general description
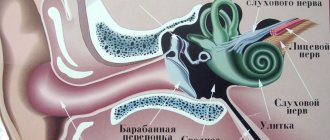
When pork tapeworm eggs enter the stomach, oncospheres emerge from them, penetrate through the intestinal mucosa and migrate with the bloodstream into the subcutaneous tissue, muscles, and internal organs, but mainly into the brain and eyes, where cysticerci subsequently develop. They are bubbles ranging in size from millet grains to 1.5 cm, filled with liquid in which the scolex is located. When the brain is damaged, cysticerci are often localized in the cerebral hemispheres, the base of the brain, but more often in the 4th ventricle. With this variant of the invasive process, the disease is called cysticercosis.
Diagnostics
The basis for diagnosis is solely the results of laboratory tests, and only then the clinical picture. Cerebrospinal fluid is collected as a material for laboratory testing using lumbar puncture. If parasites have settled in the body, then a high content of leukocytes and eosinophils, elevated protein levels, and even cysticercus particles are recorded in the biological fluid. The patient's blood is taken for a general clinical analysis.
To get a reliable picture, X-rays of the brain, computed tomography and nuclear magnetic resonance are performed.
Cynic painting
Manifestations of cysticercosis are determined by the intensity of invasion and localization of the cyst. When the brain is damaged, hypertension syndrome, severe headaches, persistent vomiting, convulsions, mental disorders, and bradycardia appear. With massive infection, symptoms of meningoencephalitis, epilepsy, brain tumors develop, and sudden death is possible. With cysticercosis of the eye, the larvae are often located in the vitreous body, the anterior chamber of the eye, causing the appearance of “sparks” and “grids” in the eyes, decreased vision up to complete blindness, and the development of conjunctivitis, uveitis and retinitis. When cysticerci enter the myocardium in the area of the conduction system, disturbances in the rhythm and conduction of the heart occur.
Symptoms of the disease
The parasite has a toxic effect on the nervous system and causes inflammatory processes in the tissues and membranes of the brain.
The larvae pose a danger even after their death: when they die, they form calcified islands, which become the cause of a persistent inflammatory process in the body.
Cysticercosis causes disorders such as cerebral edema , hydrocephalus (due to increased secretion of cerebrospinal fluid), blockage of channels between parts of the brain, and reactive arachnoiditis.
It is believed that the main cause of acquired epilepsy in the world is cysticercosis, which affects 2 to 4% of the world's population.
The disease does not have pronounced symptoms. Characteristics of nerve irritation are mainly observed, but complete neuronal death is extremely rare.
In addition, the disease is different:
- shallow paresis;
- small areas of sensory impairment;
- speech disorders;
- beginning epileptic seizures;
- mental changes, neurotic syndrome.
In severe cases, agitation, depression, hallucinatory-delusional states are observed, and status epilepticus can be established.
Epileptic seizures that appear for the first time serve as a reason to suspect the presence of pork tapeworm infection.
In some cases, headaches appear, accompanied by dizziness and vomiting. They are caused by increased intracranial pressure or cerebral edema.
If the larvae infect the fourth ventricle of the brain, signs of Bruns syndrome begin: severe and sharp headaches, vomiting, forced head position, difficulty breathing, palpitations. Increased symptoms lead to loss of consciousness.
When the lateral ventricles are affected by cysticercomas, when the interventricular canal is blocked, symptoms of a tumor of the frontal lobes of the brain appear with periodic loss of consciousness. When the channels are freed, the symptoms go away.
When the base of the brain is affected, a picture of basal meningitis appears with headaches, vomiting, heart rhythm disturbances, damage to the optic nerves and partial paralysis of the cranial nerves.
Cysticercosis can cause severe damage to the spinal cord.
The disease has a long course, alternating periods of severe exacerbation and long (sometimes up to several years) remission. The disease cannot go away on its own.
Treatment of cysticercosis
For cysticercosis of the brain and eyes, treatment is only surgical.
For the purpose of prevention, comprehensive medical and veterinary measures are carried out aimed at treating infested individuals, strict control over pork carcasses in slaughterhouses, maintaining personal and public hygiene, and sanitary education among the population.
Essential drugs
There are contraindications. Specialist consultation is required.
- Praziquantel (anthelmintic). Dosage regimen: orally, at a dose of 5 mg/kg once. For neurocysticercosis: at a dose of 20 mg/kg orally once a day for 14 days.
- Albendazole (anthelmintic). Dosage regimen: orally, for patients weighing 60 kg or more, 400 mg 2 times a day; for patients weighing less than 60 kg, the dose is set at the rate of 15 mg/kg/day, divided into 2 doses; maximum daily dose - 800 mg; The course of treatment for neurocysticercosis is 8-30 days.
- Niclosamide (anthelmintic). Dosage regimen: orally, chew, 1.0 g (2 tablets), after an hour - another 2 tablets. (total 2 g).
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| Head of the Department of Infectious Diseases, I.M. Sechenov Moscow Medical Academy, Doctor of Medical Sciences, Professor N.A. Malyshev, Moscow. |
Therapeutic measures
To prescribe effective treatment for neurocysticercosis, it is important not only to evaluate all the symptoms, but also to obtain accurate information about the number of larvae, their viability and location, as well as the resistance of the patient’s immune system to helminths. Treatment is selected individually for each clinical case and is carried out comprehensively:
- medications are prescribed to eliminate the symptoms of the disease;
- anthelmintic therapy is carried out;
- if necessary, lesions are removed surgically;
- ventricular shunts are applied.
After making a diagnosis, the doctor prescribes medications to eliminate the symptoms of the disease.
Therapy for parenchymal neurocysticercosis
- For a single lesion, treatment is carried out with Albendazole at a dosage of 100 mg per kilogram of weight. The duration of therapy is three days.
- If the degree of infection is moderate, treatment is carried out with Praziquantel in a similar dosage. The duration of therapy is seven days. If side effects occur, steroids are prescribed as a concomitant drug.
- In case of severe infection (when the number of larvae is more than one hundred), Albendazole is prescribed at a dosage of 15 mg per kilogram of weight (this is the daily dosage). The course of therapy is a week. In parallel, treatment with steroids is carried out.
If colloid cysts are found, treatment is carried out as follows:
- if the affected areas are single, treatment with anthelmintic drugs is not carried out;
- for moderate infection, treatment is carried out with Albendazole for one week at a dosage of 15 mg per kilogram of weight;
- in case of severe infection, steroids are prescribed in significant dosages in combination with osmodiuretics.
For parenchymal neurocysticercosis, treatment is carried out with Albendazole at a dosage of 100 mg per kilogram of weight.
Therapy for extraparenchymal neurocysticercosis
- If cystic cysts are detected, Albendazole is prescribed at a dosage of 15 mg per kilogram of weight, while the patient takes steroids in parallel. The course of therapy is one month.
- If a patient develops arachnoiditis or angiitis, the doctor prescribes steroids in large dosages. The course of therapy is long and supervised by a specialist. With this diagnosis, there is no need to prescribe special antiparasitic drugs.
- For hydrocephalus, no medications are prescribed; a ventricular shunt is applied.
Therapy for ventricular neurocysticercosis
- Ventricular cysts are removed surgically. As for anthelmintic drugs, they are prescribed at the discretion of the specialist.
- For ependymitis, anthelmintic medications are not prescribed. If the pathology is accompanied by hydrocephalus, a ventricular shunt is required and steroids are prescribed in parallel in high dosages.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0.5 | 3 | 5 | 5 | 5 | 5 | 5 | 0.5 | 3 | 5 | 5 | 5 | 5 | 5 |
Diagnosis of the disease
When a patient with signs of pathology comes for an appointment, the doctor collects an anamnesis, finds out complaints, symptoms of characteristic forms of the disease, the presence of taeniasis, and clarifies the rules of personal hygiene. Diagnostics include:
- blood test for eosinophils;
- electroencephalography;
- chest x-ray;
- cerebrospinal fluid analysis;
- serological method of blood testing to detect antibodies to cysticerci;
- ophthalmoscopy;
- computed tomography;
- histological examination of affected tissues.
- Non-surgical nose correction: methods
- What is a bank deposit? Interest rates, opening conditions and types of deposit accounts for individuals
- How to open dwg format
Symptoms
The development of cysticercosis in humans is indicated by such signs as:
- increased emotional irritability;
- alternation of nervous excitability with prolonged periods of apathy;
- poor sensitivity;
- the occurrence of convulsive conditions reminiscent of epileptic seizures;
- in rare cases, hallucinations and loss of orientation in space are observed.
Based on the location of the parasite larvae, a number of additional symptoms may occur:
- Large hemispheres of the brain – migraine attacks, nausea, vomiting. Floating neoplasms in the form of bubbles interfere with healthy metabolism and the free outflow of fluids, which leads to an increase in intracranial pressure.
- Fourth ventricle of the brain - headaches and attacks of nausea are accompanied by disruptions in the functioning of the heart and respiratory organs.
- Base of the brain – blurred vision, partial hearing loss, pain in the back of the head, failure of certain parts of the body.
- Mixed localization - severe convulsive states, mental disorders, hallucinations, delusions.
Etiology of cysticercosis
The worm is completely white, the length of its flat body is 2-3 meters. There are individuals 8 m long. The size of the scolex is several mm. Weapons:
- Four symmetrically located side suction cups.
- The anterior proboscis is crowned with two rows of hooks.
The neck is followed by a strobila, which includes up to 900 segments. The first proglottids are small, short, asexual. As you move away from the cervix, male organs appear, and later - female ones. The reproductive system of a hermaphrodite is strikingly complex:
- The male organs are many round testes with tubules flowing into the copulatory organ.
- Female organs are branched ovaries containing vitelline, consisting of three lobules. Between them lies the body of Melis, the ootype and the uterus.
Fertilized eggs mature. The development of the worm embryo begins right in the uterus. As the number of eggs increases, its size increases. Gradually, the uterus becomes the main component of the proglottid. Mature members leave the worm, being thrown out in feces. The appearance of the proglottids is quite sufficient to make a diagnosis.
Mature eggs contain an embryo, posing a threat to all living things. Including the owner of the worm. The oncosphere with a diameter of 31-38 microns is surrounded by a dense shell that is dissolved by gastric juice. The larva will choose the muscles or brain, where it will shed its hooks, becoming a fin (cysticercus).
Treatment principle
Parasitic invasion of the eyes and brain is treated only on an inpatient basis, with mandatory hospitalization of the patient . In other cases, outpatient monitoring of the patient is sufficient. Therapy for cysticercosis is long-term, lasting several months. To combat helminths, the course of treatment is selected individually, depending on the severity of the condition and the clinical complexity of the disease.
In medical practice, there are three anti-invasive techniques:
- Conservative or antiparasitic. Antihelmintic drugs are prescribed (Mebendazole, Albendazole, Praziquantel). Treatment is carried out with extreme caution due to the risk of developing a severe allergic reaction (anaphylactic shock) and only under the supervision of a doctor. The course of therapy is gradual, with periodic 3-week intervals.
- Surgical. They resort to it if a source of invasion is identified and it can be eliminated without threatening the vital centers of the brain. If necessary, treatment can be supplemented with conservative therapy.
- Symptomatic. It is an auxiliary course to achieve greater effectiveness of the main treatment. Provides for the use of antihistamines, anticonvulsants, dehydration, sedatives and other medications.
After completing the course of treatment, the patient must undergo control tests to establish the effectiveness of the chosen therapy and the actual results in removing helminths from the body.
Provoking factors
The cause of cysticercosis of the brain, as well as other organs, can be:
- Failure to comply with personal hygiene rules;
- Growing food in soil fertilized with feces infected with tapeworm eggs;
- Ignoring laboratory standards for analyzing contaminated stool;
- Eating meat inseminated with helminth larvae;
- Poorly washed and processed food;
- Tactile contact with a sick person.
Only a laboratory assistant can determine the presence of helminthiasis in a person, animal or product. The specificity of the manifestation of cysticercosis is such that the parasite does not immediately detect its presence in the body and, moreover, it is not visible to the naked eye on the surface of an infected vegetable or fruit.
Complications
With timely and adequate treatment, the dynamics of healing of cysticercosis is positive. But in case of ineffective therapy or in severe advanced situations, the disease has adverse consequences for the health and life of the patient.
Recovery from helminth infestation occurs only with a single or minimal insemination by pork tapeworm larvae. However, with multiple infections by tapeworm eggs, death is inevitable.
Other, no less dangerous complications of cysticercosis are:
- Basal meningitis;
- Neoplasms, for example, ependymoma (blockage of the foramen of Monroe);
- Palsy of the 6th and 7th cranial nerves;
- Eye diseases and loss of vision, including blindness;
- Mental disorders - depression, dementia, hallucinations, etc.;
- Epilepsy.
In comparison with other forms of Finnosis, the prognosis for parasite infection of the central nervous system and vision is always negative. Death can occur suddenly, during another epileptic attack or exacerbation of occlusive hydrocephalus (hydrosis of the brain).
Cysticercosis of the spinal cord
The larvae of parasites enter the spinal cord most often from the brain, but can also directly from the stomach or intestines, and settle on the roots, membranes or in the medulla itself. This is also quite severe cysticercosis, the symptoms of which are as follows:
- pain in the legs, arms, back;
- girdle pain in the abdomen and chest;
- movement dysfunctions;
- in severe cases, paralysis.
This all happens because the larvae cause adhesions on the roots and membranes, as well as the formation of cysts. Compression of the spinal cord cannot be ruled out.
Diagnosis is carried out using a serological reaction, MRI, and myelography.
There is no specific treatment.
Pathogenesis and symptoms of cysticercosis
The disease begins from the moment the cysticercus enters the stomach and/or intestines of the victim. There, gastric juice dissolves the larval shell. The previously depressed head protrudes outward. It already has a corolla with hooks and suction cups that help attach to the walls of the digestive organs, and then leak through them into the blood. Then the larvae spread throughout the body, settling in the lungs, eyes, heart, brain and spinal cord, and skin. Symptoms and treatment of cysticercosis depend on which organ the parasites choose as their place of residence. As they develop, they increase in size and put pressure on neighboring cells, causing significant pain to the owner. Their waste products poison humans. But the death of a worm brings little good. The body of the parasite can dissolve (leasing occurs). This releases particularly dangerous substances, often leading to allergic shock, 20% of cases of which result in death. Sometimes the dead worm becomes calcified (calcified), but the inflammatory processes in the affected organs of the victim continue.
Likely consequences
Positive prognoses for returning to a healthy life after infection with pork tapeworm depend on the extent of damage to body tissue by helminths. As a rule, with significant invasions of the areas of the brain that are responsible for the functioning of the organs of vision and hearing, a partial deterioration in their functioning is observed. Patients who have been exposed to such parasite infections require long-term treatment and need follow-up by a doctor. Often the body’s recovery occurs throughout life.
A lethal outcome with cysticercosis of the brain can occur only due to the development of convulsive conditions, epileptic seizures, as well as the accumulation of copious amounts of fluid under the skull.
The consequence of an advanced disease is a decrease in a person’s ability to work and general activity. The trouble is due to the fact that the course of the disease is often accompanied by an increase in intracranial pressure. Against the background of the pathological phenomenon, chronic migraine attacks are formed, and the patient’s psyche suffers.
Methods for diagnosing cysticercosis
Several successive steps will help diagnose the disease:
- examination, data collection, taking into account answers to questions about personal hygiene;
- clarification of patient complaints;
- specific test for cysticercosis;
- conducting electroencephalography, radiography, ophthalmoscopy, CT, MRI;
- diagnostic biopsy to detect neoplasms, to study the material taken and to possibly identify larvae;
- conducting a serological blood test to detect pork tapeworm antibodies.
Neurocysticercosis requires differential diagnosis with tuberculosis, phlebitis, toxoplasmosis, brain tumors, and neurosyphilis.
Cysticercosis during pregnancy
In other organs, such as the heart and kidneys, it is extremely rare that cysticercosis, or pork tapeworm, can also appear. Symptoms and treatment depend on the location. Thus, when the heart is damaged, the patient experiences disturbances in heart rhythms. A small number of people affected may develop heart failure.
The disease cysticercosis during pregnancy is very dangerous, since the larvae of pork tapeworm are able to penetrate the placenta to the fetus. In such cases, the child is born dead or with significant abnormalities. In addition, the uterus (cervix, mucous membrane) is affected by cysticerci. As a complication, inflammation of the appendages occurs. If the larvae choose the placenta as their place of residence, spontaneous abortion may occur. Treatment of pork tapeworm in pregnant women is complicated by possible side effects that occur when the parasites die. Doctors often recommend terminating a pregnancy if cysticercosis of the brain, spinal cord, eyes, uterus or placenta is detected in the early stages. If the disease is detected late, the decision is made by the attending physician.
Pulmonary cysticercosis. Symptoms, signs, treatment
Cysticerci settle in the lungs even less often than in the skin, but they also cause a lot of unpleasant moments. The largest number of them is collected in the interstitial (interstitial) tissue, less often in the peribronchial tissue. Then they grow, compress the lumen and cause inflammation. The size of the larvae in the lungs reaches 2 cm. A special capsule is formed around each one. This process is accompanied by an inflammatory reaction with symptoms of pneumonia. When the parasite dies, it either dissolves or calcifies. The lungs are deformed. With an x-ray, you can see these changes, as well as foci of parasites, similar to shadow spots, ranging in size from a grain to a cherry. As a rule, there are no pronounced symptoms. The patient may complain of:
- cough (sometimes with sputum or streaks of blood);
- shortness of breath after exercise;
- low temperature;
- moderate pain in the chest.
Diagnosis includes x-rays, stool analysis for helminths, and a specific blood test for the presence of eosinophils.
Treatment is very rare and for isolated lesions it is performed surgically. In most cases, a course of taking Mebendazole or Parasiquantel is prescribed.
Cysticercosis pisiformis
Content
Cysticercosis of farm and domestic animals…………………………….……………………………………………………….3
Cysticercosis pisiformis….………………………………………………………………………………6
List of references……………………………………………………….9
Cysticercosis of farm and domestic animals
CYSTICERCOSES (Cysticercoses), finnoses, helminthiases, many others. species of animals and humans, caused by larvae (cysticerci, or finns) of cestodes of the family Taeniidae, class Cestoda.
Cysticercosis in cattle (bovine), as well as in zebu, yak and buffalo (intermediate hosts), is caused by Cysticercus bovis (bovine cysticercus), the larval stage of the bovine tapeworm Taeniarhynchus saginatus, which parasitizes the human intestine (definitive host).
Cysticercus is a transparent vesicle the size of a pea or more, inside of which there is a scolex (Fig. 1) with 4 suckers without hooks. In the human intestine, the tapeworm (length 3-10 m, lives 15 years or more) separates segments containing more than 100 thousand eggs each (up to 1 million eggs are released per day). In the external environment, eggs (Fig. 2) retain invasive properties for up to 18 months. The route of infection of animals is nutritional. The embryos (oncospheres) emerging from the eggs in the body of the intermediate host penetrate into the blood, and then into the muscles (including the heart), liver and other organs, where they grow and turn into invasive cysticerci.
Cellulose cysticercosis of pigs, wild boars, and less commonly dogs, camels and other animals (intermediate hosts). The causative agent C. cellulosae is the larva of the armed tapeworm (pork tapeworm) Taenia solium, which lives in the human intestine (definitive or intermediate host). Cysticercus up to 20 mm long, with a scolex inside, 4 suckers and a proboscis with hooks. The biology of the pathogen and the epizootology of the disease are basically the same as for bovis cysticercosis. The development of the helminth occurs with the participation of humans and pigs (intermediate host); In the mechanism of transmission of the pathogen to pigs, coprophagy is of decisive importance. Cellulose cysticerci (unlike bovis) also settle in the brain and spinal cord, in the eyes and subcutaneous tissue.
Cysticercosis tenuicollis of sheep, pigs, camels, goats, horses, deer, other wild ruminants, less often cattle is caused by C. tenuicollis - the larval stage of the cestode Taenia hydatigena, parasitizing in the intestines of dogs, wolves, foxes and other carnivores (length up to 5 m). Cysticerci, ranging in size from a pea to a chicken egg, are localized in the liver and on the serous integument (usually on the mesentery), hanging in the form of clusters. The route of infection is nutritional (ingestion of helminth eggs scattered by dogs in excrement with food and water). Dogs and other definitive hosts become infected by eating the organs of killed or dead sheep and other herbivores affected by tenuicol cysticerci.
Ovis cysticercosis of sheep, goats, camels and goitered gazelles. The causative agent of C. ovis is the larva of the cestode T. ovis, which parasitizes the intestines of dogs, foxes and jackals (length up to 1 m). Cysticercus is a vesicle 2-9 mm in size, contains a scolex armed with hooks, is localized in the intermuscular connective tissue (heart and other muscles), in the liver, lungs and other organs. The development and mechanisms of transmission of the pathogen are the same as with tenuicol cysticercosis.
Cysticercosis tarandus and parenchymatous of reindeer (less commonly other species), elk, roe deer and sheep are caused by C. tarandi, which affects skeletal muscles and the heart, and C. parenchymatosa, localized in the liver, less often in the heart, skeletal muscles and abdominal cavity. The corresponding imaginal forms of cestodes T. crabbei (up to 2 m long) and T. parenchymatosa (up to 100 cm long) parasitize the intestines of dogs, arctic foxes, wolves, coyotes, and lynxes (definitive hosts). Cysticerci tarandus and parenchymatous are morphologically similar to each other. Their sizes range from 7 to 10.5 mm. The biology of the pathogen and the epizootology of the disease are the same as for tenuicolosis cysticercosis.
Cysticercosis pisiformis of rabbits and hares. The causative agent C. pisifbrmis is the larva of the cestode T. pisiformis, which parasitizes the intestines of dogs, foxes, cats, and jackals (definitive hosts). Cysticerci (length -12 mm) are localized on the serous covers of the abdominal and, less commonly, thoracic cavities. The biology of the pathogen and the epizootology of the disease are the same as for other cysticercosis transmitted through dogs.
Human cysticercosis (finnosis). Caused by pork tapeworm larvae. Infection occurs when pork tapeworm eggs are ingested in food and water contaminated with the feces of a human infected with pork tapeworm. It may be a complication of intestinal taeniasis, in which mature segments of the helminth are thrown into the stomach during antiperistalsis of the intestines. Cysticerci are most often localized in the brain and spinal cord, under the skin, in the eyes and muscles. Depending on the location of the larvae, it manifests itself as headaches, sometimes convulsions, mental disorders, muscle pain, and eye damage. Prevention: veterinary and sanitary control of pork carcasses, routine identification and treatment of patients, health education.
Cysticercosis pisiformis
Pisiform cysticercosis of rabbits and hares is caused by tapeworm larvae of the family Taeniidae, suborder Taeniata.
Larvae in the vesicular stage are localized in hares, rabbits and rodents on the mesenteric omentum, on the serous integument of the abdominal cavity, and around the outside of the colon at the entrance to the pelvic cavity. Tapeworms parasitize dogs and other carnivores in the small intestine.
Pathogen.
Cysticercus pisiformis - oval-shaped blisters, 6-12 mm long, 4-6 mm wide. Inside the bladder there is a clear liquid, through which the scolex shines through in the form of a spot the size of a millet grain. Taenia pisiformis in the ribbon stage is up to 2 m long, the scolex is armed with 36-48 hooks arranged in two rows. The posterior edge of each segment is wider than the anterior edge, as a result of which the strobile resembles a saw with its lateral edges. Mature segments contain a uterus filled with almost round eggs, measuring (0.036...0.04) x (0.032...0.037) mm.
Developmental biology.
T. pisiformis is a biohelminth that develops with the participation of definitive (dog, wolf, fox, arctic fox, cat) and intermediate (rabbit, hare, sand hare) hosts. Squirrels, house mice, rats (red and black), guinea pigs, monkeys, etc. have also been identified as intermediate hosts. The cestode secretes segments and eggs, which are ingested with food and water by the intermediate hosts. From the intestines of rabbits and other rodents, oncospheres with the bloodstream mainly enter the liver, where, destroying capillaries, migrate through the parenchyma to the outer layers of the liver, and then, destroying the organ capsule, exit into the abdominal cavity. Then they attach to the omentum and mesentery, develop into a vesicular form, reaching the invasive stage approximately on the 45th day. Definitive hosts become infected by eating the internal organs of infected rodents. In the intestines of dogs, the cestode develops to the sexually mature stage on the 35th day, in foxes - on the 70th day.
Epizootological data.
Pisiform cysticercosis is almost universally distributed in the Russian Federation and neighboring countries. In the Stavropol Territory, during autopsy of 196 hares, pisiform cysticerci were found in 96.4%. In the northern and northeastern regions of the European part of the Russian Federation, white hares are infected up to 24%, in Tatarstan - 39%, in Buryatia - 25%, etc.
Sources of spread of the invasion are dogs and other carnivores, both domestic and wild.
At the same time, hunting dogs play a significant role in the spread of invasion. In the Tver region, out of 34 dogs, 19 (55.88%) were infected with T. pisiformis.
The intensity of infestation in rabbits and hares ranges from one to 613 blisters.
Pathogenesis and immunity.
The pathogenic effect of the larvae on the body of rabbits is due to the nature of the development of the parasite in the body of the intermediate host. In general, the development of pathological processes during this invasion is similar to those with tenuicol cysticercosis in sheep.
In the first 5 days, oncospheres migrate from the intestine, damaging the corresponding tissues and vessels in the liver parenchyma. In the second phase of development, the larvae migrate intensively in the liver parenchyma, damaging the liver tissue. There is an increase in leukocytes and eosinophils in the blood, a decrease in the number of red blood cells, and a decrease in hemoglobin levels. This period lasts from 6 to 13 days. The third phase lasts about 20 days and is characterized by the most severe pathological phenomena. Larvae of sufficiently large size, lysing the surrounding liver tissue, enter the abdominal cavity en masse, causing serous-hemorrhagic and sometimes purulent peritonitis.
The fourth and fifth phases are characterized by the extinction of acute phenomena and the settlement of larvae in the abdominal (sometimes also in the thoracic) cavity. The larvae mature in the places where they are localized, are isolated by connective tissue, and the process becomes chronic. Allergic and toxic phenomena develop in the body, protein metabolism is sharply disrupted: the content of total protein, albumins, alpha globulins decreases, and the content of gamma globulins increases.
Symptoms of the disease.
In sick rabbits, their appetite worsens, they often lie down, arch their backs, palpation reveals an enlarged liver, it is hardened and painful, the mucous membranes of the eyes and mouth are anemic. After 1.5 months from the onset of infection, rabbits are significantly retarded in growth and development compared to healthy ones. The death of rabbits is most often observed in the period from 13 to 23 days after infection.
Pathological changes.
In dead rabbits with high AI, the liver is enlarged and has a dark cherry color. Already on the 10th day after infection, a large number of cysticerculi under the capsule are visible. The surface of the liver is covered with tortuous hemorrhagic ducts ending in dark red cavities. Serous-fibrinous peritonitis is often observed, as a result of which the entire omentum is knocked into a compact mass. In the late stage of development of the invasion, cysticercuses are found in large numbers around the colon at the entrance to the pelvic cavity.
Diagnostics.
Diagnosis of cysticercosis pisiformis during life has not been developed. One can only suspect the disease based on clinical signs and further diagnose it by examining dog feces using the method of successive washes and detecting segments of the parasite.
Posthumous diagnosis is made on the basis of autopsy of animals and detection of corresponding pathological changes in the liver and cysticercus.
Treatment.
It is recommended for chemotherapy of cysticercosis pisiformis in rabbits to use mebendazole by group or individual feeding with food at a rate of 25 mg/kg for 3 or 5 days with an interval of two days.
Prevention and control measures.
In rabbit farms unaffected by cysticercosis, mebendazole should be given with food for prophylactic purposes according to the above scheme and dose.
It is strictly prohibited to feed the internal organs of hares to hunting dogs. In rabbit farms and private farms, affected organs of rabbits must be disposed of in accordance with veterinary legislation. Keep dogs and cats away from areas where rabbits are kept. Systematically examine carnivores and, if necessary, deworm them.
Cestodosis, caused by the imaginal stage of the cestode Cittotaenia denticulata of the Anoplocephalidae family, also occurs in rabbits and hares.
Tapeworms 40-50 cm long are localized in the posterior part of the small intestine. The scolex of the cestode is not armed, the genitals are double. Cirrus is armed with small spines. In the hermaphroditic segment, the uterus is reticulate and occupies the entire width of the segment. The diameter of the egg is 0.054-0.07 mm, the oncosserra is equipped with a fouche-like apparatus, the horns turn into thin processes. Developmental biology involves oribatid mites.
Diagnosis of animal infestation is made by detecting segments or eggs in feces using the sequential washing or Fulleborn method. Posthumous diagnosis is made on the basis of opening the intestine and finding cestodes in it.
During treatment, it is recommended to give fenasal to rabbits at a dose of 0.1 g/kg individually or in a group method with food. Bithionol is given in a dose of 0.2 g/kg individually orally once.
It is probably possible to use fenbendazole, phenalidone and other drugs used for moniesiosis in ruminants.
Preventive control measures consist of breaking contact between rabbits and intermediate hosts. Helminthocoprological studies should be periodically carried out and, if necessary, deworming should be prescribed. After deworming, feces are removed to a manure storage facility.
In rabbits and hares, tetrathyridia can be found in the liver - the larvae of the tapeworm Mescestoid.es lineatus are elongated, 5 to 7 mm long. The anterior end of the larva is widened, containing a scolex inside, but without a proboscis and hooks; the posterior end is slightly thinned. For the purpose of prevention, you should not feed rabbits with hay from under haystacks, where oribatid mites, the intermediate hosts of the helminth, often live. Grass should be mowed in sunny weather from cultivated pastures and hayfields.
List of used literature
Parasitology and invasive animal diseases / M. Sh. Akbaev, A. A. Vodyanov, N. E. Kosminkov and others; edited by M. Sh. Akbaeva. - M.: Kolos, 1998. - 743 p.: ill. — (Textbooks and teaching aids for students of higher educational institutions).
Leikina E. S., The most important helminthiases of humans, [3rd ed.], M., 1967; Parasitology and invasive diseases of agriculture. animals, ed. K. I. Abuladze, M., 1975;
Treatment of calves infected with bovis cysticerci, “Veterinary Medicine”, 1980, No. 3, p. 40-42.