The brain is one of the most active consumers of blood in the human body. If nerve cells stop receiving blood rich in oxygen and nutrients, they can die within 5-7 minutes. Acute disruption of cerebral blood flow during a stroke is a serious condition that threatens a person’s life and can make him disabled.
Our expert in this field:
Tafintseva Ekaterina Anatolevna
Head of hospital, general practitioner
Call the doctor
But insufficient blood flow to the brain can also be chronic. This condition is called chronic cerebral ischemia, also called chronic cerebrovascular insufficiency, dyscirculatory encephalopathy.
Facts about chronic cerebral ischemia:
- Most often the disease occurs after 40-50 years.
- Currently, its prevalence is growing, as the population of developed countries is aging, and the prevalence of the main causes of dyscirculatory encephalopathy - arterial hypertension and atherosclerosis - is growing.
- At first, the disease leads to relatively mild symptoms, but over time it disrupts performance, turns a person into a disabled person, and leads to strokes.
- The most commonly affected artery is the carotid artery, which supplies blood to most of the brain.
To reduce the risk of serious consequences, treatment of ischemia should begin as early as possible. At the first symptoms - headaches, unsteady gait, fatigue, memory loss, poor sleep - you should immediately visit a doctor. Make an appointment with a neurologist at the medical office.
Treatment of cerebral vascular ischemia
The main treatment for cerebral ischemia is aimed at combating its causes – atherosclerosis and high blood pressure. A neurologist may prescribe the following medications:
- Drugs that lower blood pressure . There are different groups of them, they act differently. Proper treatment is one that helps to consistently maintain blood pressure at optimal levels. The doctor must select a combination of drugs individually for each patient.
- Antilipidemic agents . They help reduce the level of fat in the blood and prevent the growth of atherosclerotic plaques.
- Antiplatelet agents are drugs that prevent platelets from sticking together and forming blood clots. One of the popular antiplatelet drugs that doctors often prescribe to patients is aspirin.
- Antioxidants – ascorbic acid, tocopherol, eikonol.
Also, treatment of chronic cerebral vascular ischemia includes combating the symptoms of the disease. For increased fatigue, adaptogens and B vitamins are used. For anxiety, increased excitability, and sleep disorders, the doctor prescribes tranquilizers, anxiolytics, and sedatives. When memory and thinking are impaired, nootropic drugs (piracetam, Actovegin, etc.) help.
Lifestyle is also important. With discirculatory encephalopathy, you should not overwork, you need full sleep, and physical activity should be strictly dosed.
Take care of yourself, book a consultation now
Many people know what a stroke is and how dangerous this condition is. Nerve cells tolerate a lack of oxygen very poorly and die quickly. Chronic cerebral ischemia is a less famous, but no less dangerous condition. With it, approximately the same processes occur in the brain, but there are significant differences:
- The process is extended over time. Blood flow in the cerebral vessels is not suddenly disrupted. The activity of nerve cells decreases gradually. At first, a person is bothered by relatively mild symptoms, but over time they increase and severe complications develop.
- Unlike a stroke, with chronic ischemia in the brain there is not one focus in which many nerve cells died at once. The process is diffuse in nature, that is, it occurs not in one, but in many vessels, the entire brain suffers.
During cerebral ischemia, three stages are distinguished, each of which is characterized by certain signs.
Arterial hypertension and ischemic cerebrovascular accidents
L. A. Kalashnikova Professor, Doctor of Medical Sciences
Scientific Center for Neurology, Russian Academy of Medical Sciences
Arterial hypertension is one of the most common diseases. In Russia, about 40% of the adult population suffers from it. The danger of arterial hypertension is that it causes damage to the arteries of various organs, including the brain, which over time can lead to cerebrovascular accidents (CVA), both ischemic (cerebral infarction) and hemorrhagic (cerebral hemorrhage) . The insidiousness of arterial hypertension is that in some cases it is asymptomatic, not manifested by headaches or dizziness, as a result of which people often do not know that they have high blood pressure (BP) and do not take antihypertensive drugs. Sometimes in these cases they first learn about elevated blood pressure only after the development of cerebral urinary tract. Moreover, some people are aware of high blood pressure, but believe that there is no need to take antihypertensive drugs, since they feel satisfactory and do not suffer from headaches. Meanwhile, high blood pressure has a damaging effect on the walls of the arteries of the brain, changes in which over time can cause a stroke. It is also necessary to keep in mind that not only the absolute values of blood pressure are of great importance for damage to the arterial wall, but also the hemodynamic features of arterial hypertension: increased diastolic pressure, variability of systolic blood pressure, disruption of the circadian rhythm of blood pressure (absence of a physiological decrease in blood pressure at night or its increase , episodes of excessive nocturnal decrease in blood pressure). In connection with the latter, even moderate arterial hypertension requires timely correction, as it can lead to cerebral complications.
In arterial hypertension, small arteries (with a diameter of less than 500-800 microns) that supply blood to the deep parts of the cerebral hemispheres (white matter, internal capsule, subcortical ganglia) are predominantly affected. This selectivity of damage is due to the peculiarities of the anatomical structure of the arterial system, due to which it is the wall of small arteries in the deep regions of the brain that experiences the greatest pressure and undergoes the greatest destructive changes.
Damage to the cerebral arteries during arterial hypertension leads to the development of small deep-lying (lacunar) cerebral infarctions. Clinically, they are manifested by a special type of stroke - lacunar stroke. It has a number of distinctive clinical manifestations: preservation of consciousness in the acute period, absence of symptoms of damage to the cerebral cortex (disorders of speech, writing, etc.), good recovery of impaired functions over time. Lacunar infarctions are clearly visible on magnetic resonance imaging in the form of small, deeply located foci of ischemia no larger than 1 cm in size, rarely 1.5 cm. The further course of vascular pathology is determined by the prevalence of damage to the cerebral arteries and treatment tactics. If a person who has suffered a lacunar stroke does not have clinical symptoms of diffuse brain damage (decreased memory, bilateral increase in muscle tone, difficulty controlling pelvic functions) and there are no signs of diffuse brain damage on tomograms, then the prognosis is usually favorable provided that secondary medical treatment is performed. prevention. If the patient has clinical and tomographic signs of diffuse brain damage, then after suffering a lacunar stroke they most often gradually increase.
Arterial hypertension is the cause not only of acute ischemic cerebrovascular accidents (lacunar infarctions), but also of gradually progressive insufficiency of blood supply to the brain, leading to the formation of vascular (dyscirculatory) encephalopathy. Its development is associated with widespread damage (arteriolosclerosis) of arteries with a diameter of less than 150-200 microns, supplying blood to the white matter of the cerebral hemispheres and subcortical ganglia, which leads to their ischemia. Clinically, encephalopathy is manifested by cognitive impairment (primarily, memory loss), changes in gait (slowing, shuffling, unsteadiness), blurred speech, less commonly, choking when swallowing, difficulty controlling urination. The development of speech disorders of the aphasia type is uncharacteristic, since the cerebral cortex remains relatively intact, and the main changes are localized in the deeper parts of the cerebral hemispheres. Symptoms of encephalopathy may increase gradually or appear for the first time after a lacunar stroke. Neuroimaging - X-ray computed tomography or magnetic resonance imaging of the brain - is of great importance in the diagnosis of vascular (dyscirculatory) encephalopathy. It reveals diffuse changes in the white matter of the cerebral hemispheres (termed “leukoaraiosis”), small lacunar infarctions (often asymptomatic), and dilation of the cerebral ventricles. In everyday life, patients with dyscirculatory encephalopathy are often interpreted as suffering from sclerosis, although they are not characterized by atherosclerotic lesions of the main arteries of the head with occlusion or severe stenosis of their lumen.
Primary and secondary prevention of acute and chronic progressive vascular diseases of the brain in arterial hypertension consists of timely detection of elevated blood pressure and its correction. For this purpose, various groups of antihypertensive drugs are used: inhibitors of angiotensin-converting enzyme and its receptors, calcium channel blockers, diuretics, beta blockers, alpha blockers. It must be borne in mind that one should not reduce blood pressure below the “working” level, since in conditions of a narrowed lumen of intracerebral arteries (arteriolosclerosis), this can increase cerebral ischemia through the mechanism of cerebrovascular insufficiency and lead to an increase in focal neurological symptoms, the appearance of general weakness and dizziness. Patients also need to be prescribed complex drugs that improve blood circulation and nutrition of the brain (Cavinton, etc.), and drugs that improve the rheological properties of the blood, since with arterial hypertension there are pronounced circulatory disorders in the small vessels of the brain.
The effectiveness of drugs that normalize blood circulation in brain tissue has been confirmed by numerous studies. For decades, doctors around the world have been using them to reduce complications of vascular diseases. In order for the drugs to have maximum effect, it is necessary to exclude the influence of negative factors. Smoking, excessive alcohol consumption, foods rich in cholesterol, increased mental stress - all this negatively affects the condition of blood vessels.
For hypertensive encephalopathy, the drug Cavinton is prescribed, which has a complex effect. It helps normalize vascular tone, ensures blood delivery to areas of the brain with insufficient blood circulation, improves blood fluidity, as well as nutrition and energy supply to the brain in conditions of insufficient blood circulation by increasing the delivery and absorption of glucose and oxygen by nerve cells - substances necessary for their normal functioning . A lack of these substances can lead to the death of neurons responsible for memory and thinking. The consequence of this is a progressive weakening of memory and attention. Course use of Cavinton and Cavinton forte in the form of solution and tablets in this category of patients is accompanied by restoration of memory functions, positive changes in the emotional-volitional sphere, reduction of weakness, dizziness, and unsteady gait. During a course of treatment with Cavinton, a noticeable improvement in physical, mental and social functions and quality of life is achieved.
One of the important aspects of the treatment of cerebrovascular disorders in patients with arterial hypertension is the treatment of headaches. It should be noted that it is not always associated with an increase in blood pressure, but may be due to a decrease in cerebral vascular tone, which responds well to treatment with Cavinton Forte. In case of cerebrovascular insufficiency, including arterial hypertension, Cavinton Forte is taken 1 tablet 3 times a day after meals, for 3 months, with a repeat course of treatment after six months. Antidepressants can help with so-called “tension headaches.”
Timely detection, comprehensive treatment, regular monitoring and normalization of blood pressure, correction of cerebrovascular insufficiency in arterial hypertension are the key to preventing such serious complications as stroke and cerebral infarction.
Symptoms of cerebral ischemia in adults at the first stage of the disease
Typically, at the onset of the disease, patients present the following complaints:
- Headaches and dizziness.
- Increased fatigue.
- Feeling unsteady while walking.
- Weakness, heaviness in the head.
- Sleep disorders.
- Frequent, causeless mood swings.
- Deterioration of memory and attention.
During the examination and examination, the doctor may detect mild disorders.
Treatment is best started at this stage. Proper therapy can greatly reduce symptoms or get rid of them completely. Make an appointment with a neurologist and a medical examination.
Signs of cerebral ischemia at the third stage
Over time, the disease turns a person into a disabled person:
- Intellectual functions are impaired: abstract thinking, reading, counting, memorizing and reproducing information, etc.
- Facial expressions become sluggish.
- Walking slows down.
- The gait becomes uncertain, coordination of movements is significantly impaired.
- Falls and fainting are observed.
Many patients suffering from cerebral ischemia at the third stage have already suffered a stroke or an attack of transient ischemic attack (sometimes more than once).
Causes of illness in newborns
One of the serious childhood pathologies is ischemia.
Until today, medicine has not found effective drugs to get rid of the disease. The causes of the disease in children and adults vary significantly. Cerebral ischemia in newborns is a consequence of hypoxia that occurs in the prenatal state or during childbirth. Quite often the disease develops in infants whose mothers are over 35 years old.
The main factors provoking the disease:
- multiple pregnancy;
- toxicosis in the later stages, which occurs in a severe form and is accompanied by an increase in pressure and the presence of protein in the urine;
- placental abruption;
- illnesses and bad habits of the mother;
- the birth of a baby earlier or later than the due date;
- disruptions in the uteroplacental circulation, which provokes necrosis of parts of the baby’s brain;
- heart defects in a child.
In medicine, there are three degrees of severity:
- Mild stage of ischemia. You can observe a pronounced depressed state in the baby. Or, conversely, strong excitement, which lasts up to five to seven days.
- Moderate degree of ischemia. This form is usually accompanied by seizures in newborns. Such symptoms can be observed in a child for quite a long period.
- Severe ischemia. These babies are immediately placed in the intensive care unit.
No matter how scary the diagnosis of “cerebral ischemia” may sound, treatment carried out by modern medicine allows us to achieve significant success. The main directions are the restoration of blood circulation in the brain and the creation of conditions for the full functioning of areas unaffected by the disease.
The main thing to remember is that only an experienced doctor can evaluate all the signs and choose the right treatment methods to minimize the consequences. In milder cases, timely adoption of measures will completely eliminate hypoxia in the newborn’s brain.
How does the disease progress?
Over time, if proper treatment is not carried out, signs of cerebral vascular ischemia increase. The rate of progression of the disease can be different - sometimes slow and sometimes rapid. A rapid increase in symptoms is typical in cases where the disease began in youth, especially if the person suffers from high blood pressure.
Sometimes, if the disease can be “caught” at the first stage, it can be completely cured. In other cases, thanks to treatment, it is possible to significantly slow down the increase in symptoms, maintain the ability to work, and the ability to live an active life.
We will call you back
Leave your phone number
There are two main reasons for the development of chronic cerebral ischemia:
- Atherosclerosis is a condition in which cholesterol plaques form on the walls of the arteries. They narrow the lumen of the vessel and lead to impaired blood flow.
- Arterial hypertension is a disease in which there is a sustained increase in blood pressure greater than 140/90 mm. Hg Art. In most cases (more than 90%), essential hypertension is detected, which occurs as an independent disease. In less than 10% of patients, increased blood pressure is caused by pathologies of other organs, such as the kidneys.
Third stage
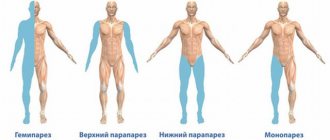
It is distinguished by a clear manifestation of neurological syndromes. In this case, there is a disturbance in walking and the ability to maintain balance (the patient may often fall). Urinary incontinence is observed, and parkinsonian syndrome is also characteristic. Due to the absence or decrease in a sober understanding of what is happening to the patient, the volume of his complaints decreases.
Personality disorders can manifest themselves as inhibited reactions, explosive states, apathetic-abulic symptoms and psychological abnormalities. In addition to neurodynamic (or dysregulatory) disruptions in the cognitive sphere, the manifestation of such operational disorders as speech and memory impairment, decreased thinking ability, etc. is possible. All these symptoms can later develop into dementia. The latter leads to an inability to quickly adapt to a new situation and to a drop in performance in personal, social and professional areas of life. Very often, doctors indicate a person’s inability to work. At a certain point, the patient stops caring for himself.
What happens in the brain during chronic ischemia?
During ischemia, oxidative stress develops in brain cells, free radicals accumulate in them, which cause their damage and death. The metabolism in the brain tissue is disrupted, the function of neurons decreases - this process does not happen unexpectedly, in a couple of minutes, but gradually, it is extended over time.
A phenomenon arises that can be called a “vicious circle.” Impaired blood flow leads to damage to nerve tissue, and because of this, in turn, the nervous regulation of blood flow deteriorates.
At the beginning of the disease, blood flow may be impaired in only one or two cerebral vessels, but gradually the pathological process covers more and more cerebral arteries. The vascular network is developed differently in different people. In some people, the cerebral vessels have many “spare bypasses” - they can compensate for blood flow disturbances for a certain time, the disease in this case progresses more slowly. If there are few such workarounds, the symptoms increase faster.
Types of disease
There are several types of vascular ischemia:
- Transient ischemic attack of blood vessels. This is an acute and reversible process characterized by a sudden disruption of blood circulation to the brain. The condition does not reach the level of a stroke, so it is classified as a separate subtype. As a rule, the duration of a transient ischemic attack does not exceed 60-90 minutes. Mostly patients with cerebral atherosclerosis and compression of the main arteries (carotid, vertebral) suffer.
- Chronic vascular ischemia. This type of cerebral pathology is characterized by a slow progressive disruption of blood supply to the brain, which leads to a gradual increase in neurological disorders. Previously, this disease was called “dyscirculatory encephalopathy.” Chronic cerebral ischemia appears in people suffering from atherosclerosis, blood clots and diseases that are accompanied by disturbances in blood properties, such as viscosity. Over a long period of time, first small and then large foci of gliosis form in the brain. It mainly occurs in the basal ganglia region.
What risk factors increase the likelihood of developing the disease?
The causes of cerebral ischemia are atherosclerosis and high blood pressure. The risk of these conditions is increased if the following conditions are present in a person's life:
- Sedentary lifestyle.
- Heredity: if similar pathologies were diagnosed in close relatives.
- Unhealthy diet: excess animal fats and sugar in the diet.
- Overweight, obesity.
- Smoking, excessive drinking.
- Age over 45-55 years.
- Men suffer from cardiovascular diseases more often than women.
Even if you are healthy, but some of these risk factors are present in your life, it would be a good idea to visit a therapist or neurologist. The doctor will examine you, order an examination and recommend regular screening programs that will help diagnose the disease in a timely manner.
Get a consultation with a doctor
For treatment of chronic cerebral ischemia to be effective, it must be started as early as possible. It is important to establish the correct diagnosis in time, and this is not always easy.
Causes and symptoms of the disease
Ischemia of cerebral structures is attributed to age-related changes, as a result of which the vessels lose their elasticity and become fragile. Vessels affected by atherosclerosis have a narrowed lumen in the cavity due to fatty deposits on the walls, thereby disrupting the flow of blood.
The causes of chronic cerebral ischemia can be caused by concomitant pathologies of the cardiovascular and endocrine systems.
Accompanying illnesses:
- Failure of heart rhythm (tachycardia, bradycardia);
- Systemic vasculitis (inflammation of the walls of blood vessels with subsequent destruction);
- Diseases of the venous system (phlebitis, varicose veins, obliteration);
- Pinched blood vessels (osteochondrosis of the cervical spine);
- Diabetes;
- Cerebral amyloidosis (disorder of protein metabolism with deposition of amyloid in tissues);
- Hereditary angiopathy (narrowing of small vessels or complete blockage);
- Autoimmune diseases (production of antibodies leading to the destruction of healthy tissue);
- Blood clot formation;
- Persistent increase or decrease in blood pressure (hypertension, hypotension);
- Osteochondrosis.
Chronic ischemia is more often of mixed etiology and occurs in a leukoencephalopathic or lacunar form. The leukoencephalopathic form is characterized by bilateral diffuse damage to the white matter, caused by persistent disorders in hypertension. The lacunar form is expressed by numerous foci due to damage to small vessels.
Chronic encephalopathy reduces the brain compensation mechanism, causing a malfunction of brain structures with an increase in pathological symptoms, which leads to irreversible processes.
Clinical manifestations of pathology in the initial phase of development can be mistaken for overwork. An increase in symptoms with damage to the white matter occurs in the phase of active progression of the disease.
Symptoms related to the manifestation of chronic ischemia:
- Migraine;
- Apathy;
- Unstable emotional background (mood swings);
- Noise in ears;
- Unstable blood pressure (possible hypertensive crisis);
- Speech impairment;
- Disorders of the musculoskeletal system (staggering gait caused by poor coordination);
- Loss of consciousness;
- Decreased sensitivity;
- Epileptic seizures;
- Damage to the motor pathway of the nervous system (paresis);
- Lack of voluntary movements (paralysis).
Chronic cerebral ischemia may have periods of temporary well-being with no symptoms.
Diagnosis of cerebral ischemia in a neurologist’s office. What happens during a doctor's appointment?
At the beginning of your appointment, the neurologist will ask you some questions:
- What symptoms bother you? When did they appear?
- Do you suffer from arterial hypertension, atherosclerosis, or other chronic diseases?
- How have your symptoms changed over time? Did they get stronger?
- What usually makes your condition worse?
- Do your symptoms interfere with your ability to work or cope with daily activities?
A full neurological examination will then be performed. The doctor will check the strength and tone of your muscles, reflexes, skin sensitivity, movements of facial muscles, and eyeballs. You will be referred to an ophthalmologist for a fundus examination.
At the initial stage of the disease, the neurologist may not detect any abnormalities at all, or they will be very weak.
Modern methods for diagnosing chronic cerebral ischemia
If cerebral ischemia is suspected, a neurologist may prescribe the following diagnostic methods:
- Fundus examination . Performed by an ophthalmologist. Already at an early stage of the disease, damage to the retinal vessels can be detected (which indicates a similar damage to the cerebral vessels), which intensifies over time.
- Blood pressure measurement . As a rule, it turns out to be elevated.
- Electrocardiography (ECG) . Changes characteristic of arterial hypertension are revealed.
- Dopplerography of cerebral vessels . Detects disturbances in the outflow of venous blood from the brain, narrowing of the lumen of blood vessels, and signs of sclerosis.
- Electroencephalography (EEG) . There are certain disturbances in brain activity.
- Computed tomography and magnetic resonance imaging . The images can reveal enlargement of the cerebral ventricles (a sign of hydrocephalus), areas of low density in the brain tissue. These methods do not always detect pathological changes during ischemia, so their results cannot be considered 100% reliable.
- Blood chemistry . Allows you to identify increased levels of “bad” cholesterol.
If necessary, your doctor may prescribe other diagnostic methods for you.
Antihypertensive therapy
Antihypertensive therapy is aimed at maintaining normal blood pressure and stabilizing the state of chronic ischemia. If doctors prescribe antihypertensive drugs, the patient should be careful and monitor for fluctuations in their blood pressure. As is known, in the case of developing chronic ischemia, the mechanism of autoregulation of cerebral blood flow begins to work intermittently.
If we talk directly about antihypertensive drugs prescribed by doctors, then first of all we are talking about medications of two groups:
- angiotensin-converting enzyme inhibitors;
- angiotensin II receptor antagonists.
Drugs of both the first and second groups are capable of simultaneously exerting two effects: in addition to angiohypertensive, they are also angioprotective, which means protecting the affected organs, which usually include the kidneys, heart and brain. The effect of antihypertensive drugs usually increases significantly when they are combined with antihypertensive drugs such as hydrochlorothiazide and indapamide.