Trunk stroke is a pathology that reflects damage to the nervous tissue in the trunk area. This is an emergency condition that requires immediate hospitalization. A stroke is often called a stroke because it develops suddenly against the background of apparent relative well-being, leading to progressive neurological deficits up to coma and death.
Causes of brain stem stroke
Most often, the disease affects older people with high blood pressure, atherosclerosis, increased blood clotting activity, as well as those suffering from inflammatory vascular diseases, autoimmune or tumor processes.
Atherosclerosis is one of the common causes of brainstem stroke
At a young age, the cause may be:
- vascular malformation,
- arterial aneurysm,
- heart defects,
- rheumatic endocarditis,
- atrial fibrillation,
- diabetes,
- long-term use of anticoagulants.
We recommend reading the article about stroke in young people. From it you will learn about the causes of pathology in young people, symptoms of hemorrhagic and ischemic stroke, diagnosis and treatment, consequences and preventive measures.
And here is more information about cerebral vascular thrombosis.
First aid for bleeding in the brain stem
First aid is provided to the patient after symptoms occur. It is very important to recognize a brain stem stroke in time so as not to harm the person during the most dangerous period. The following actions are carried out:
- The patient should be placed in a horizontal position with his head raised.
- Free your neck from clothing and accessories.
- Remove dentures from your mouth.
- Create conditions for maximum fresh air supply.
- If the state is unconscious, then the head should be turned to the side to allow saliva to flow out.
- The oral cavity must be cleared of vomit.
- Apply cold to your head. Exposure to the part of the brain that is the opposite side of the paralysis of the limbs.
- Cover the patient with a blanket.
- Monitor respiratory parameters, heart rate and blood pressure.
- If there are signs of clinical death, perform resuscitation measures.
Find out more about the symptoms of the disease and first aid rules:
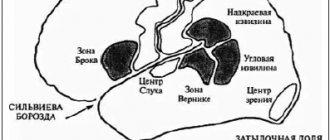
What happens during pathology
The peculiarity of a stroke is associated with the anatomical structure and location of this part of the brain. The stem part is located near the base of the skull, namely the foramen magnum. When swelling (heart attack, ischemic stroke) or hematoma (hemorrhage, hemorrhagic) occurs, tissue wedging may occur with irreversible destruction of the centers of respiration and regulation of vascular tone, which is a fatal complication.
With a more favorable course, there is a disruption of the processes controlled by the medulla oblongata, midbrain, pons and cerebellum. These include:
- heartbeat,
- movements,
- muscle tone,
- cough,
- sneezing,
- speech,
- swallowing,
- blinking,
- vomit,
- vegetative reactions,
- facial expressions,
- vision,
- hearing.
The patient loses the ability to maintain contact with the outside world, but his consciousness remains intact. Therefore, brainstem stroke is called the disease of a “locked person” in a motionless body.
Characteristic
Brainstem stroke (stroke) is a life-threatening condition that is characterized by impaired blood flow in the area of the brain stem, which is associated with impairment of vital functions (respiratory, cardiac activity). There are types: ischemic, hemorrhagic, venous. Ischemic stroke is an acute disruption of the blood supply to an area of the medulla with the subsequent development of hypoxic and necrotic processes.
Hemorrhagic stroke is the formation of a focus of hemorrhage within the medulla, followed by swelling and compression of the nervous tissue. Venous stroke develops as a consequence of blockage of the lumen of the cerebral veins and venous sinuses. The proportion of ischemic strokes is 79%, hemorrhages in the medulla - 16%, hemorrhages in the subarachnoid space - 3%.
Damage to the brainstem is detected in about 20% of cases in the total number of episodes of cerebral blood flow disturbances of various locations. The percentage of ischemic and hemorrhagic strokes in the brainstem area is 75% and 25%. Foci of hemorrhage in the brainstem localization are detected in 3% of cases in the total mass of hemorrhagic strokes, foci of ischemia in the brainstem area - in 20% of cases of all cerebral infarctions.
Brainstem localization of the pathological focus is associated with an increased risk of death compared to hemispheric strokes. The trend is explained by the accumulation of vital centers in the stem section (breathing, swallowing, regulating the functioning of the heart and the condition of the blood vessels). The brain stem includes sections - the oblongata and middle sections, the pons. The cerebellum and an area called the quadrigeminal form the roof of the brainstem.
Mechanical injuries, ischemic damage or intracerebral hemorrhage in the brainstem area within the brain are often accompanied by involvement of surrounding structures and lead to the development of brainstem symptom complexes, which are called alternating syndromes (with manifestations in different directions relative to the location of the focus). Alternating (cross) syndromes are observed when one half of the trunk is damaged.
Symptoms of brainstem stroke
The abundance of nerve centers and conducting nerve fibers lead to many symptoms in this pathology. Initially, there is severe pain in the back of the head, partial or complete loss of consciousness, weakening of strength in the limbs, fluctuations in pulse rate, blood pressure and temperature.
The clinical picture in the acute stage has features of a general cerebral process; it is associated with an increase in intracranial pressure (cephalgia, dizziness, vomiting). Later, manifestations of destruction of the nuclei of the cranial nerves, the nerve pathways that provide movement and sensitivity, occur.
In ischemic stroke, the pathognomonic (characteristic) signs are:
- limb paralysis,
- displacement of the tongue to the side,
- loss of sense of balance,
- chaotic eye movements,
- facial distortion
- drooping upper eyelid,
- difficulty breathing and swallowing due to relaxation of the muscles of the upper palate.
With small-focal brain damage, there are local disturbances in movement and sensitivity of the hand, face, tongue, choking, double vision, hearing loss or loss of balance without other manifestations.
Hemorrhagic stroke is characterized by rapid progression, the appearance of motor and sensory disorders along with loss of consciousness and coma. Symptoms of hemorrhage in the brain stem:
- paresis (paralysis) of half the body,
- weakened vision,
- strabismus,
- slurred speech
- loss of sensation,
- coma,
- dizziness,
- increased body temperature,
- difficulty breathing,
- arrhythmia.
Since the prognosis of a stroke depends entirely on how quickly the diagnosis is made and treatment is started, all cases of unexplained weakness, slurred or incoherent speech, unsteady gait, loss of sensation or loss of muscle tone should be regarded as a probable stroke and an ambulance should be called immediately for the victim .
Watch the video about the types of strokes and their manifestations:
First aid
Stroke damage to the brain after a few hours causes irreversible changes in brain structures - necrosis of a significant number of stem cells.
However, there is a time period for providing medical care to the victim, equal to 3-4 hours, during which the serious consequences of a stroke will be minimal.
Before the ambulance arrives, take the following measures:
- reassure the patient, do not create panic;
- Place the victim in bed so that the head is elevated 30 degrees;
- if the victim has lost consciousness, then turn his head to the side so that he does not choke on saliva, and if he vomits, he does not choke on vomit;
- unfasten belts, buttons, collars to increase oxygen access;
- If possible, measure your blood pressure: if it is high, give medicine to lower it;
- To ensure the outflow of blood from the brain, apply a heating pad to the patient’s feet.
Do not give the victim food, drink or drugs that dilate blood vessels. There is no need to try to deliver the patient to a medical facility on your own: to transport him, you need an ambulance with special medical equipment in order to begin measures to stabilize the patient’s condition even at the pre-hospital stage.
Diagnosis of ischemic, hemorrhagic disorders
The main rules for differential diagnosis are to exclude diseases similar to a stroke, as well as to determine its origin (blockage of a vessel or hemorrhage). The following factors are considered in favor of ischemia:
- gradual onset
- elderly age,
- angina pectoris
- rhythm disturbance,
- heart disease,
- the attack occurred while resting,
- pressure is normal or low.
With hemorrhage, patients before a stroke usually suffer from hypertension with a crisis course, at the very beginning they develop loss of consciousness, deterioration of their condition after physical or emotional stress. Since all these symptoms are relative, an accurate diagnosis will require the following studies:
- Tomography (CT or MRI) shows the focus of ischemia or hematoma, swelling of brain tissue, the degree of displacement of the medulla oblongata, and helps to examine the vessels near the stroke area.
- A spinal puncture is prescribed when tomography is impossible and it is difficult to determine the type of disease. It is not performed when the brain is displaced.
A hemorrhagic stroke occurs with high cerebrospinal fluid pressure, its color is pink, the protein content is increased, and there is an admixture of blood.
- Ultrasound of the vessels of the neck and head confirms spasm or blockage of the artery, makes it possible to assess the possibilities of bypass blood supply, and can detect an aneurysm.
- Angiography is indicated before starting thrombolytic therapy.
- General clinical examination of blood, urine, coagulogram, sugar and lipid profile, as well as pulse oximetry are carried out to select medications.
Diagnostic measures
Symptoms of damage to the brain stem allow the neurologist to predict in advance the location of the damage. Further research is aimed at clarifying:
- there was a brain stem infarction or hemorrhagic hemorrhage;
- what important centers are damaged and the size of the pathological focus;
- tissue became saturated with blood or a hematoma formed (if hemorrhage was detected in the brain stem).
To clarify these data, CT or MRI of the brain is used. Hardware examination provides a complete picture of the size of the lesion and the nature of damage to brain structures.
Treatment of pathology
During the first 7 days, patients are in intensive care or intensive care wards. Monitoring and correction of basic life processes is carried out - blood pressure, body temperature, heart contractions (ECG).
If there is no spontaneous breathing, an endotracheal tube is placed and a ventilator is connected. The need for such actions is associated with the suppression of natural reflexes of coughing and swallowing. The level of respiratory failure is measured using pulse oximetry; if the saturation index decreases, then oxygen supply is increased.
Antihypertensive drugs are prescribed for blood pressure levels above 180/105 mmHg. Art. with initially elevated numbers and 160/95 mm Hg. Art. for those who had normal levels before illness. The decrease should be smooth and moderate, since hypotension enhances ischemic processes.
The following medicines may be used:
- to stabilize blood pressure Captopril, Ebrantil (for hypertension), Dopamine, Dobutamine, Reopoliglucin (for hypotension);
- maintaining normal blood sugar levels - glucose solution or Insulin (depending on the glycemic level);
- prevention of cerebral edema – Mannitol, Magnesium sulfate, Albumin;
- for temperature regulation – Aspirin (for ischemia), Naproxen;
- anticonvulsants – Finlepsin, Depakin;
- for severe nausea - Motinorm, Cerucal;
- antiplatelet agents and anticoagulants - thrombolytics in the first hours (Alteplase), then Heparin with a transition to Warfarin and Aspirin;
- neuroprotectors – Cerebrolysin, Nimotop, Actovegin, Glycine, Somazina.
In the acute period, drugs are administered intravenously or intramuscularly, then tablet forms are prescribed for a long time. The duration of drug therapy for stem strokes is usually at least 1 year.
Etiology
By origin, brainstem stroke occurs:
- ischemic is associated with a lack of blood flow due to blockage (obstruction) of the artery supplying the area;
- hemorrhagic due to rupture of the artery and bleeding from it.
Types of brainstem stroke
The first type is much more common than the second, accounting for 75-80% of all cerebrovascular accidents.
Causes of ischemic stroke
Risk factors for ischemic stroke include old age, high blood pressure, increased cholesterol in the blood, atherosclerosis, smoking, heart disease, and diabetes.
It should be noted that the increase in blood pressure is above 140/90 mm. Hg, relative to normal, doubles the risk of stroke.
All causes of ischemic stroke can be divided into groups:
- Atherothrombotic - ischemia occurs due to a slowly increasing plaque in the area of the vessel. Such a stroke is preceded by symptoms of transient cerebrovascular accident, signs of prolonged “robbing” the brain of oxygen and nutrients: memory loss, absent-mindedness, development of tearfulness or irascibility, and others. More often happens at night or early in the morning.
- Embolic develops suddenly; a sharp and rapid blockage of the afferent artery occurs with an embolus. More often it occurs with heart diseases (atrial fibrillation, defects, artificial valves), which are characterized by the formation of blood clots in the cavities of the heart and their spread through the bloodstream. More often happens during the day, during emotional or physical overload.
- Ischemia may develop with a decrease in blood pressure, when there is insufficient blood flow to the brain. This is a hemodynamic type.
- Lacunar is characterized by damage to small arteries located deep in the brain. It often develops during the day, against the background of high blood pressure. Since small areas are deprived of blood supply, the symptoms are erased, and its prognosis is better than that of others.
- Hemorheological is rare and develops due to increased blood viscosity.
One of the causes of ischemic stroke is high blood pressure
The brain is an organ where chemical processes actively occur, but it does not have its own reserves of nutrients. This means that any reduction in blood flow with oxygen and nutrients quickly affects its function in a negative way. Without a blood supply, a neuron can survive for a maximum of five to eight minutes, after which it dies.
Normally, 50-55 ml of blood flows through 100 g of brain per minute; with a stroke, this figure drops to 10.
After blockage of a vessel, the following is possible: ischemia occurs in the area it fed, neurons die, and their function is lost. But next to it there is another area (ischemic penumbra or penumbra), in which the blood supply has not reached a dangerous minimum. However, the brain cells in it also suffer from ischemia and damage from the decay products of dead neurons. They are viable, but they are also at risk of death, so it is important to start therapy as early as possible. This will reduce the affected area and preserve more brain functions.
Due to the accumulation of breakdown products, edema develops in this area, which compresses adjacent structures, pushing them to the side, further impairing blood flow and functioning.
Anatomy of ischemic stroke
Causes of hemorrhagic stroke
It occurs less frequently, but its symptoms are more severe and the prognosis is worse. Highlight:
- With parenchymal hemorrhage, changes occur in the substance of the brain. This is possible with arterial hypertension, bleeding disorders or weakness of the vascular wall (aneurysm).
- Subarachnoid - bleeding onto the surface of the brain due to pathology of the vessels in the membranes. More often, it is caused by an aneurysm, so it usually affects young, apparently healthy people.
A brainstem stroke develops when there is a lesion in the vertebrobasilar vascular system.
Consequences for the patient
The outcome of a stroke for patients is often pessimistic - the ability to eat, speak, not only walk, but even sit in bed becomes impossible. In severe cases, the trunk part is pinched in the occipital foramen, breathing and heartbeat stop, and convulsions begin. In such cases, the patient's death occurs.
If the acute period has passed, then subsequent infections of the urinary system, lungs, blockage of veins with blood clots and bedsores make recovery difficult. This is due to the forced immobile position of the patient and neurological abnormalities.
At this stage, dangerous complications include sepsis, gastric and intestinal bleeding, ischemia of the heart muscle, and arrhythmia. Due to the instability of gait when the brain stem is damaged, even with a mild course of the disease, falls with bone fractures or other injuries are not excluded.
Signs that are considered unfavorable for recovery:
- pressure does not decrease with intensive treatment or it cannot be increased to normal;
- high body temperature or changes therein;
- persistent paralysis, speech, vision, and swallowing disorders;
- lack of consciousness in the first days after the attack.
Therapeutic measures
Treatment of brainstem stroke can be conservative or surgical. Therapeutic tactics depend on whether a stroke has occurred in the brain stem or hemorrhage, as well as on the nature of the hemorrhage (tissue impregnation or hematoma formation).
Conservative
Brainstem lesions are treated conservatively if brainstem stroke or hemorrhagic impregnation is detected. The patient is placed in intensive care, where he is prescribed:
- diuretics (Mannitol, Lasix) to prevent cerebral edema;
- intensive oxygen therapy (if the patient breathes on his own, then through a nasal catheter, and if respiratory function is impaired, mechanical ventilation is used);
- sedatives (Phenazepam, Relium, etc.);
- muscle relaxants to prevent possible seizures;
- antihypertensive drugs (drugs of this group in small doses to prevent recurrent stroke are prescribed to patients even with normal blood pressure);
- blood-thinning medications (for hemorrhagic impregnation of brain tissue).
At an early stage, damage to the brain stem can cause a recurrent stroke or provoke an increase in the ischemic focus, so therapy is aimed at preventing possible consequences. When the patient’s condition has stabilized, he is transferred to a ward, where rehabilitation begins, allowing the impaired functions to be fully or partially restored.
Operational
Hemorrhage into the brain stem may be accompanied by the formation of large hematomas. The blood clot compresses nearby tissues, aggravating the pathological process.
Hemorrhagic stroke of brain stem cells is treated according to the following scheme:
- craniotomy is performed over the area of the hematoma;
- Blood clots are removed without affecting brain tissue.
In the future, the pathology is treated in the same way as an ischemic stroke or hemorrhagic impregnation - with the help of drugs that prevent possible complications.
The doctor decides how to treat the pathology individually, taking into account the nature and degree of brain damage.
Recovery after brainstem stroke
The rehabilitation period after a stroke of the brainstem is more difficult than with similar pathologies of other localizations. This is due to the fact that there are difficulties in eating; you need to feed pureed food or through a nasogastric tube.
It takes a long time for motor functions and sensitivity of the limbs to be restored; to develop it, you need to use special gymnastics, massage, reflexology, and physiotherapeutic procedures.
Even after the ability to walk, residual neurological deficits and inability to focus the gaze lead to unsteadiness and dizziness, falls and serious injuries. To restore speech, you will need sessions with a speech therapist.
It takes patients at least 1.5 - 2 years to return to their previous life. But most often, complete rehabilitation cannot be achieved, despite the efforts of doctors, relatives and patients.
Consequences of brain stem damage
Trunk stroke is characterized by a high mortality rate. Even if the victim can survive, he will completely or partially lose certain functions. Timely treatment and rehabilitation do not guarantee the restoration of lost skills. The consequences of brainstem stroke depend on the form of the disease, location and extent of brain damage.
Death is caused by stem swelling with pinching of the area under the meninges. This causes heart failure, respiratory blockage, and epileptic seizures. With large-scale tissue damage, urinary tract infections, thrombosis, pneumonia, and bedsores appear. Myocardial infarction, sepsis, and gastric bleeding may develop.
Attention. Patients with mild cerebrovascular accidents who are able to walk often fall and break limbs, which also leads to death.
Swallowing dysfunction
Swallowing problems after a stroke are called dysphagia. The skill is difficult to restore; special techniques are used for this. Initially, the victim is taught the ability to swallow crushed food.
Such a swallowing disorder reduces the effectiveness of the entire rehabilitation program, since the patient receives food using gastrostomy tubes.
Speech disorders
Damage to the brain stem leads to speech impairment, which is accompanied by difficulties with pronunciation and understanding of some words. People begin to speak quietly, indistinctly, inarticulately. This pathological phenomenon has a favorable prognosis.
It is necessary to work with a speech therapist. After completing the course, the patient continues the exercises at home.
Deterioration in limb functionality
A brainstem stroke always leads to impaired motor functions. The patient begins to involuntarily wave and move his arms and legs. This is due to loss of control over the muscular system.
It is possible to restore motor skills only in the first months after the stroke. The more time has passed after the blockade, the worse the prognosis: it will be impossible to regain muscle strength.
Problems with coordination
The phenomena of ischemia and hemorrhage during a brainstem stroke provoke dizziness, which impairs coordination of movements. The painful sign must be eliminated as soon as possible.