Epidural hematomas of the brain are an accumulation of blood between the cranial bones and the dura mater of the brain resulting from traumatic injury. It is considered a rare type of hematoma: according to medical statistics, it accounts for no more than one and a half percent of cases.
The Neurosurgery Department of CELT invites you to undergo diagnostics and treatment of hematomas in Moscow. Our multidisciplinary clinic has been operating in the paid medical services market for the third decade and enjoys a good reputation among patients. Our specialists have many years of practical experience and have modern techniques that allow them to carry out effective and most gentle operations.
Etiology of epidural hematomas
As already mentioned, the formation of an epidural hematoma occurs above the dura cerebral membrane, which causes its detachment from the inner cranial surface. Since under the age of two years and after sixty it is fused to the cranial bones, during these periods this type of hematoma is extremely rare. Most often it is diagnosed in male patients aged sixteen to twenty-five years who lead an active lifestyle.
An epidural hematoma occurs due to traumatic injuries. This can be a blow from a small object to a slow-moving head, or a blow to the head against a stationary object, usually when falling. Most often, the injury occurs in the area of the temples or crown, and hemorrhage occurs from the meningeal artery and its branches.
Total information
The average blood volume that usually occurs in this condition is 120 ml, in some cases it can be reduced to 30 or even increased to a maximum of two hundred and fifty milliliters. The diameter of the hematoma is usually from 6 to 7 cm, and the main localization is the temporal region.
Unlike a subdural hematoma, where the bleeding is venous, an epidural hematoma develops due to arterial bleeding. It has one-sided localization and limited distribution. In children, due to the special anatomical structure, when the inner surface of the skull is fused with the dura mater, this pathology is very rare.
Epidural hematoma clinic
The diameter of the hematoma formed above the hard shell does not exceed eight millimeters, the volume is one hundred and twenty milliliters. Its peculiarity is that its thickness increases from the periphery to the center, and the danger is that it causes an increase in intracranial pressure and compression of brain tissue. The classic picture of hematoma formation is characterized by the presence of a clearly visible light interval, which lasts about half an hour and manifests itself as follows:
- The victim loses consciousness for a short period of time and then comes to, often maintaining an insignificant stunned state;
- He complains that he is dizzy, has a feeling of weakness and a headache of moderate intensity;
- He may experience a lack of symmetry in the nasolabial folds, as well as involuntary oscillatory movements of the eyeballs.
After this, the victim becomes worse, which is manifested by the following:
- Increased headaches;
- Depressed state of consciousness (sometimes comatose);
- Increased blood pressure;
- Facial nerve paralysis;
- Pupil dilation and lack of reaction to light.
Subacute form
This course of the disease is vaguely similar to the acute form. However, it is characterized by a number of individual symptoms:
- After about 20 minutes there is a light interval. Its duration is up to 12 days.
- Life support functions remain unchanged.
- In rare cases, a jump in blood pressure is observed.
- Symptoms are mild.
- The patient is fully conscious, less often slightly stunned.
- Bruises develop in the fundus.
After the end of the light period, the condition of the injured person deteriorates sharply.
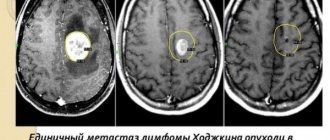
Diagnosis of epidural hematomas
In order to correctly make a diagnosis, CELT specialists conduct comprehensive studies to accurately determine the location, diameter and volume of the hematoma, as well as to determine its consequences. Instrumental diagnostic tests prescribed for the patient are presented as follows:
- X-ray of the skull to detect fractures;
- Cerebral angiography (study of cerebral vessels);
- Echoencephalography;
- Computer and magnetic resonance imaging, incl. and with contrast.
Source of bleeding
Having figured out how an epidural hematoma forms, it is easy to understand what exactly is the source of bleeding. During the strike, deformation of the skull occurs, which leads to rupture of blood vessels. The latter are closely related to the dura mater of the brain. Most often, deformation of the meningeal artery occurs. Less common are cases where bleeding occurs due to rupture of the diploe vessels and meningeal veins. Blood leaving them forms a hematoma, which can lead to cerebral edema.
Treatment of epidural hematomas
When developing treatment tactics for hematomas, neurosurgeons and neuropathologists are based on the results of diagnostic studies and individual patient testimony. It may involve the use of conservative or surgical techniques.
| Hematoma treatment methods | What are they? |
| Conservative | Conservative treatment is carried out for hematomas with a volume of up to 50 mm if there is no progressive clinical picture and there are no symptoms of brain compression. It involves the use of drugs to prevent cerebral edema, relieve pain, vomiting and convulsions. |
| Neurosurgical | Surgery is the more common treatment option. Removal of the hematoma is carried out using endoscopic techniques through a specially created hole in the skull. Through it, part of it is aspirated, after which they resort to trepanation and completely remove the hematoma. The neurosurgeon also locates and ligates the damaged blood vessel using various techniques. |
The Neurosurgery Department of CELT is staffed by neurologists and neurosurgeons with many years of experience in scientific and practical work. You can make an appointment with them online on our website or by contacting our operators: +7 (495) 788 33 88.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Causes of hematoma
In most cases, hematomas of this type are of traumatic origin. However, a pathological condition can also develop. It is caused by a rupture of a blood vessel. People suffering from a sharp increase in blood pressure are at risk.
So, let's figure out what can trigger the development of a disease such as an epidural hematoma. The causes of its occurrence are traumatic brain injury caused by a small object. These include a hammer, stick, stone. Upon impact, the affected area is relatively small. The development of a hematoma is influenced not only by the force of the blow, but also by the position of the head. If it is motionless, then the risk doubles. A blow to a fixed object can also lead to the formation of blood clots in the brain. That is, a person, while in motion or in a standing position, falls and hits a door, corner of a table or shelf.
As a rule, as a result of injury, the skull is locally deformed. A characteristic depression may appear in this place. When an impact occurs on the damaged area, the bone is pressed into the cranial cavity. This causes rupture of blood vessels, which leads to bleeding.
Therapy
Conservative treatment
If the volume of the resulting cavity does not exceed 30–50 ml, the patient does not experience progressive symptoms and signs of brain compression, conservative treatment is possible.
The main goal of therapy is the gradual resorption of the mass of spilled blood, and therefore it is vitally important to constantly monitor the dynamics of the hematoma volume.
Surgical intervention
For larger formations and the presence of brain compression, emergency surgical intervention is indicated. In such cases, a milling hole is made in the area of the skull with the expected localization of the accumulation.
The choice of treatment tactics is determined by the degree of damage and its location
Through it, using a special aspirator of blood clots and fluid, part of the hematoma is removed, after which craniotomy is performed to remove the formation in full and ligate the damaged vessel.
If veins are the source of bleeding, they are coagulated, followed by packing with a hemostatic sponge. In cases of damage to the diploic veins, surgical wax is used, and if sinus injuries are detected, their plastic surgery and tamponade are performed. At the end of the operation, a bone flap is put in place and the wound on the surface of the scalp is sutured.
Simultaneously with the manipulations, hemostatic, decongestant and symptomatic treatment is used. During the recovery period, patients receive neurometabolic and absorbable medications. To speed up the process of muscle recovery in paretic limbs, therapeutic massage and physical exercise are indicated.
Closed external drainage
As an alternative to craniotomy, a minimally invasive surgical intervention - closed external drainage - can be chosen. This method is recognized as more gentle and has a number of advantages, but can only be used in cases where emergency removal of the formation is not required.
According to indications, minimally invasive surgery is performed
An intraosseous needle is inserted through the skin to perforate the skull. A special drainage catheter, the diameter of which does not exceed 3 mm, is placed into the resulting hole. A fluid receiver is attached to it, which is placed 15–20 cm below head level to ensure optimal fluid outflow.
When carrying out minimally invasive therapy, the integrity of the cranium is not compromised, and the risk of infection and the likelihood of relapse of the pathology are minimal.
The light interval is weakly expressed
In severe traumatic brain injuries, the epidural hematoma occurs with a weakly defined light interval. In this form, the patient may fall into a coma with initial loss of consciousness. It lasts several hours. This is followed by the stage of stupor, and after this the patient goes into deep stupor. In this state, maintaining contact with the patient is quite problematic. Doctors observe disruption of life support functions. This form is characterized by the fact that a weakly expressed light interval can last several days. After which the patient again falls into a coma. He may develop paralysis. His condition becomes extremely serious.
Forecast and possible consequences
The prognosis for epidural hematomas directly depends on the patient’s age, the volume of the formation and the timing of the operation. The most favorable outcome is observed in the following cases:
- conservative treatment of small formations;
- performing surgical intervention at the stage of moderate decompensation. In this case, the probability of restoration of lost neurological functions is highest, and the risk of mortality is minimal.
When performing an operation at the stage of decompensation, the prognosis is the least positive. Craniotomy is fatal in 40% of cases, and significant neurological deficits are common in surviving patients.
Acute form
An acute epidural hematoma can develop in three ways. There is a bright interval:
- pronounced;
- poorly expressed;
- completely absent.
Most often, the latter option occurs when extensive injuries occur, which cause severe brain damage. In this case, the patient may fall into a coma. As a rule, no positive dynamics are observed. In the acute form, when there is no light gap, there is a high probability of death.