Causes of disruption of the pituitary gland (weakening of hormone production): cerebral circulatory disorders (strokes); massive blood loss; tumor processes or metastases; skull injuries; surgical treatment of brain pathologies, radiation therapy; severe course of viral diseases, infections; encephalitis, meningitis; late toxicosis of pregnancy; autoimmune inflammation; congenital hypoplasia of the pituitary gland.
The main reason for the increased formation of hormones is adenoma.
Disturbances in the functioning of the pituitary gland can be caused by a tumor, vascular diseases of the brain, trauma, surgery, blood loss, and congenital developmental anomalies. They manifest themselves in the form of insufficient or excessive production of hormones. In patients, growth, functioning of the reproductive and thyroid glands, kidneys, adrenal glands, milk secretion, and labor in women change. Men suffer from impotence and loss of libido.
The pituitary gland has two parts - anterior (adenohypophysis) and posterior (neurohypophysis). The first produces: prolactin, somatotropin, thyrotropin, adrenocorticotropic, gonadotropic hormones. Vasopressin accumulates in the posterior part, and melanocyte-stimulating factor is synthesized in the intermediate cells, which is responsible for skin color and adaptation of the eyes to darkness. These properties of pituitary tropic hormones are among the main ones. A deficiency or excess of any of them causes a chain of pathological reactions in the body. Often diagnosed with infertility, emaciation or obesity.
Symptoms of pituitary gland dysfunction in women and men vary in variety. All pathological conditions, depending on changes in function, are divided into: with a decrease in the formation of hormones :
- hypopituitarism (Simmonds and Sheehan syndrome), pituitary dwarfism, diabetes insipidus;
- with increased hormonal synthesis : acromegaly, gigantism, Itsenko-Cushing's disease, hyperprolactinemia.
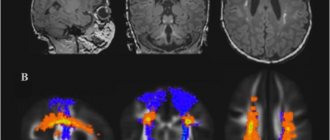
Diagnosis of the condition includes: blood and urine tests for hormones, radiography of the skull bones, MRI and CT, PET of the brain, angiography to detect vascular disorders, tests with liberins of the hypothalamus, as they control the functioning of the pituitary gland.
PET CT scan of the brain with methionine
To assess the functioning of target organs, it is necessary to determine sex, thyroid hormones, and cortisol in the blood.
For hormonal deficiency, replacement therapy with pituitary hormone analogues is used. If a tumor is detected, drug, radiation or surgical treatment may be chosen. They are often used in combination. One alternative method is to freeze part of the gland using a catheter that is passed through the sphenoid bone at the base of the skull.
Read more in our article about dysfunction of the pituitary gland, possible diseases, their symptoms and treatment.
Causes of pituitary gland dysfunction
The weakening of hormone formation can lead to:
- cerebral circulatory disorders - ischemic or hemorrhagic stroke;
- massive blood loss - at risk are women with frequent abortions, difficult childbirth, patients with ulcerative defects in the stomach, intestines, who have undergone trauma or extensive surgery;
- tumor processes or metastases;
- skull injuries;
- surgical treatment of brain pathologies, radiation therapy;
- severe course of viral diseases, malaria, tuberculosis or syphilitic infections;
- encephalitis, meningitis;
- late toxicosis of pregnancy;
- autoimmune inflammation;
- congenital hypoplasia of the pituitary gland.
The main reason for the increased formation of hormones is adenoma. Its cells are capable of hormonal production, while the remaining parts of the pituitary gland are compressed by the tumor, which leads to a significant decrease in other pituitary hormones.
We recommend reading the article about pituitary adenoma. From it you will learn about the causes of pituitary adenoma, symptoms of a brain tumor in men and women, classification of the disease, as well as the diagnosis and treatment of pituitary adenoma.
Find out more about the diagnosis and treatment of hypothyroidism here.
Effective treatments
Taking medications is ineffective while the tumor is in the pituitary gland tissues. Drug therapy to correct hormonal levels is prescribed after removal of a pituitary adenoma or other type of tumor. Depending on the size of the tumor, tumor tissue is removed through the nasal passages or craniotomy is performed.
With the active growth of all types of neoplasms and the appearance of a complex of negative signs, it is important to find out what factors provoke the rapid progression of the pathological process. Peripheral and local symptoms disappear after a certain period after tumor removal, but relapses are possible if the provoking factors persist.
If the body size of prolactinoma, adenoma, thyrotropinoma, or other types of formations is small, and there are no local negative signs, radiation therapy is possible. Exposure to specific particles suppresses the growth of tumor cells. If the effectiveness of the method is low, surgery is prescribed to remove the tumor.
It is important to contact an experienced neurosurgeon: surgical intervention affecting pituitary tissue requires a highly qualified doctor and the correct selection of hormonal compositions after tumor resection.
Find out how acute adnexitis manifests itself in women and how to treat the inflammatory disease.
The reasons for increased estradiol in women and the normal levels of the hormone by age are written on this page.Go to https://fr-dc.ru/vnutrennaja-sekretsija/polovye/lechenie-kisty-bez-operatsii.html and read about the causes and treatment of ovarian cysts in women without surgery.
What diseases occur with changes
The pituitary gland has two parts - anterior (adenohypophysis) and posterior (neurohypophysis). In the first one is formed:
- prolactin (stimulates milk production during lactation);
- somatotropin (regulates growth);
- thyrotropin (provides synthesis of thyroid hormones);
- adrenocorticotropic hormone (activates the adrenal cortex);
- gonadotropic - follicle-stimulating and luteinizing (responsible for the formation of sex hormones, maturation of eggs and sperm).
Vasopressin accumulates in the posterior part, it retains water in the body and oxytocin, which increases uterine contractions and milk production. The intermediate cells synthesize melanocyte-stimulating factor, which is responsible for skin color and eye adaptation to darkness. These properties of pituitary tropic hormones are among the main ones. In addition to these, they have many additional functions. A deficiency or excess of any of them causes a chain of pathological reactions in the body.
Prolactin
With a decrease in education, women have poorly developed mammary glands, and milk production decreases or stops after childbirth. A pathological increase in the formation of the hormone causes galactorrhea - the flow of milk outside of pregnancy and childbirth, combined with menstrual irregularities.
Somatotropin
Growth hormone deficiency leads to dwarfism (pituitary dwarfism), growth retardation or gigantism, acromegaly with excess somatotropin.
Thyrotropin
With increasing concentration, it stimulates the formation and release of thyroxine and triiodothyronine into the blood by the thyroid gland, leading to hyperthyroidism and thyrotoxicosis. Low levels of thyroid-stimulating hormone cause hypothyroidism. This condition is more common and occurs when adenomas or destruction of cells of the anterior pituitary gland.
Adrenocorticotropic hormone
With its increased production, the release of the hormone of the adrenal cortex (cortisol), sex hormones (androgens, estrogens and progesterone) increases. Hypercortisolism syndrome (Itsenko-Cushing's disease) occurs. Low amounts of adrenocorticotropic hormone (ACTH) lead to adrenal insufficiency.
Since ACTH and cortisol are in an inverse relationship, in case of primary damage to the adrenal glands (Cushing's syndrome, cancer), ACTH is lower than normal.
Gonadotropic
Impaired formation of follicle-stimulating and luteinizing hormone in women leads to uterine bleeding and menstrual irregularities, and in men they provoke impotence and infertility, enlarged mammary glands (gynecomastia)
Vasopressin
With its deficiency, diabetes insipidus develops - urine is produced abundantly, excess vasopressin leads to fluid retention in the body and an increase in edema.
Oxytocin
A decrease in hormone synthesis slows down labor, inhibits contractions, leads to postpartum bleeding due to insufficient contraction of the uterus, and disrupts the activity of the mammary gland when feeding the baby.
Diagnostic measures
An endocrinologist is involved in the diagnosis and treatment of pathologies of the pituitary gland. Diagnosis begins with an initial examination and interviewing the patient about what problems are bothering him. If the mammary glands are enlarged and milk is released from the nipples when palpating the breast, this indicates an excess of the hormone prolactin in the blood. Then a medical examination is prescribed, which consists of laboratory and instrumental examination.
Before checking the presence and level of certain hormones in the blood, it is necessary to conduct hardware tests to find out which part of the pituitary gland is damaged.
Instrumental diagnostic methods – brain ultrasound, CT and MRI. Magnetic resonance imaging allows you to determine all possible pathologies of the pituitary gland, its structure and size. This examination method increases the accuracy of diagnosis to 95-98%.
Cysts and adenomas are clearly visible on MRI images. If they are detected, a CT scan using contrast agents is additionally prescribed. Modern MRI equipment is able to detect the slightest changes in the size of the lower appendage of the brain.
A visual examination of the patient and the results of hardware diagnostics through computed tomographic analysis and MRI also give the endocrinologist the opportunity to determine which hormones need to be tested for by drawing blood. In addition, to determine the presence of inflammatory and infectious processes in the pituitary gland, a puncture of cerebrospinal fluid from the lower back is prescribed. This analysis allows you to identify diseases such as meningitis, encephalitis, etc.
Symptoms of pituitary gland dysfunction in women and men
The clinical symptoms of pituitary diseases are characterized by a variety of signs. This is due to the proximity of cells responsible for different vital parameters and the important role of tropic hormones in the regulation of the endocrine system.
All pathological conditions, depending on changes in function, are divided into:
- with decreased hormone production: hypopituitarism (Simmonds and Sheehan syndrome), pituitary dwarfism, diabetes insipidus;
- with increased hormonal synthesis: acromegaly, gigantism, Itsenko-Cushing's disease, hyperprolactinemia.
Watch the video about hormonal levels and the pituitary gland:
Simmonds syndrome
The formation of all pituitary hormones is disrupted, which is accompanied by the development of the following symptom complex:
- sudden weight loss with loss of subcutaneous fat, volume of muscle tissue and reduction in the size of internal organs;
- decreased sweat secretion, dry and wrinkled skin of a gray-sallow color, blueness of the fingers;
- teeth decay and hair falls out;
- in children, growth slows down (dwarfism), the formation of sexual characteristics, and mental development;
- in men – low potency and libido, hair loss on the chin, in the pubic area, armpits, the size of the prostate and external genitalia decreases;
- in women, menstruation stops, the mammary glands and uterus atrophy, nipple pigmentation disappears;
- due to low levels of thyroid hormones, lethargy, muscle weakness, drowsiness, constipation appear, the pulse slows down and blood pressure drops, body temperature decreases;
- a decrease in ACTH is accompanied by hypotension, weak immunity, and a drop in blood sugar concentration;
- from the nervous system - low motor and mental activity, apathy, depressive reactions, rapid aging, radiculitis with severe pain, polyneuritis, convulsions.
Sheehan syndrome
Occurs after childbirth or abortion with severe blood loss. In patients, milk production stops, menstruation decreases or completely disappears. There is swelling of the body, weakness, low activity, and drowsiness. The skin loses its elasticity, hair falls out, and nails become brittle. Patients report frequent dizziness and fainting.
Sheehan syndrome
Pituitary dwarfism
Violation of somatotropin formation leads to inhibition of growth and formation of internal organs. Accompanied by:
- a lag in the development of the muscular and skeletal system, the maximum height of patients reaches 120-130 cm in adulthood;
- underdevelopment of the genital organs, heart, lungs, kidneys, liver;
- low blood pressure, bradycardia;
- mental development is close to normal, the emotional sphere is close to youthful.
Diabetes insipidus
Patients have severe thirst and excessive urine production, which disrupts sleep. The volume of fluid loss can reach 5-20 liters per day. If the patient tries to drink less and reduce urination, this leads to severe dehydration.
Acromegaly
Appears in adults in the form of enlargement of the nose, ears, lower jaw, lips, disproportionately large arms and legs. Due to high levels of growth hormone, patients report pain in bones and joints, headaches, impaired vision, functioning of the heart, lungs, and genital organs. Patients are often diagnosed with malignant and benign tumors.
Gigantism
If growth hormone is produced in excess before the end of ossification of the skeleton, then the growth of children is ahead of their peers and reaches more than 2 meters in adolescence. At the same time, the head seems small, and the limbs seem disproportionately long. Patients have mental disorders, metabolic processes, and sexual function. Often infertile.
Dysfunction of the pituitary gland (gigantism)
Itsenko-Cushing's disease
Characteristic manifestations are:
- red moon-shaped face;
- stretch marks on the skin;
- obesity;
- increased hair growth on the body and face;
- darkening of the skin in the elbows, neck and areas of friction with clothing;
- arterial hypertension;
- osteoporosis with frequent fractures.
Hyperprolactinemia
With an increase in the formation of prolactin in women, the menstrual cycle is disrupted, such as scanty periods (oligomenorrhea) or their absence (amenorrhea). Following this, milk-like drops begin to be released from the mammary glands of nulliparous women, and hair growth on the body and chin increases. Nipple discharge also occurs in men. They are characterized by impotence and low libido, enlarged mammary glands. Excess prolactin leads to infertility in both sexes.
Watch the video about hyperprolactinemia:
Hypofunction of the anterior pituitary gland
This condition is associated with complete or partial loss of function of the adenohypophysis and, consequently, with a decrease in the release of corresponding tropic hormones. With total hypofunction, severe cachexia and dysfunction of the peripheral endocrine glands are observed (growth retardation, hypogonadism, hypothyroidism, decreased blood pressure up to collapse, muscle weakness). In advanced cases, exhaustion reaches an extreme degree.
Atrophy of the pituitary gland, accompanied by severe cachexia, is observed during prolonged starvation, especially protein starvation. One of the options for such total hypofunction of the anterior pituitary gland is psychogenic (nervous) anorexia . This syndrome occurs in neuroses, psychopathy, schizophrenia, and in mentally healthy people (usually women) with an excessive desire to meet modern fashion standards and for this purpose following a strict diet aimed at sharply reducing body weight.
With insufficient production of any one or more tropic hormones of the adenohypophysis, diseases such as pituitary dwarfism (from the Greek nanos - dwarf), or dwarfism (short stature), and pituitary hypogonadism occur.
Pituitary dwarfism based on genetic disorders, trauma during childbirth, tumors of the central nervous system, which is accompanied by damage to the hypothalamus and hypofunction of eosinophilic cells of the anterior pituitary gland. In pituitary dwarfism, the leading mechanism is a deficiency of somatotropic and gonadotropic hormones.
Patients with pituitary dwarfism are short in stature. It is generally accepted that dwarf height in women is below 120 cm, and in men below 130 cm. Adult dwarfs retain the body proportions characteristic of younger children, with a predominance of the length of the body over the length of the limbs. The facial features of adult dwarfs are similar to those of children, and the characteristic appearance of an “old-looking youth” arises. The muscular system is underdeveloped. Intelligence is usually not affected.
Another form of hypofunction of the anterior pituitary gland associated with gonadotropin deficiency is pituitary hypogonadism. It manifests itself in men as eunuchoidism, and in women as infantilism.
Specific signs of pituitary eunuchoidism are expressed in the underdevelopment of the gonads, external genitalia and secondary sexual characteristics.
Female infantilism is characterized by a slender build without pronounced signs characteristic of an adult female body.
Treatment consists of replacement therapy with appropriate sex hormones.
Diagnosis of the condition
To examine patients, the following is prescribed:
- blood and urine test for hormones;
- radiography of the skull bones;
- MRI and CT, PET of the brain;
- angiography to detect vascular abnormalities;
- tests with liberins of the hypothalamus, as they control the functioning of the pituitary gland.
Positron emission tomography of the brain
To assess the functioning of target organs, it is necessary to determine sex, thyroid hormones, and cortisol in the blood.
Complications
Diffuse heterogeneous changes in the pituitary gland can lead to complications such as:
- hormonal imbalance ;
- when enlarges, compression of nearby structures occurs;
- cerebral ischemia
- development of epilepsy;
- progression of visual up to blindness;
- development of diabetes mellitus;
- changes in the structure of other endocrine organs.