Subdural and epidural hematoma are formed as a result of rupture of intracranial vessels. This is a very life-threatening pathology, fraught with serious consequences, requiring qualified treatment and long-term rehabilitation.
The brain is covered by several membranes, the outermost of which, adjacent to the bone, is the dura mater. The hematoma located under it is called subdural, and above the membrane is called epidural (from the Latin durae matris - hard shell, sub means above, above, epi - under, below). Both types of hematomas can be located anywhere in the skull, have different sizes, and the patient’s condition and the choice of treatment methods depend on this.
Author of the article / Site experts Shulepin Ivan Vladimirovich, traumatologist-orthopedist, highest qualification category
Total work experience over 25 years. In 1994 he graduated from the Moscow Institute of Medical and Social Rehabilitation, in 1997 he completed a residency in the specialty “Traumatology and Orthopedics” at the Central Research Institute of Traumatology and Orthopedics named after. N.N. Prifova.
Subdural hematoma
Rupture of blood vessels and release of blood under the dura mater can occur for various reasons:
- during traumatic brain injury;
- as a result of rupture of abnormal vessels (aneurysm, malformation);
- with a sharp increase in blood pressure and artery rupture;
- in persons with reduced blood clotting;
- with inflammation of the meninges;
- in the presence of a tumor in the cranial cavity, compressing blood vessels;
- in a newborn child during difficult labor.
Blood pours into the space between the dura mater and the arachnoid membrane, it compresses the brain, as a result, intracranial pressure increases and the brain is compressed. With a large hematoma, a displacement of the hemispheres occurs. As a result, symptoms of a disorder of the central nervous system and vital functions develop due to compression of the respiratory and circulatory centers located in the brain.
The severity of these symptoms will depend on the nature of the hematoma, the mechanism and time of its formation. In this regard, there is the following clinical classification of subdural hematomas:
- Spicy.
- Subacute.
- Chronic.
The acute clinical form develops during the first 3 days after a stroke or other cause of vessel rupture. Subacute hematoma is considered to be from 4 days to 2 weeks. Chronic subdural hematoma sometimes may not manifest itself, or symptoms may be very mild, up to the development of complications - from 2 weeks to several months. Usually the volume of such a hematoma is small.
All signs of hematoma are divided into 2 groups: general cerebral and focal. General cerebral are associated with increased intracranial pressure and are manifested by headache, vomiting, confusion, even loss of consciousness, convulsions and coma may develop.
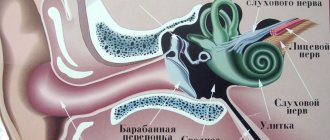
Focal symptoms depend on which part of the brain is compressed by the hematoma. Compression in the back of the head leads to imbalance and coordination of movements, in the frontal region - to blurred vision, dilated pupils, in the temporal region - hearing suffers, in the crown region - involuntary movements and sensitivity disorders occur. In general, the symptoms are very diverse and do not allow a diagnosis to be made without special examinations.
Characteristic symptoms
Subdural and epidural hematomas have some differences in symptoms. The most important thing is the presence and duration of the so-called “light” period after injury. With an epidural hematoma of the brain, there is such a period, after which a gradual or immediate loss of consciousness occurs. Subdural hematoma of the brain, in turn, is characterized by a consistently increasing headache and an increase in the person’s restlessness.
Location of the meningeal artery
General symptoms indicating the presence of a hematoma:
- dizziness;
- headache;
- weakness;
- memory loss (short-term or long-term);
- vomit;
- loss of consciousness;
- coma;
- increased blood pressure;
- excited state.
In addition, subdural hematoma of the brain is characterized by the following symptoms:
- slurred speech;
- paralysis;
- deterioration or loss of vision;
- convulsions;
- weakness in the limbs;
- numbness.
In addition, epidural hematomas also have symptoms characteristic only of this type, for example, dilation of the pupil and drooping of the eyelid, on the side where the hematoma is diagnosed. On the opposite side there is muscle weakness or pyramidal insufficiency.
Pyramidal insufficiency is a disorder of the pyramidal cells of the fifth layer of the cerebral cortex. It manifests itself in muscle hypertonicity, partial or complete paralysis of parts of the body, convulsions, and decreased reflex activity.
Epidural hematoma
This type of hematoma occurs as a result of a rupture of a vessel passing between the skull bone and the dura mater. Most often it is traumatic in nature - as a result of a blow to the head, a fracture of the skull bones, and can be more extensive and dangerous.
The peculiarity of clinical manifestations is an acute course, a short period of imaginary improvement - up to 2 days, after which a sharp deterioration occurs.
The patient is “loaded”—severe drowsiness, lethargy, and lethargy appear, which progress to loss of consciousness and cerebral coma. In children, such hematomas are especially dangerous due to insufficient hardness of the membrane and more pronounced compression of the brain.
There are 2 forms of hematoma:
- acute traumatic;
- chronic.
The acute form occurs in most cases, is associated with trauma and is characterized by a severe course. Chronic epidural hematoma is limited hemorrhage resulting from minor trauma or other cause of vessel rupture. Such a hematoma does not produce pronounced symptoms, becomes surrounded by a capsule and is often detected only during a tomographic examination.
Clinical manifestations
The clinical manifestation of a subdural hematoma has a slower onset than with an epidural hematoma, due to the lower rate of venous bleeding compared to arterial bleeding. A clearly defined “lucid gap”, which is classic for an epidural hematoma, may not be observed; the timing of the manifestation of symptoms varies extremely - both immediately after the injury, within a few minutes[11], and delayed, after two weeks[12]. In addition, in contrast to the classic “lucid interval,” changes in the state of consciousness in SDH are often wave-like and gradual [13].
When the volume of hemorrhage is sufficient to compress the brain, signs of intracranial hypertension or focal neurological symptoms due to damage to the medulla appear [3]. The clinical picture of SDH is extremely variable. In addition to the volume of the hematoma, its location, etc., the mechanism of injury of acceleration-deceleration with counter-impact is important, which often entails bilateral brain damage [13].
Impaired consciousness in SDH, in contrast to the manifestations of epidural hematoma, often develops not according to the stem type, but according to the cortical type, and may have amentive, oneiric manifestations, the development of “frontal” symptoms with decreased criticism, absurd behavior, etc. is typical. excitement, a typical wavy headache with a meningeal tint or a hypertensive nature, increased headache is accompanied by vomiting. Epileptic seizures occur, often generalized. In half of the cases bradycardia is observed. There are congestion in the fundus, with chronic SDH - with elements of atrophy of the optic nerve nipple. The combination of SDH with severe brain contusion can be accompanied by brain stem disorders such as respiratory and hemodynamic disorders, diffuse changes in muscle tone and reflex sphere [13].
Diagnostics
After collecting an anamnesis and examination, the patient is sent for a tomographic examination of the head: computed tomography - CT, which reveals the size, location and exact localization. Even more informative is MRI - magnetic resonance imaging of the brain; it allows not only to determine the exact parameters of hemorrhage, but also to obtain information about the functional state of brain tissue.
For young children, the most gentle ultrasound examination is echoencephalography (EEG). When a patient is admitted in serious condition, he is immediately sent for an emergency tomography.
Tomography makes it possible to differentiate epi- and subdural hemorrhages from a brain hematoma located in its tissue itself - an intracerebral hematoma.
If the patient’s condition allows, a contrast study of the vessels is performed - cerebroangiography, which makes it possible to identify which vessel is damaged.
Diagnosis of epidural and subdural cerebral hemorrhage
Diagnosis of an acute condition includes, first of all, visualization using CT of the brain, mainly in case of injury (to exclude a fracture); after neurosurgical interventions, visualization in the bone window is necessary. If the CT results are unclear or to assess the dynamics, it is advisable to perform an MRI of the skull.
Differential diagnosis
The differential diagnosis of EDH, as well as acute and chronic SDH, includes:
- Subdural or epidural emphysema, for example, after neurosurgical or ENT operations (often difficult to distinguish from hemorrhages; history and possible air inclusions help);
- Subdural hygroma (subdural accumulation of cerebrospinal fluid), for example, after traumatic or iatrogenic ruptures of the arachnoid mater, hyperdrainage during implantation of a shunt system or CSF loss syndrome, for example, after spinal cord or brain injury; when visualized, a “sickle-shaped” extracerebral mass effect with density or signal dynamics like cerebrospinal fluid.
Treatment
All patients, regardless of the type of hematoma, are hospitalized in the neurosurgical department. Medical tactics depend on the results of the examination: the nature, location and size of the hemorrhage, as well as on the condition of the patient. Treatment can be conservative or surgical.
Conservative treatment
For a small hematoma, when it does not tend to increase and does not cause significant compression of the brain and does not pose a threat to health, treatment consists of the following measures:
- bed rest;
- painkillers;
- antiemetics;
- diuretics to relieve swelling;
- cardiac and respiratory stimulants;
- sedatives;
- nootropics - drugs that improve cellular metabolism of brain tissue;
- B vitamins, vitamin and mineral complexes.
As a rule, after complex treatment, small hematomas resolve.
Surgery
The operation is indicated when the hematoma poses a threat to the patient's life. Traditionally, trephination (opening) of the skull is performed; for this purpose, milling holes are drilled through which the bone is filed to gain access to the shell. The blood is removed, drainage is installed for its outflow and control for 1 day, the membranes are sutured. The bone fits into place and grows together quite quickly.
Modern endoscopic technologies make it possible to operate on hematomas without detachment of a bone fragment, through a small hole, under the control of a video camera and display. This operation takes much less time than craniotomy and is less traumatic.
Rehabilitation
Damaged nerve tissue is restored very slowly, so the rehabilitation period is quite long.
It can last from several months to a year; in children, recovery is faster.
The body has the ability to heal itself. In this regard, you need not to interfere with him, and moreover, help him. To do this, you should give up smoking and alcohol, heavy physical activity, avoid stressful situations, and organize a nutritious diet with enough protein and vitamins.
During the entire rehabilitation period, you must regularly visit a doctor and take prescribed medications. These are mainly nootropics, vitamins, antispasmodics. Those who have disorders of movement, sensitivity, speech and other functions are sent for treatment to a rehabilitation center, where they receive massage, exercise therapy, and physiotherapeutic procedures.
Complete recovery with adequate treatment is measured not in days, but in months, and can take almost a year, provided that no complications develop.
Consequences and complications
The outcome of hematomas is not always favorable. Complications such as lethargy, weakness and muscle wasting, physical inactivity, decreased vision and hearing, impaired balance, swallowing, speech, and writing are common. There may also be mental disorders in the form of memory loss, dementia, and neuroses. Often a complication is a convulsive syndrome similar to epilepsy.
In young children, hematomas in the cranial cavity can lead to the development of cerebral palsy (CP), epilepsy, hydrocephalus, delayed intellectual development, and mental disorders.
Prognosis and prevention
Unfortunately, the prognosis for both life and health cannot be called favorable. According to statistics, the mortality rate is more than 50%, with epidural hematomas - up to 80%, and its main cause is swelling of the brain and the spread of blood in the medial direction with compression of vital centers - blood circulation and respiration.
As for the health prognosis, the consequences are also very common, but they can be prevented or reduced to a certain extent by strictly following the regimen prescribed by the doctor and performing all treatment procedures. Preventing the appearance of hematomas consists of preventing injuries, in particular sports ones - protecting the head with a helmet, especially in children “racing” a bicycle.
It is important to pay close attention to your health, regular examination and treatment of existing diseases, and timely consultation with a doctor in case of a head injury.
The main reason is injury
An epidural hematoma occurs due to a blow. In this case, there is the following classification:
- hit on the head with a small object;
- hitting the head directly against a traumatic object.
In addition to the temporal zone, the inferior parietal region is very often damaged. When a temporary deformation of the skull is formed, the vessels that are directly connected to the hard shell rupture.
This mechanism provokes the development of hematoma and cerebral edema.