Symptoms of a brain tumor in children
The limited internal space of the skull is reserved only for the brain and there is no room for anything else. Therefore, as brain tumors grow in children, excess intracranial pressure is created in the skull. This pressure can also be created by obstructing the flow of cerebrospinal fluid in the brain.
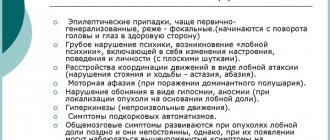
Associated symptoms include:
- Headache;
- Seizures;
- Nausea and vomiting;
- Irritability;
- Lethargy and drowsiness;
- Changes in the patient’s character and mental activity;
- Macrocephaly (increase in head volume) in children whose skull bones have not yet fully fused;
- Coma and death if untreated.
Other symptoms may also appear, for example, with a tumor in the cerebellum, children may experience difficulty moving, walking, and coordinating. When a tumor arises near the optical pathways, visual changes may occur.
First symptoms
Symptoms that occur in the first stages of the disease do not allow one to draw an unambiguous conclusion about the presence of a tumor. After all, the first signs are similar to symptoms that are observed in other diseases:
- headache, which increases with physical activity, but which subsides if the person is in an upright position;
- nausea , which occurs at any time, regardless of the time of eating, and the person’s well-being does not improve after vomiting;
- decreased concentration , impaired coordination of movements, weakened memory;
- epilepsy attacks , convulsions.
The manifestation of these symptoms indicates the presence of a tumor, which at this stage is treatable. However, such symptoms are rarely “listened to.”
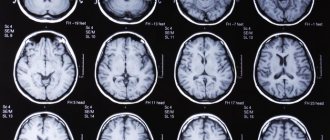
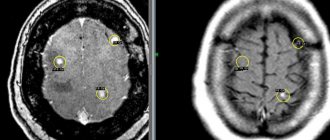
Diagnosis of brain tumors
Children who exhibit symptoms consistent with a brain tumor should be carefully examined by a pediatrician or pediatric neurologist to find the cause of the problems.
The examination usually includes a magnetic resonance scan of the brain and if it shows the presence of a tumor, the patient is sent to a consultation with a pediatric neurosurgeon, whose task is to develop, together with the child’s parents, the most effective treatment method.
Other specialists may also be involved for consultations:
- Pediatric oncologists;
- Ophthalmologists;
- Doctors who specialize in epilepsy (to treat seizures);
- Radiologists;
- Specialists in functional diagnostics.
To develop the right treatment plan for a child with a brain tumor, the surgical team needs information about:
Tumor location
This can be determined using computed tomography or magnetic resonance imaging. Such information is necessary because There are areas of the brain where surgery is impossible. The scan allows you to evaluate the possibility of surgical treatment.
Tumor type
To do this, sections of tumor tissue are examined under a microscope. Not knowing this information allows you to assess how the tumor will develop and spread.
Tumor class
The higher the class, the more aggressive the tumor will behave and spread at a faster rate.
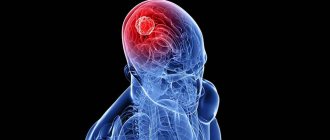
Types of brain tumors in children
Brain tumors can be classified as:
- Primary, that is, those that arose directly in the brain.
- Metastatic, which arose as a result of metastases from tumors of other organs entering the brain.
- Benign, non-cancerous, growing rather slowly.
- Malignant, cancerous. These tumors can be very aggressive and spread quickly to other parts of the brain.
Below we look at some common types of brain tumors in children.
Astrocytoma. Astrocytomas account for about half of all childhood brain tumors and most often appear between the ages of 5 and 8 years. Tumors of this type develop from glial cells and astrocytes. For these tumors, it is very important to know their growth rate (although 80% of them are slow-growing).
There are 4 main types of astrocytomas in children:
- Pilocytic astrocytoma (grade 1). These tumors are filled with fluid and grow very slowly. When these tumors occur in the cerebellum, surgery is necessary.
- Diffuse astrocytoma (grade 2) invades adjacent parts of the brain, making surgery to remove it quite difficult.
- Anaplastic astrocytoma (grade 3) is a malignant tumor that requires combined treatment.
- Glioblastoma multiforme (grade 4) is the most malignant of all types of astrocytomas.
Children may also experience:
- Brain stem glioma;
- Tumor of the choroid plexus;
- Craniopharyngioma;
- Tumor of germ cells;
- Medulloblastoma;
- Optic nerve glioma.
Causes
There is an assumption that malignant neoplasms appear in children due to the inability of the immune system to prevent the harmful effects of carcinogens.
Genetic transmission of the gene from close relatives is not excluded.
Is there a connection between cell phones and brain cancer - one of the most discussed issues of our time
Risk factors:
- ionizing, ultraviolet and radiation radiation;
- chemicals (chromium, arsenic, formaldehyde);
- vinyl chloride gas, used in the production of plastics;
- sugar substitute aspartame;
- herbicides, pesticides;
- solar radiation;
- electromagnetic fields emitted by mobile phones;
- regular consumption of smoked meats and store-bought sausages;
- intrauterine developmental defects;
- Some viruses can cause abnormalities in the body.
Treatment
Your treatment plan for pediatric brain tumors may include one or more of the following:
Surgical intervention
This method must be resorted to in almost all cases, either to remove a tumor or to perform a biopsy. For slow-growing tumors, this is the only treatment needed.
Radiation therapy
In this case, a narrow beam of high-energy radiation is directed at the tumor and a small area of neighboring tissue. For the treatment of children under 3 years of age, this method is used with great caution due to the risk of interfering with brain development.
Chemotherapy
This treatment method is used quite widely, especially in the case of aggressive, fast-growing tumors. Chemotherapy drugs can be taken orally, injected into a vein, into the cerebrospinal fluid, or directly into the cavity left by surgery.
Classification
There are many options for classifying pathology.
Tumors are classified according to their method of occurrence:
- primary (formed from brain structures);
- secondary (metastases are “carried” into the skull by lymph or blood from organs affected by a malignant neoplasm).
The source of secondary formations most often are metastases of the breast, lung, kidney, colon and skin melanoma.
Depending on what kind of brain tissue began to grow, there are:
- neuroepithelial neoplasms;
- formations from the nervous tissue itself;
- meningeal tumors (tumors from the membranes of the brain);
- pituitary tumors.
Cancerous brain tumors are divided into 4 stages, and the classification is based on the extent of metastases. To determine the stage of the process, not only the size of the tumor is taken into account, but also the presence of metastases, which is designated by the letter M. This information is presented in more detail in the table.
| Stage designation | Description of metastasis |
| M 0 | no cancer cells were detected |
| M 1 | cancer cells are registered in the cerebrospinal fluid (cerebrospinal fluid) |
| M 2 | metastases are localized only in the brain |
| M 3 | metastasis to the spinal cord is noted |
| M 4 | extraneural metastasis (metastases extend beyond the central nervous system, i.e. they can be in any part of the body) |
The basis of malignant processes is made up of neuroepithelial and secondary neoplasms. In this regard, the statistics are not reassuring: the incidence of secondary tumors is 7 times more common than primary ones.
Second opinion for brain tumors in children
Despite the fact that brain tumors are often quite well identified on MRI and CT, errors in the interpretation of scan results do occur.
This may be due to a number of reasons, including:
- Low accuracy of equipment (for example, an outdated tomograph or one with defects that arose during operation);
- Lack of sufficient experience of a CT and MRI specialist.
Moreover, medical errors do not always indicate low qualifications of the doctor. They can happen even to fairly experienced CT scanners who simply don't see rare tumors very often. For example, a brain test may go to a doctor who has more experience diagnosing the lungs or liver.
In this situation, the only option to avoid incorrect treatment (which could endanger the child’s life) is to get a second opinion from qualified radiologists. The National Teleradiological Network (NTRS) invites you to get a second opinion from leading specialists from the best clinics and institutes in the country, with just access to the Internet. It doesn’t matter how far you are, just upload the scan results to our server and within a day the primary diagnosis will either be refuted or confirmed.
NTRS is a simple way to reduce the risk of scanning errors to a minimum.