologies, injuries (including at birth), chronic diseases, infections, and poisoning. Patients with paroxysmal disorders often have a hereditary predisposition to such conditions. Social conditions and harmful working conditions can also cause the development of pathology. Paroxysmal disorders of consciousness can cause:
- bad habits (alcoholism, smoking, drug addiction);
- stressful situations (especially when they are repeated frequently);
- disturbance of sleep and wakefulness;
- heavy physical activity;
- prolonged exposure to loud noise or bright light;
- unfavorable environmental conditions;
- toxins;
- sudden change in climatic conditions.
Types of paroxysmal activity
Taking into account all the characteristics, the phenomenon of paroxysmal states is classified into two large categories - epileptic and non-epileptic.
Epileptic type of activity is manifested in a sick person by typical conditions - seizures that appear from time to time. These are convulsive conditions that occur with a certain frequency, and sometimes repeat one after another.
Epilepsy can be a congenital pathology, but it can also be acquired if a person has suffered a severe traumatic brain injury, suffers from a brain tumor, intoxication, or has experienced conditions of severe ischemia. Epilepsy, in turn, is also divided into convulsive and non-convulsive; the picture of such conditions is very diverse.
Grand mal seizure
Most often, this type of seizure occurs in an epileptic condition. It goes through several phases, replacing one after another. In the initial phase of development of the pathological condition, the patient experiences a so-called aura. It lasts for several seconds and indicates the imminent approach of epilepsy.
With an aura, patients experience clouding of reason, they fall out of the events taking place around them, and hallucinations and affective facts come to the fore in consciousness. Considering the clinical signs of an aura, we can talk about the presence of a focus of excitation. The aura during paroxysmal conditions can be:
- viscerosensory - accompanied by an attack of nausea, unpleasant sensations in the stomach, after which all these signs “rise up”, are noted in the lungs, behind the sternum and such an aura ends with a blow to the head and loss of consciousness;
- visceromotor - this condition has various manifestations, for example, dilation and constriction of the pupil, not associated with a change in the light entering the organ of vision, alternating hot flashes with chills, the appearance of goose bumps, abdominal pain and bouts of diarrhea;
- the sensory aura is characterized by various disorders of the sensory organs, auditory and visual hallucinations, dizziness, increased odors;
- impulsive aura is manifested by abnormal motor activity. This could be sharp screams, aggression towards others, pyromania or kleptomania, acts of exhibitionism;
- psychic aura - usually manifests itself as a hallucination, during which a person performs active actions in an imaginary world - sings songs, dances, goes to a demonstration, argues with someone. This type of disorder is called hallucinatory mental activity. There is also ideational activity, which manifests itself in problems with thinking. The patients themselves, who have experienced such seizures with ideational activity, describe them as a stupor of thoughts.
All these various auras are harbingers of paroxysmal states and indicate the imminent onset of an epilepsy attack.
Usually the epileptic seizure itself begins immediately after the aura; there are no specific signals about its onset. A seizure can occur in a convulsive or non-convulsive scenario. Atypical forms of a seizure are tonic or clonic phases. Sometimes they cause complete relaxation of the patient’s body, and sometimes convulsive activity is recorded only in one half of the body.
The classic manifestations of epilepsy are seizures that affect the entire body. Convulsions and seizures are observed in the limbs and throughout the body, so epilepsy is extremely difficult to tolerate.
Short-term seizures are not dangerous; a person can only injure himself when falling, but with prolonged epileptic seizures there is a risk of cerebral edema and death.
Seizures in severe cases are quite long, about half an hour. And they follow each other. The person seems to be in a comatose state, in a stupor . Urea increases in the blood, and increased protein content is found in the urine.
Often the last attack has not yet subsided when a new attack begins. And if the body still copes with isolated attacks and stops them, then with frequent attacks this does not happen. Such patients are diagnosed with status epilepticus.
Minor seizure
A minor seizure, although smaller in volume, is much more difficult to determine in terms of diagnosis, since there are many characteristics of minor seizures that can be difficult to classify correctly. Among the signs of this type of seizure are:
- short-term loss of consciousness;
- unexpected twitching of limbs, unclenching of hands;
- falling to the ground;
- propulsive movements - forward impulses, for example, a sharp forward movement of the head;
- falling and the appearance of convulsions after an axial turn.
Paroxysmal states of a nonconvulsive nature are associated with clouding of consciousness for a short time, visions of delirium with fantastic plots. Due to their similarity, such paroxysms are called narcoleptic.
With ambulatory automatisms, a person detaches himself from the environment and begins to make some unconscious, that is, automatic movements. Sometimes this may be associated with aggressive behavior towards others.
Paroxysmal dream states are characterized by specific signs - a person remembers everything that he sees and experiences, but the picture of the outside world is absolutely not perceived by him.
Paroxysmal brain activity - what is it?
Paroxysmal brain activity is a fairly broad concept that characterizes the manifestations of a certain range of disorders.
This type of brain activity represents the electrical activity of the cerebral cortex, in one of the areas of which the processes of excitation exceed the processes of inhibition.
In this case, the process of excitation is distinguished by a sudden onset, a rapid course and an equally sudden ending.
On the EEG, the emerging paroxysmal activity is displayed in the form of sharp waves , which are characterized by the fastest possible achievement of their peak (highest point). There are two types of paroxysmal brain activity: epileptic and non-epileptic.
Epileptic paroxysmal activity is provoked by a disease such as epilepsy. Epilepsy is a chronic brain pathology that expresses itself in the form of various types of seizures that are prone to recurrence.
An epileptic seizure can be convulsive or non-convulsive. There is a fairly broad typology of seizures:
- Grand mal seizure.
- Minor seizure.
- Psychosensory seizures.
- Twilight state of consciousness.
- Generalized seizures.
- Partial (focal).
Non-epileptic paroxysmal activity is expressed by the following symptoms:
- Autonomic disorders (dizziness, pressure changes, nausea, tachycardia, angina pectoris, weakness, stool upset, chills, shortness of breath, shortness of breath, sweating, pain in the left side of the chest).
- Headache.
- Hyperkinetic disorders: tics, myoclonic jerks, Friedreich's syndrome, Unferricht-Lundborg disease, ataxia, dysarthria, Crumpey disease, etc.
- Dystonic syndromes of the muscular system (torso curvature, torsion spasm, scoliosis).
- Migraines (simple and with aura).
The non-epileptic form is most often found in children, adolescents, the elderly, as well as in people prone to neurotic disorders.
Causes
- Violation of the body's metabolism. These include: hypothyroidism and hyperthyroidism, diabetes mellitus, Cushing's disease, menopause, etc.
- Psychovegetative syndrome: neuroses, depression, phobias, hysterical personality development, mania, etc.;
- Increased symptoms can cause exacerbation of the following diseases: pyelonephritis, liver failure, pneumonia, etc.
- Alcohol and drug intoxication.
Electroencephalogram (EEG) study
EEG is one of the most popular methods for diagnosing many types of diseases. It is designed to study the electrical activity of the brain without damaging the scalp.
Using special electrodes, readings of brain activity are taken in the form of alpha, beta, theta and delta waves.
During paroxysms, it is mainly the alpha rhythm that is disrupted (normally it is observed at rest).
It is the EEG that can detect paroxysmal activity. With one type of brain activity or another, the rhythm of the waves changes. During paroxysmal activity of the brain, a sharp increase in the amplitude of the wave occurs, and it is also clearly noticeable that such activity has centers - foci. EEG can detect not only the localization of the focus of paroxysmal activity, but also its size.
Brain activity is displayed graphically - you can see the length and frequency of each wave at the moment of wakefulness, falling asleep, deep sleep, anxiety, mental activity, etc.
With paroxysmal activity of the cerebral cortex, the waves will look like this: peaks will predominate, peaks may alternate with a slow (long) wave, and with increased activity, so-called spike waves will be observed - a large number of peaks following each other.
Treatment
First of all, it is not the paroxysmal activity itself that is treated, but its causes and consequences. Depending on the disease that caused the paroxysms.
- If this is a head injury, then localized damage is eliminated, blood circulation is restored, and then symptomatic treatment follows.
- With epilepsy, they first look for what can cause it (a tumor, for example). If epilepsy is congenital, then they mainly fight the number of seizures, pain syndrome and detrimental consequences for the psyche.
- If paroxysms cause problems with blood pressure, then treatment will be aimed at therapy of the cardiovascular system, etc.
The main thing is that everyone should know that if a doctor writes in the conclusion “the presence of paroxysmal brain activity”, this is not a final diagnosis. And it certainly does not mean that you should be diagnosed with epilepsy or another serious disease. It is recommended not to panic, but to undergo examination by a therapist, neurologist and psychotherapist.
Source: https://moyagolova.ru/paroksizmalnaya-aktivnost-golovnogo-mozga-chto-eto/
Non-epileptic conditions
Such paroxysmal activity can be divided into several types - muscle dystonia, autonomic disorders, headaches, myoclonic syndromes. They usually first appear at a young age and progress in old age .
This is usually affected by cerebrovascular accidents seen in older people. Therefore, to prevent such conditions, patients are prescribed drugs in advance to activate cerebral blood flow. This is done with extreme caution, since the wrong medicine can provoke a seizure.
Different forms of seizures
When considering the syndrome of paroxysmal states, it is worth paying attention to those diseases that most often accompany such crises.
- headache;
– myoclonic syndromes and other hyperkinetic states;
– autonomic disorders;
– muscular dystonic syndromes and dystonia.
In most cases, these problems are recorded in patients who have not reached the age of majority. But recently, more and more often, the paroxysmal state makes itself felt for the first time already in adulthood. It is also possible for the symptoms of the above diseases to dynamically progress, which become more severe against the background of chronic and acute cerebrovascular accidents or age-related cerebral disorders.
It is also important to take into account the fact that in some cases, non-epileptic paroxysmal conditions may be a consequence of the effects of certain medications prescribed to neutralize circulatory failure, as well as diseases such as parkinsonism and some mental disorders caused by old age.
Epilepsy is not the only form of manifestation of disorders of the central nervous system. There are other paroxysmal conditions in neurology that can be classified as epileptic.
One striking example is sensory (sensitive) Jacksonian seizures. Their manifestation occurs when a person is conscious. Symptoms include tingling and numbness in the face, limbs and half of the torso. In some cases, sensory seizures can turn into motor ones, which will significantly complicate the patient’s condition.
Attention should also be paid to Jacksonian epilepsy. In this case, both sensory and motor seizures are possible. The latter are especially problematic because they involve muscle spasms in the part of the face and limbs that are located on the side opposite the epileptic focus. In this case, disturbances in consciousness, as a rule, are not observed. In some cases, motor seizures can become generalized.
Complex absence seizures can be atonic, myoclonic, or akinetic. The first make themselves known through a sudden fall, the cause of which is a sharp decrease in the postural tone of the legs. As for the myoclonic form, it is characterized by rhythmic short-term muscle twitching, accompanied by a loss of consciousness. Akinetic absence seizure is a seizure with immobility, which can also result in falls.
Small absence seizures are also possible, in which a person also plunges into an unconscious state. There are no feelings of discomfort after its completion. The patient often cannot remember the moment of the attack.
Kozhevnikov epilepsy is characterized by limited short seizures that are clonic in nature. They most often capture the muscles of the arms, but the tongue, face and even legs can be affected by this process. Loss of consciousness during such convulsions is a rare occurrence.
Such paroxysmal activity can be divided into several types - muscle dystonia, autonomic disorders, headaches, myoclonic syndromes. They usually first appear at a young age and progress in old age.
This is usually affected by cerebrovascular accidents seen in older people. Therefore, to prevent such conditions, patients are prescribed drugs in advance to activate cerebral blood flow. This is done with extreme caution, since the wrong medicine can provoke a seizure.
- headache;
– myoclonic syndromes and other hyperkinetic states;
– autonomic disorders;
– muscular dystonic syndromes and dystonia.
Epilepsy is not the only form of manifestation of disorders of the central nervous system. There are other paroxysmal conditions in neurology that can be classified as epileptic.
Kozhevnikov epilepsy is characterized by limited short seizures that are clonic in nature. They most often capture the muscles of the arms, but the tongue, face and even legs can be affected by this process. Loss of consciousness during such convulsions is a rare occurrence.
Treatment of paroxysmal conditions is the domain of highly qualified specialists. Therefore, if signs of a single seizure become noticeable, especially when it is the first, the patient must be urgently hospitalized in a neurosurgical or neurological department. There they will be able to examine him and determine the current treatment plan.
It is important to ensure that the patient does not suffer any injuries before being taken to the hospital. It is also worth putting a spoon wrapped in a bandage into the mouth or using a mouth dilator.
In most cases, the treatment process for patients with status epilepticus begins in the ambulance. If doctors are not yet around, and the person is still having a seizure, then the first thing to do is to rule out the possibility of aspiration of vomit or mechanical asphyxia due to tongue prolapse.
As for non-epileptic forms, the causes of paroxysmal states can be completely different. It all depends on the key disease, the symptoms of which are aggravated. Therefore, the best thing that can be done is to take the person to the hospital as quickly as possible, where he can be examined and an accurate diagnosis made.
Therapy of paroxysms
It is impossible to cure the manifestations of paroxysmal activity until the causes of its occurrence are removed. If a person has suffered a head injury, then doctors try to eliminate the effect of the damaging factor as early as possible and restore blood circulation in the injured area, so as not to provoke the appearance of paroxysmal activity.
If paroxysms appear as a result of increased intracranial pressure, then all measures are taken to normalize blood circulation, and tactics for further prolonged care for such patients are determined.
Major convulsive seizures are more difficult to cope with; they are treated surgically, and the treatment does not always give a stable result.
In cases of a seizure, a sick person must be protected from injury, and after the seizure ends, he must be helped to recover . If the attack lasts longer than 5-7 minutes, it is necessary to call an ambulance and the patient will be given anticonvulsants. For the treatment of non-epileptic paroxysmal conditions, patients are prescribed medications.
Paroxysmal conditions in medical practice have not yet been sufficiently studied. Available data indicate a variety of pathologies, difficulties in diagnosing and treating paroxysms. At the moment, there are a number of conservative and surgical methods for the treatment of paroxysms, however, they still need to be improved to achieve a stable effect.